Early outcome of endoscopic mitral valve surgery in elderly patients: a high-volume single center experience
- 1Department of Cardiovascular Surgery, University Heart and Vascular Center Hamburg, Hamburg, Germany
- 2Department of Cardiovascular and Thoracic Surgery, University Hospital Augsburg, Augsburg, Germany
Introduction: Despite increasing use of transcatheter approaches, endoscopic mitral valve surgery (MVS) remains an established option for treatment of mitral regurgitation (MR). Nevertheless, as perioperative risk increases with age, outcome of endoscopic MVS in elderly patients is uncertain.
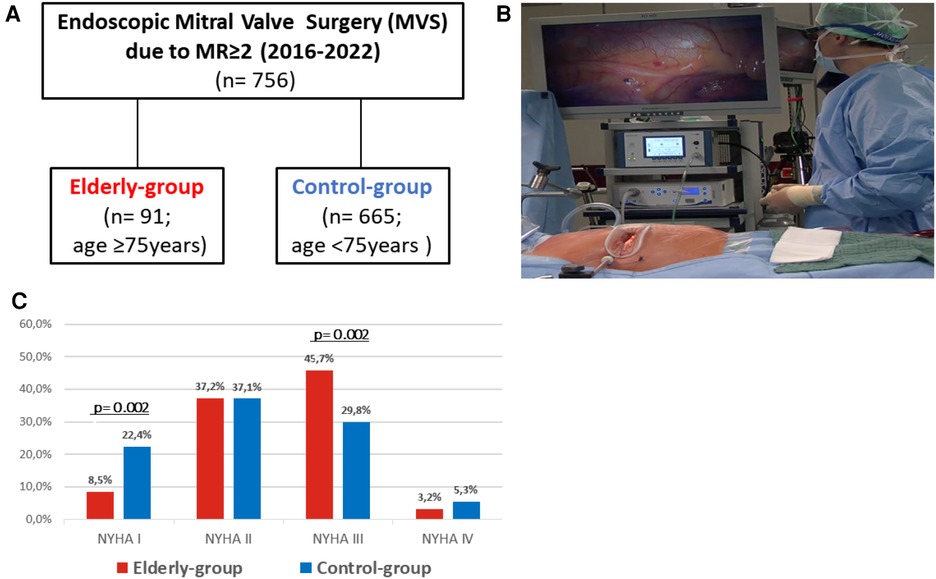
Methods: We retrospectively analyzed 756 consecutive patients with MR ≥2, who underwent minimally-invasive MVS at our institution between 2016 and 2022. Patients were stratified by age ≥75 (elderly-group; n = 91) or <75 years (control-group; n = 665). All patients received endoscopic MVS via right anterolateral minithoracotomy with non-rib spreading soft tissue retraction and 3D-camera visualization.
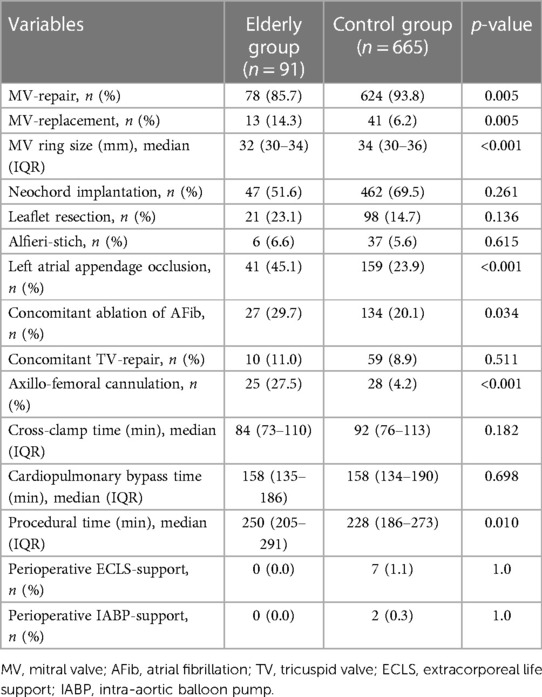
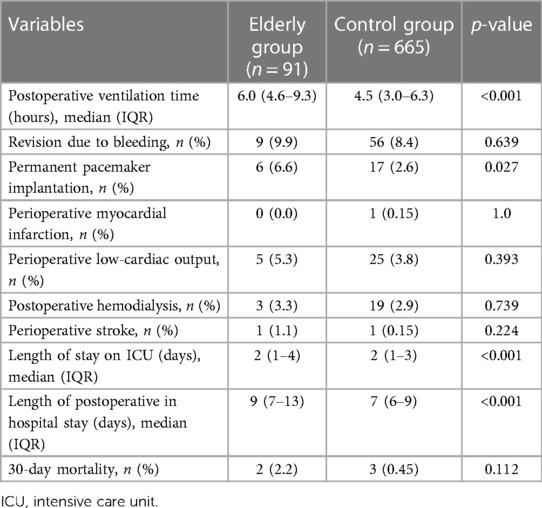
Results: Overall surgical risk was increased in the elderly-group (median age of 77 (76–80) years vs. 58 (51–67) years, p < 0.001) with STS-PROM Scores of 1.9% vs. 0.4% (p < 0.001) and increased prevalence of hypertension, diabetes, coronary artery disease and atrial fibrillation (AFib). Elderly patients were also more symptomatic (NYHA class III 45.7% vs. 29.8%; p = 0.002). Axillo-femoral perfusion was more frequently used in the elderly-group (27.5% vs. 4.2%; p < 0.001). Cross-clamp and cardiopulmonary bypass times were similar. Rate of MV repair was 85.7% vs. 93.8% (p = 0.005). Closure of the left atrial appendage was more frequently performed in the elderly-group (45.1% vs. 23.9%; p < 0.001), whereas rate of concomitant tricuspid valve repair was similar (11.0% vs. 8.9%; p = 0.511). Postoperative complications including perioperative hemodialysis (3.3% vs. 2.9%; p = 0.739), low cardiac output (5.3% vs. 3.8%; p = 0.393), perioperative stroke (1.1% vs. 0.15%; p = 0.224) and myocardial infarction (0% vs. 0.15%) were favorably low in both groups. Acute mortality at 30 days was 2.2% vs. 0.4% (p = 0.112).
Conclusion: Despite increased prevalence of outcome-relevant comorbidities and surgical risk, perioperative outcome of patients aged ≥75 years undergoing endoscopic MVS is favorable. Therefore, endoscopic MVS is a valuable therapeutic option for selected elderly patients and should be taken in consideration during routine heart-team discussion.
Introduction
Prevalence of MR, which represents the second most common type of valvular heart disease (VHD) in Europe, increases with age (1). Moderate to severe MR is present in approximately 8% of the population aged ≥75 years, and about half of cases remain undiagnosed and thus untreated (2), resulting in increased morbidity and mortality. In addition to conventional MVS, which still is the most prevalent strategy to address MR (3), transcatheter mitral valve (MV) technologies developed as a viable treatment option for high-risk (4) and/or elderly patients (5). Despite promising periprocedural results, long-term durability of transcatheter edge-to-edge repair (TEER) remains inferior compared to conventional MVS, in particular in the treatment of primary MR (PMR) (4, 5).
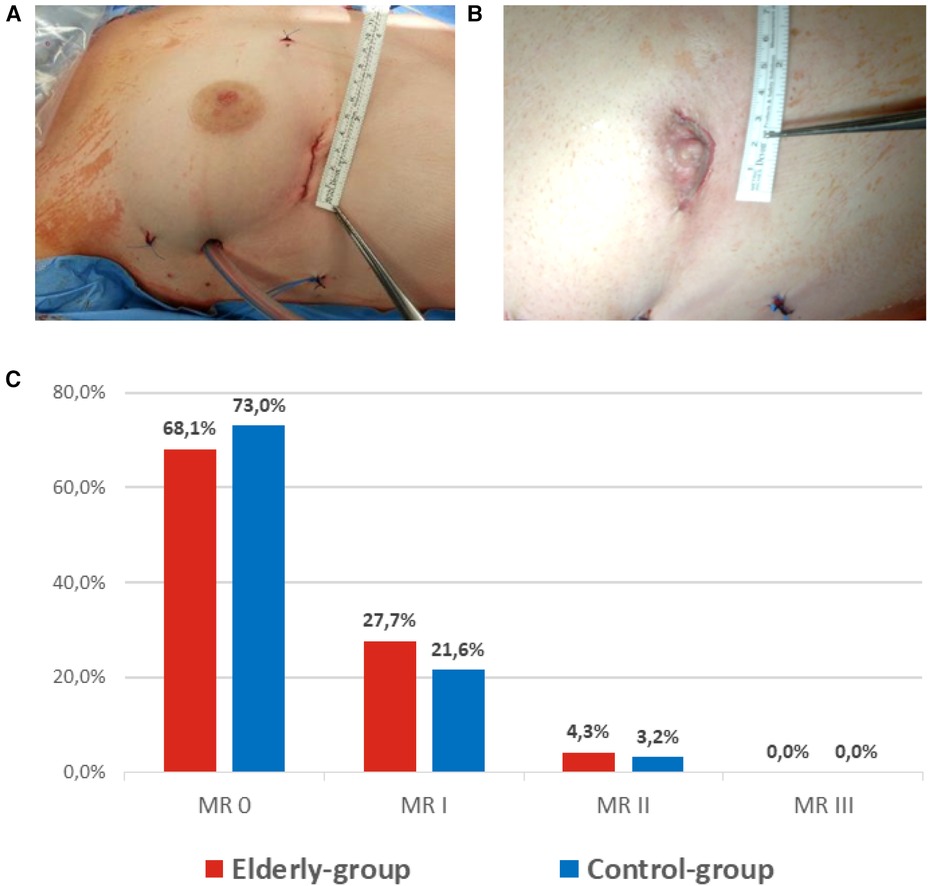
Minimally-invasive MVS via anterolateral mini-thoracotomy evolved as a safe alternative to conventional sternotomy (6), resulting in lower postoperative ventilation times, transfusion rates, shorter stay on intensive care unit (ICU) and shorter in-hospital stay (7). In particular elderly, frail patients may potentially benefit from reduced surgical trauma. Nevertheless, due to an increased prevalence of outcome-relevant comorbidities and elevated perioperative risk (8), outcome of minimally-invasive MVS in elderly patients remains uncertain (9). Therefore, the aim of our study was to analyze perioperative outcome of consecutive patients aged ≥75 years undergoing minimally-invasive endoscopic MVS due to MR≥2 at our institution between 2016 and 2022 (Figure 1A).
Patients and methods
Ethical statement
Due to anonymous data collection and retrospective study-design, informed patient consent was waived according to a statement of our local ethics committee. The study complies with the Declaration of Helsinki.
Patients
We herein report periprocedural outcome of 756 consecutive patients undergoing endoscopic MVS due to relevant MR at our institution between 2016 and 2022. Patients were stratified according to age ≥75 (elderly-group; n = 91) or <75 years (control-group; n = 665) (Figure 1A).
Inclusion criteria
All 756 consecutive patients undergoing endoscopic MVS at our institution between 2016 and 2022, were retrospectively analyzed. Patients receiving MVS via full-sternotomy, mainly due to concomitant CABG or aortic valve surgery were excluded from analysis. Furthermore, patients with severe MV stenosis and acute infective endocarditis were excluded.
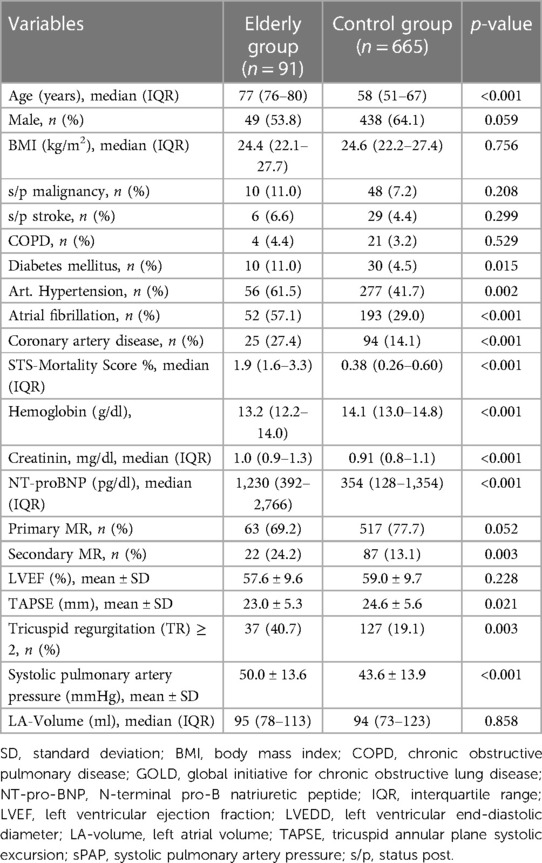
Surgical setup and technique of endoscopic mitral valve surgery
Endoscopic MVS was performed via right anterolateral mini-thoracotomy under 3D endoscopic guidance. A limited skin incision (<4 cm) was used to enter the fourth intercostal space. A non-rib spreading soft tissue retractor was placed to facilitate appropriate surgical access (Figure 1B). Peripheral cardiopulmonary bypass (CPB) was established via percutaneous cannulation of the femoral artery or open direct cannulation of femoral or axillary arteries. Venous cannulation was performed using the right femoral vein either via surgical cut-down and direct visualization or percutaneously. In patients >85 kg or in patients requiring concomitant tricuspid valve repair, a second venous cannula was inserted percutaneously via the right jugular vein to optimize venous drainage during cardiopulmonary bypass (CPB) or to prepare for total bypass. Aortic occlusion was performed using a transthoracic aortic clamp and antegrade cardioplegia was administered via the aortic root. After exposure of the MV using direct left atrial access, standardized intraoperative examination was performed to determine the etiology of MR and define the surgical strategy. At the surgeon`s discretion, MV repair or replacement was performed using the appropriate surgical techniques (e.g., chordal replacement, leaflet resection, Alfieri stich). Concomitant procedures such as atrial fibrillation (AFib) ablation, left atrial appendage (LAA) closure or tricuspid valve repair were performed according to our institutional standards.
Statistical analysis
Anonymous retrospective data collection was obtained using a specifically designed MVS-database. Normally distributed continuous variables are presented as mean values and standard deviation, whereas median and interquartile range are used for non-normally distributed continuous variables. Absolute numbers and percentages are used for categorical variables. Unpaired t-test was used for between-group comparison of normally distributed numeric variables, otherwise Mann–Whitney U-test was used. χ2 test was performed for between-group comparison of categorial variables if the minimum expected cell size was at least 5. Otherwise, Fisher's exact test was used. Kaplan–Meier analysis and logrank test was used to compare mid-term survival during. If p-value was <0.05, results were considered statistically significant. IBM Corp. Released 2019. IBM SPSS Statistics for Windows, Version 26.0. Armonk, NY: IBM Corp. was used for all statistical analyzes. The data underlying this article will be shared on reasonable request to the corresponding author.
Results
Study population
Between 2016 and 2022, a total of 756 consecutive patients underwent endoscopic MVS at our institution due to MR ≥ 2 and were stratified according to age ≥75 or <75 years at the time of surgery (Figure 1A) resulting in median age of 77 (76–80) vs. 58 (51–67) years (p < 0.001) in groups respectively. In addition, prevalence of outcome-relevant comorbidities including hypertension, diabetes, coronary artery disease or AFib was increased within the elderly-group (Table 1). Of note, patients in the elderly-group, were more likely to present with NYHA class III symptoms (45.7% vs. 29.8%; p = 0.002) (Figure 1C) and increased baseline serum-levels of creatinine and natriuretic peptide. According to standard operative risk stratification, patients in the elderly group presented with an overall increased surgical risk profile (STS PROM: 1.9% vs. 0.4%; p < 0.001) (Table 1).
Preoperative echocardiographic characteristics
All patients within both groups, preoperatively presented with MR ≥ 2. The rate of concomitant relevant tricuspid regurgitation (TR) ≥2 was increased in the elderly-group (40.7% vs. 19.1%; p = 0.003). In contrast to comparable rates of PMR, which was present in 69.2% (elderly-group) vs. 77.7% (control-group) of patients (p = 0.052), prevalence of secondary MR (SMR) was significantly increased in the elderly-group (24.2% vs. 13.1%; p = 0.003). Prolapse of the posterior mitral leaflet (PML) represented the most common cause of PMR and was similarly prevalent in groups (42.2% vs. 47.8%; p = 0.316). Left ventricular ejection fraction (LVEF) was similar in both groups (p = 0.228), whereas right ventricular (RV) function, measured as tricuspid annular plane systolic excursion (TAPSE), was significantly impaired in the elderly-group in comparison to the control group (23.0 ± 5.3 vs. 24.6 ± 5.6; p = 0.003). Furthermore, systolic pulmonary artery pressure was increased within the elderly patients (Table 1).
Procedural data
Surgical details are summarized in Table 2. Briefly, direct arterial cannulation of the axillary artery was more frequently used within elderly vs. control group (27.5% vs. 4.2%; p < 0.001). MV repair was performed in 85.7% vs. 93.8% of patients (p = 0.055). Median annuloplasty ring size used, was 32 (30–34) vs. 34 (30–36) mm (p < 0.001). Implantation of neochords (51.6% vs. 69.5%; p = 0.261), as well as leaflet resection (23.1% vs. 14.7%; p = 0.136) were predominantly used to correct leaflet prolapse or flail. Concomitant occlusion of the LAA was performed in 45.1% vs. 23.9% of patients (p < 0.001). Cross-clamp and cardiopulmonary bypass times were similar between groups, whereas procedural time was increased within the elderly group (Table 2).
Perioperative results and 30-day mortality
Median postoperative ventilation time was significantly increased in the elderly group [6.0 (4.6–9.3) h vs. 4.5 (3.0–6.3) h; p < 0.001]. Furthermore, length of stay on intensive care unit [2 (1–4) days vs. 2 (1–3) days; p < 0.001] and length of in-hospital stay [9 (7–13) days vs. 7 (6–9) days; p < 0.001] were longer in the elderly-group. Rates of perioperative myocardial infarction, low cardiac output syndrome, hemodialysis and surgical revision due to bleeding were similar (Table 3). Of note, incidence of perioperative stroke was similarly low (1 patient in each group; p = 0.224). At discharge, 68.1% vs. 73.0% of patients had no residual MR and 27.7% vs. 21.6% had mild residual MR (Figure 2C).
30-day mortality was 2.2% (2/91) vs. 0.45% (3/665 (p = 0.112). One patient in the elderly-group expired due to multi-organ failure 5 days after urgent MVS due to decompensated heart failure. A second patient committed suicide 16 days after surgery.
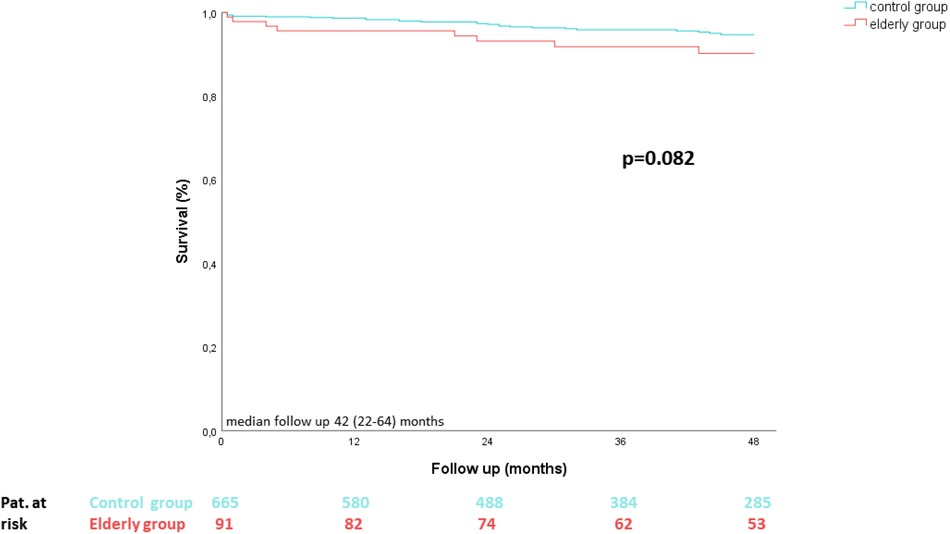
MV re-operation and survival rates during follow up
In contrast to the elderly group, in which MV re-operation was not necessary during a median follow up of 42 (22–64) months, 16 patients within the control group underwent MV re-operation (p = 0.135). Furthermore, Kaplan–Meier survival analysis revealed no statistical differences between groups (p = 0.082) (Figure 3).
Discussion
Endoscopic MVS, which developed as an alternative to full-sternotomy, is traditionally performed in younger patients with low surgical risk. Nevertheless, in addition to transcatheter mitral valve repair strategies (e.g., TEER), minimally-invasive endoscopic MVS, may represent a potential therapeutic option for elderly patients (10).
In the present analysis, patients aged ≥75 years showed similarly low rates of perioperative complications compared to patients <75 years, despite increased prevalence of outcome-relevant comorbidities and overall increased surgical risk.
Study population and preoperative patient characteristics
Patients ≥75 years had increased prevalence of comorbidities, impaired RV function and were more likely to present with NYHA class III symptoms and SMR in comparison to younger patients. Therefore, elderly patients exhibit an increased perioperative surgical risk (8), according to established risk stratification models (e.g., The Society of Thoracic Surgeons (STS) predicted risk of mortality (PROM) score) (STS PROM: 1.9% vs. 0.4%; p < 0.001) (Table 1) (11).. However, relevance of standard risk stratification tools to predict risk in elderly patients undergoing minimally-invasive MVS remains unclear (12). Therefore, in addition to risk score calculation, interdisciplinary heart-team discussion integrating patients' physical status, frailty, anatomical features, as well as life expectancy, is mandatory to achieve optimal patient outcome (13, 14). Of note, all patients included in the current analysis were assessed in a multidisciplinary team and defined as appropriate surgical candidates.
Procedural characteristics, perioperative complications and mid-term follow up
Since introduction of minimally-invasive MVS (6), the technique evolved as an alternative to full-sternotomy, resulting in low rates of perioperative complications, reduced recovery time and superior cosmesis (Figures 2A,B) (7). Due to excellent 3D visualization (Figure 1B), endoscopic MVS can be routinely performed for treatment of a wide variety of mitral and tricuspid valve diseases (15). In addition to isolated MV leaflet prolapse, complex Barlow's disease (16), SMR due to ventricular dysfunction (17, 18), as well as infective endocarditis (19), can be targeted.
Repair rates within our series were 85.7% vs. 93.8% (p = 0.055). Of note, out of 13 patients within the elderly group, who underwent MV replacement, 3 patients had previously received TEER, 3 patients suffered from previous MV endocarditis with advanced destruction of leaflets, 4 patients had advanced leaflet degeneration with partial calcification and 3 patients showed SMR with severe mitral leaflet tethering. In accordance with current guidelines, in particular in the treatment of PMR MV repair was preferred over MV replacement (3), due to better short- and long-term survival, as well as fewer valve related complications, regardless of patients' age (20, 21). The preferred MV repair technique [e.g., “respect vs. resect” (22)], was performed with similar frequency in in both groups. As the implantation of pre-measured PTFE-loops (23) simplifies chordal replacement during minimally-invasive MVS, resulting in excellent long-term durability (24), it became the predominantly used technique (i.e., in 73.1% of all MV repair cases) at our institution.
Retrograde arterial perfusion due to cannulation of the femoral artery potentially represents a risk factor for perioperative stroke during minimally-invasive MVS, especially in patients with aortic or iliofemoral atherosclerosis, although conflicting data has been published (25). Direct cannulation of the right axillary artery to allow for antegrade arterial perfusion evolved as an alternative to conventional femoral cannulation during minimally-invasive MVS (26). Particularly in elderly patients with aortic atherosclerosis, antegrade perfusion may be associated with reduced perioperative stroke rates in comparison to retrograde perfusion (27) even though prospective randomized data does not exist. Of note, direct cannulation of the right axillary artery to facilitate antegrade arterial perfusion was performed in 27.5% of elderly patients in comparison to 4.2% of patients <75years (p < 0.001) and perioperative stroke rates were comparably low (1 patient in each group; p = 0.224) within our cohort.
Due to the absence of a control-group of patients treated with TEER or via full-sternotomy, the comparison to other MV treatment strategies is limited. Nevertheless, favorably low rates of perioperative myocardial infarction, low-cardiac output syndrome, hemodialysis and stroke within both groups, emphasize feasibility and safety of minimally-invasive MVS in elderly patients. Interestingly, perioperative complication rates seem to be lower than in recently published surgically treated elderly cohorts and comparable with real world TEER data (5). Of note, reduced postoperative ventilation time in the control group may reflect recent implementation of an enhanced recovery after cardiac surgery (ERAS) protocol, including patients <70 years at our institution. Expansion of the ERAS protocol from younger to elderly patients may potentially be of clinical value, as elderly patients may specifically benefit from rapid extubation, early postoperative mobilization and reduced duration of in-hospital stay (28).
Overall 30-day mortality was 0.7% (5/756), which compares favorably to published data (12). The numerical difference between groups (2.2% vs. 0.45%; p = 0.112), may be reflective of different baseline and procedural characteristics, e.g., higher rates of SMR and MV replacement in elderly patients (29).
In both groups, >95% of patients showed postoperative MR ≤ I at the time of discharge. Most importantly, freedom from MV re-operation was 100% during a median follow up of 42 months within the elderly group. Given the fact that residual MR > I, which is more frequently accepted after TEER in elderly patients (5), results in worse long-term outcome and survival (30), minimally-invasive MVS therefore represents a promising therapeutic option in elderly patients.
Study limitations
Study limitations include the retrospective single-center study design. However, this is one of the largest consecutive series of elderly patients, undergoing endoscopic MVS at a specialized heart valve center, following institutional standards. Furthermore, despite differing age-related baseline characteristics within both groups, propensity score matching, or regression analysis was not included within our analysis. Therefore, the independent effect of age on the outcome after endoscopic MVS remains unknown. Due to the absence of a control-group of patients treated with TEER or via full-sternotomy, the comparison to other MV therapeutic strategies is limited. Nevertheless, the aim of our study was to demonstrate safety and feasibility of endoscopic MVS in elderly patients. Obviously, patients suffering from age-related contraindications for MVS, such as porcelain aorta or severe frailty, did not undergo MVS and consequentially were not included for analysis. Therefore, favorable perioperative results cannot generally be transferred to the elderly population. Nevertheless, results underline that age alone does not represent a contraindication for endoscopic MVS. Furthermore, it emphasizes the importance of interdisciplinary heart team assessment to select appropriate surgical candidates independent of age.
Conclusion
Despite increased prevalence of outcome-relevant comorbidities and surgical risk, perioperative outcome of patients aged ≥75 years undergoing endoscopic MVS is favorable. Therefore, in addition to transcatheter approaches, endoscopic MVS is a valuable therapeutic option for selected elderly patients and should be taken in consideration during routine heart-team discussion.
Author's note
Data was presented at the DGTHG 52th Annual Meeting 2023 in Hamburg, Germany.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Ethical approval was not required for the study involving humans in accordance with the local legislation and institutional requirements. Written informed consent to participate in this study was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and the institutional requirements.
Author contributions
All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The handling editor [PD] declared a past co-authorship with the author(s) [ODB, HR, LC].
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Iung B, Delgado V, Rosenhek R, Price S, Prendergast B, Wendler O, et al. Contemporary presentation and management of valvular heart disease: the EURObservational research programme valvular heart disease II survey. Circulation. (2019) 140(14):1156–69. doi: 10.1161/CIRCULATIONAHA.119.041080
2. Cahill TJ, Prothero A, Wilson J, Kennedy A, Brubert J, Masters M, et al. Community prevalence, mechanisms and outcome of mitral or tricuspid regurgitation. Heart. (2021):heartjnl-2020-318482. doi: 10.1136/heartjnl-2020-318482. [Epub ahead of print].
3. Vahanian A, Beyersdorf F, Praz F, Milojevic M, Baldus S, Bauersachs J, et al. 2021 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J. (2022) 43(7):561–632. doi: 10.1093/eurheartj/ehab395
4. Feldman T, Kar S, Elmariah S, Smart SC, Trento A, Siegel RJ, et al. Randomized comparison of percutaneous repair and surgery for mitral regurgitation: 5-year results of EVEREST II. J Am Coll Cardiol. (2015) 66(25):2844–54. doi: 10.1016/j.jacc.2015.10.018
5. Buzzatti N, Van Hemelrijck M, Denti P, Ruggeri S, Schiavi D, Scarfo IS, et al. Transcatheter or surgical repair for degenerative mitral regurgitation in elderly patients: a propensity-weighted analysis. J Thorac Cardiovasc Surg. (2019) 158(1):86–94 e81. doi: 10.1016/j.jtcvs.2019.01.023
6. Chitwood WR, Elbeery JR, Chapman WH, Moran JM, Lust RL, Wooden WA, et al. Video-assisted minimally invasive mitral valve surgery: the “micro-mitral” operation. J Thorac Cardiovasc Surg. (1997) 113(2):413–4. doi: 10.1016/S0022-5223(97)70341-6
7. Hawkins RB, Mehaffey JH, Mullen MG, Nifong WL, Chitwood WR, Katz MR, et al. A propensity matched analysis of robotic, minimally invasive, and conventional mitral valve surgery. Heart. (2018) 104(23):1970–5. doi: 10.1136/heartjnl-2018-313129
8. Kolh P, Kerzmann A, Lahaye L, Gerard P,, Limet R. Cardiac surgery in octogenarians; peri-operative outcome and long-term results. Eur Heart J. (2001) 22(14):1235–43. doi: 10.1053/euhj.2000.2443
9. Nagendran J, Catrip J, Losenno KL, Adams C, Kiaii B, Chu MW. minimally invasive mitral repair surgery: why does controversy still persist? Expert Rev Cardiovasc Ther. (2017) 15(1):15–24. doi: 10.1080/14779072.2017.1266936
10. Hage A, Hage F, Al-Amodi H, Gupta S, Papatheodorou SI, Hawkins R, et al. Minimally invasive versus sternotomy for mitral surgery in the elderly: a systematic review and meta-analysis. Innovations. (2021) 16(4):310–6. doi: 10.1177/15569845211000332
11. Shahian DM, Jacobs JP, Badhwar V, Kurlansky PA, Furnary AP, Cleveland JC Jr, et al. The society of thoracic surgeons 2018 adult cardiac surgery risk models: part 1-background, design considerations, and model development. Ann Thorac Surg. (2018) 105(5):1411–8. doi: 10.1016/j.athoracsur.2018.03.002
12. Ko K, de Kroon TL, Post MC, Kelder JC, Schut KF, Saouti N, et al. Minimally invasive mitral valve surgery: a systematic safety analysis. Open Heart. (2020) 7(2). doi: 10.1016/j.jacc.2018.10.007
13. Nishimura RA, O'Gara PT, Bavaria JE, Brindis RG, Carroll JD, Kavinsky CJ, et al. 2019 AATS/ACC/ASE/SCAI/STS expert consensus systems of care document: a proposal to optimize care for patients with valvular heart disease: a joint report of the American association for thoracic surgery, American college of cardiology, American society of echocardiography, society for cardiovascular angiography and interventions, and society of thoracic surgeons. J Am Coll Cardiol. (2019) 73(20):2609–35. doi: 10.1016/j.jacc.2018.10.007
14. Chambers JB, Prendergast B, Iung B, Rosenhek R, Zamorano JL, Pierard LA, et al. Standards defining a “heart valve centre”: ESC working group on valvular heart disease and European association for cardiothoracic surgery viewpoint. Eur Heart J. (2017) 38(28):2177–83. doi: 10.1093/eurheartj/ehx370
15. Van Praet KM, Kempfert J, Jacobs S, Stamm C, Akansel S, Kofler M, et al. Mitral valve surgery: current status and future prospects of the minimally invasive approach. Expert Rev Med Devices. (2021) 18(3):245–60. doi: 10.1080/17434440.2021.1894925
16. Borger MA, Kaeding AF, Seeburger J, Melnitchouk S, Hoebartner M, Winkfein M, et al. Minimally invasive mitral valve repair in Barlow’s disease: early and long-term results. J Thorac Cardiovasc Surg. (2014) 148(4):1379–85. doi: 10.1016/j.jtcvs.2013.11.030
17. Pausch J, Bhadra OD, Sequeira Gross TM, Hua X, Conradi L, Reichenspurner H, et al. Early outcomes of endoscopic papillary muscle relocation for secondary mitral regurgitation type IIIb in patients with severe left ventricular dysfunction. Innovations. (2022) 17(4):317–23. doi: 10.1177/15569845221115419
18. Girdauskas E, Pausch J, Harmel E, Gross T, Detter C, Sinning C, et al. Minimally invasive mitral valve repair for functional mitral regurgitation. Eur J Cardiothorac Surg. (2019) 55(Suppl 1):i17–25. doi: 10.1093/ejcts/ezy344
19. Folkmann S, Seeburger J, Garbade J, Schon U, Misfeld M, Mohr FW, et al. Minimally invasive mitral valve surgery for mitral valve infective endocarditis. Thorac Cardiovasc Surg. (2018) 66(7):525–9. doi: 10.1055/s-0037-1604206
20. Jung JC, Jang MJ, Hwang HY. Meta-analysis comparing mitral valve repair versus replacement for degenerative mitral regurgitation across all ages. Am J Cardiol. (2019) 123(3):446–53. doi: 10.1016/j.amjcard.2018.10.024
21. Lazam S, Vanoverschelde JL, Tribouilloy C, Grigioni F, Suri RM, Avierinos JF, et al. Twenty-year outcome after mitral repair versus replacement for severe degenerative mitral regurgitation: analysis of a large, prospective, multicenter, international registry. Circulation. (2017) 135(5):410–22. doi: 10.1161/CIRCULATIONAHA.116.023340
22. Perier P, Hohenberger W, Lakew F, Batz G, Urbanski P, Zacher M, et al. Toward a new paradigm for the reconstruction of posterior leaflet prolapse: midterm results of the “respect rather than resect” approach. Ann Thorac Surg. (2008) 86(3):718–25; discussion 718–725. doi: 10.1016/j.athoracsur.2008.05.015
23. von Oppell UO, Mohr FW. Chordal replacement for both minimally invasive and conventional mitral valve surgery using premeasured gore-tex loops. Ann Thorac Surg. (2000) 70(6):2166–8. doi: 10.1016/S0003-4975(00)02047-6
24. Pfannmueller B, Misfeld M, Verevkin A, Garbade J, Holzhey DM, Davierwala P, et al. Loop neochord versus leaflet resection techniques for minimally invasive mitral valve repair: long-term results. Eur J Cardiothorac Surg. (2021) 59(1):180–6. doi: 10.1093/ejcts/ezaa255
25. Modi P, Chitwood WR Jr. Retrograde femoral arterial perfusion and stroke risk during minimally invasive mitral valve surgery: is there cause for concern? Ann Cardiothorac Surg. (2013) 2(6):E1. doi: 10.3978/j.issn.2225-319X.2013.11.13
26. Petersen J, Naito S, Kloth B, Pecha S, Zipfel S, Alassar Y, et al. Antegrade axillary arterial perfusion in 3D endoscopic minimally-invasive mitral valve surgery. Front Cardiovasc Med. (2022) 9:980074. doi: 10.3389/fcvm.2022.980074
27. Murzi M, Cerillo AG, Miceli A, Bevilacqua S, Kallushi E, Farneti P, et al. Antegrade and retrograde arterial perfusion strategy in minimally invasive mitral-valve surgery: a propensity score analysis on 1280 patients. Eur J Cardiothorac Surg. (2013) 43(6):e167–72. doi: 10.1093/ejcts/ezt043
28. Klotz SGR, Ketels G, Behrendt CA, Konig HH, Kohlmann S, Lowe B, et al. Interdisciplinary and cross-sectoral perioperative care model in cardiac surgery: implementation in the setting of minimally invasive heart valve surgery (INCREASE)-study protocol for a randomized controlled trial. Trials. (2022) 23(1):528. doi: 10.1186/s13063-022-06455-x
29. Di Tommaso E, Rapetto F, Guida GA, Zakkar M, Bruno VD. Benefits of mitral valve repair over replacement in the elderly: a systematic review and meta-analysis. J Card Surg. (2021) 36(7):2524–30. doi: 10.1111/jocs.15506
Keywords: mitral regurgitation, minimally-invasive mitral valve surgery, endoscopic mitral valve surgery, mitral valve repair, transcatheter mitral valve repair
Citation: Pausch J, Bhadra OD, Hua X, Stolfa P, Kuhlmann C, Voß M, Girdauskas E, Reichenspurner H and Conradi L (2023) Early outcome of endoscopic mitral valve surgery in elderly patients: a high-volume single center experience. Front. Cardiovasc. Med. 10:1182752. doi: 10.3389/fcvm.2023.1182752
Received: 9 March 2023; Accepted: 7 November 2023;
Published: 28 November 2023.
Edited by:
Paolo Denti, San Raffaele Hospital (IRCCS), ItalyReviewed by:
Praveen Varma, Amrita Vishwa Vidyapeetham University, IndiaClaudia Maria Loardi, Centre Hospitalier Universitaire de Tours, France
© 2023 Pausch, Bhadra, Hua, Stolfa, Kuhlmann, Voß, Girdauskas, Reichenspurner and Conradi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jonas Pausch j.pausch@uke.de
Abbreviations AFib, atrial fibrillation; AML, anterior mitral leaflet; CPB, cardiopulmonary bypass; ECLS, extracorporeal life support; EROA, effective regurgitant orifice area; FU, follow up; IABP, intra-aortic balloon pump; LAA, left atrial appendage; LV, left ventricle; LVEDD, left ventricular end-diastolic diameter; LVEF, left ventricular ejection fraction; MR, mitral regurgitation; MV, mitral valve; MVR, mitral valve replacement; MVS, mitral valve surgery; pro-BNP, pro-brain natriuretic peptide; NYHA, New York Heart Association; PML, posterior mitral leaflet; PMR, primary mitral regurgitation; SMR, secondary mitral regurgitation; TAPSE, tricuspid annular plane systolic excursion; TEER, transcatheter edge-to-edge repair; TR, tricuspid regurgitation; VHD, valvular heart disease.
 Jonas Pausch
Jonas Pausch Oliver D. Bhadra
Oliver D. Bhadra Xiaoqin Hua1
Xiaoqin Hua1  Evaldas Girdauskas
Evaldas Girdauskas Lenard Conradi
Lenard Conradi