Application of mind map can promote the health education effect of children with vasovagal syncope
- 1Clinical Nursing Teaching and Research Section, The Second Xiangya Hospital, Central South University, Changsha, Hunan, China
- 2Department of Pediatric Cardiovasology, Children's Medical Center, The Second Xiangya Hospital, Central South University, Changsha, Hunan, China
Objective: To explore the effect of mind map on health education in children with vasovagal syncope (VVS).
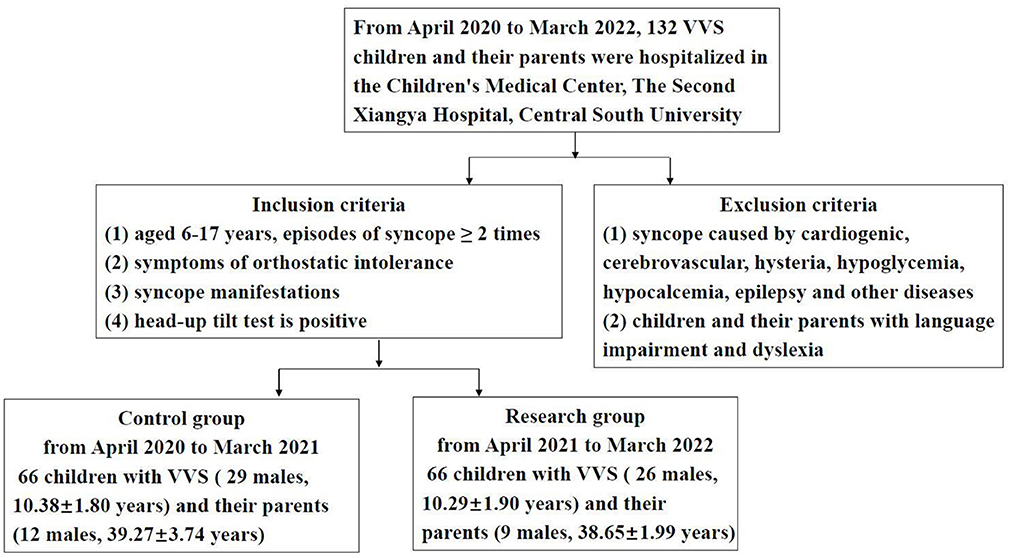
Methods: In this prospective controlled study, 66 children with VVS (29 males, 10.38 ± 1.80 years) and their parents (12 males, 39.27 ± 3.74 years) who were hospitalized in the Department of Pediatrics, The Second Xiangya Hospital, Central South University from April 2020 to March 2021 were set as the control group. 66 children with VVS (26 males, 10.29 ± 1.90 years) and their parents (9 males, 38.65 ± 1.99 years) who were hospitalized in the same hospital from April 2021 to March 2022 were set as the research group. Traditional oral propaganda method was applied in the control group, and the health education method based on mind map was applied in the research group. The self-designed VVS health education satisfaction questionnaire and comprehensive health knowledge questionnaire were used to conduct on-site return visits to the children and their parents who had been discharged from the hospital for 1 month.
Results: There was no significant difference in age, sex, hemodynamic type of VVS, and the parental age, sex, education level between the control group and the research group (P > 0.05). Health education satisfaction score, health education knowledge mastery score, compliance score, subjective efficacy and objective efficacy in the research group were higher than those in the control group (P < 0.05). If the satisfaction score, knowledge mastery score, and compliance score increase by 1 point, the risk of poor subjective efficacy is reduced by 48, 91, and 99%, respectively, and the risk of poor objective efficacy is reduced by 44, 92, and 93%, respectively.
Conclusions: Application of mind map can improve the health education effect of children with VVS.
1. Introduction
Vasovagal syncope (VVS) is a common type of neurally mediated syncope in children, and the incidence is higher in females than males (1–4). It is characterized by transient loss of consciousness, inability to maintain an upright posture of the body and falling to the ground. Clinically, some patients may have recurrent syncope episodes or pre-syncope symptoms, and even syncope-related physical accidental injury (5, 6), or anxiety and depression, loss of appetite, increased somatic symptoms and loss of confidence, resulting in a decrease in the quality of life of the child and seriously affecting the patient's learning and life (7). Taking effective intervention measures for VVS as early as possible can avoid or reduce the onset of these symptoms. Clinically, the treatment of VVS mainly based on non-drug treatment such as health education (8), including avoiding predisposing factors, anti-resistance training and increasing water and salt intake (8–10), etc. Syncope and pre-syncope symptoms can be effectively reduced through health education and some lifestyle changes (e.g., recognizing syncope prodromal symptoms, increasing water intake, anti-resistance training and physical exercise, etc.), thereby improving the quality of life and learning for children with VVS (11). It can be seen that effective health education and lifestyle guidance are crucial in VVS rehabilitation. At present, the health education methods for children with VVS are mostly dependent on traditional oral education. Children with VVS who were hospitalized for treatment were short in hospital, and the communication and expression skills of the mission nurses were different, the effective health education information received by children and their parents was limited, resulting in the failure of health education. In order to explore effective ways to improve the quality and efficiency of health education for children with VVS, this study introduced the health education method of mind map.
The mind map is a thinking tool that concretizes divergent thinking. It uses lines, symbols, vocabulary and images to form divergent and node-like structural forms, and turns cumbersome text information into a visual diagram with clear layers and rich pictures and texts. It not only omits the tedious and complicated oral communication process, but also intuitively provides visual stimulation to children and their parents, deepens the impression of key content, and eliminates the inefficient information dissemination caused by hearing fatigue, and allows learners to store and extract information more effectively, and improve work and learning efficiency (12, 13). Some studies have shown that mind maps can improve the health education effect of patients (14–16). Li et al. (17) has found that the combined communication mode of SBAR (namely Situation, Background, Assessment, Recommendation) standard and mind map used in the emergency department can improve the quality of handover, reduce adverse events and handover problems, and get higher patient satisfaction. In this study, mind map was introduced to the health education of children with VVS and their parents, and the effect of mind mapping on VVS children's health education was observed.
2. Study population and methods
2.1. Study population and data collection
A prospective controlled study was conducted. The inclusion criteria and exclusion criteria were shown in Figure 1. Children with VVS and their parents were divided into control group and research group. The study subjects returned to the hospital for follow-up visits 1 month after discharge.
The sample size was calculated by using the formula n1 = n2 = [(Zα + Zβ)2 × 2σ2]/δ2. The outcome index of this study was compliance score. The average compliance score of the control group was expected to be 3.00 ± 1.3 points, and the compliance score of the study group was expected to be increased by 1.0 points. Bilateral test, α was 0.05, the sample size ratio of the two groups was 1:1, and the test efficacy was 1 – β = 90%. The sample size calculated was 41. Consider a 25% shedding rate, the required minimum total number of participants was 51 in our study. We selected a sample size of 66 cases in each group.
2.2. Implementer of health education
The health education of the research group and the control group were implemented by pediatric specialist nurses, aged 26–45 years old, with an average age of 33.00 ± 5.03 years old.
2.3. Methods of health education
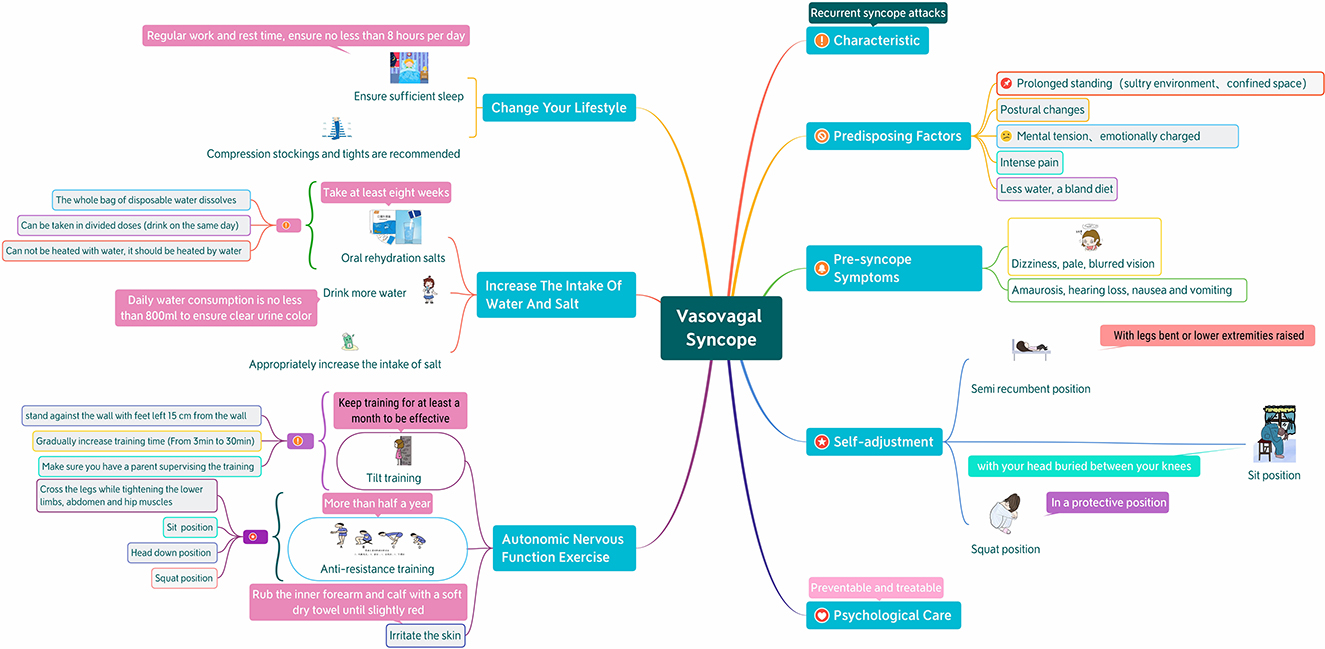
The control group received the conventional health education method, namely the oral education method, which lasted about 15–30 min. After the diagnosis was confirmed, the nurses explain VVS-related knowledge to the children and their parents, including common predisposing factors for syncope, increasing intake of water and salt, methods of taking oral rehydration salts, and instructing children on autonomic nerve function exercises, emphasizing that exercises should be performed as required. The research group received the mind map health education method, about 10–15 min. First of all, the nurses in our hospital would be trained on the knowledge of mind map. The training content was based on the medical knowledge of VVS, focusing on the background and usage of mind map. A total of 4 h of training would be conducted. After passing the real-life operation assessment, they would participate in this study. On the basis of evidence-based nursing and clinical experience, the members of the research team made a mind map, based on the content of traditional VVS health education and guided by the general information of children and their parents, to select the key points of pediatric VVS health education, from the perspective of patients, consult the literature and design a mind map of pediatric VVS self-prevention management based on peer practices. The drawing follows the principles of reasonable logic, clear fonts, and rich pictures and texts, and uses the mind map software X Mind 8 to draw (Figure 2). After the diagnosis was confirmed, the children and their parents were given health education by using mind maps. The nurses emphasized the key points one by one according to the mind maps, and guided the children to exercise their autonomic nerve function. After the teaching, hand over the mind map to the children and their parents, and guide them to consolidate knowledge and improve compliance as shown in the picture. Nurses supervise their implementation in their daily work, and carry out targeted health education as appropriate.
2.4. Evaluation method
2.4.1. General information questionnaire
The research team asked children and their parents to complete the questionnaire. The contents of the questionnaire included the child's name, sex, date of birth, academic performance, place of residence and parents' age, education level, and telephone number.
2.4.2. Health education satisfaction questionnaire (for children and their parents)
A self-designed health education satisfaction questionnaire was used. The contents include nurses' introduction of disease-related knowledge, guidance on eating and living habits, guidance on autonomous function exercise, guidance on drugs and psychological counseling. The score calculation standard was as follows: 2, satisfaction; 1, general; 0, dissatisfaction. The full score is 16 scores. The higher the score, the higher the satisfaction. The assessment was performed by the patient and the parents before the patient was discharged from the hospital. We collected 66 valid questionnaires from the research group and the control group respectively, and the recovery rate and effective rate were both 100%.
2.4.3. Health education knowledge questionnaire
The self-designed VVS health education knowledge questionnaire was used to conduct on-site return visits to the children and their parents who had been discharged from the hospital for 1 month, and understand their mastery of VVS health education knowledge, syncope frequency, compliance and re-examination of head-up tilt test (HUTT) results, etc. The specific content is as follows: (1) What are the predisposing factors for syncope? (At least answer 3 or more predisposing factors, such as prolonged standing, postural changes, strenuous exercise, etc.). (2) What to do if fainting occurs? (For example, keep your supine position with your legs slightly elevated; in a sitting position, bury your head between your knees; in a squat position, clasp your hands tightly and hold your legs tightly in a protective position). (3) What are the precautions for oral rehydration salts? (The daily amount is dissolved at one time and can be taken in divided doses; it cannot be mixed with water in the middle; it can be warmed with water; drink it up on the same day). (4) How is the autonomic nervous system exercise performed? (Such as stand training, anti-resistance training, etc. Answer at least one of them and be absolutely correct). (5) Are you taking oral rehydration salts as prescribed by your doctor? (6) Do you do autonomic nervous system exercise every day? (7) Are you guaranteed three meals a day and enough sleep? (Sleep at least 8 h per day). (8) Do you use compression stockings or tights pants? In the questionnaires survey, “know” is scored as 1, “don't know” is scored as 0; if the answer is “yes,” it is scored as 1, and the answer of “no” is scored as 0. 66 valid questionnaires were collected from the research group and the control group, respectively, and the recovery rate and effective rate were both 100%.
2.4.4. Evaluation of efficacy
(1) Subjective efficacy: after training, the number of syncope or the occurrence of syncope premonitory in the child was reduced compared with that before treatment or had no episodes, which was regarded as improvement; after the training, the number of syncope or the occurrence of syncope is increased or no change, which was regarded as noimprovement. Efficiency (Improvement rate) = number of improved cases/total number of cases. (2) Objective efficacy: according to the HUTT results of the patient's re-examination, the HUTT induced syncope time was longer than the previous once, or the result change from positive to negative, which was regarded as improved; shortened time to induction of syncope, or no change in HUTT results was considered no improvement.
2.4.5. Head-up tilt test (HUTT)
2.4.5.1. Preparations before the test
Children fasted for at least 4 h before the testing, any vasoactive medication was stopped for at least five half-lives, and drink that could affect autonomic nervous system function (e.g., coffee) was avoided. The test was performed ata suitable temperature, dim light, and quiet environment. Detailed instructions and risks should be described to children and their legal guardians/parents. Signed informed consent should be obtained before the test (9, 18, 19).
2.4.5.2. Basic HUTT (BHUT)
The test was performed using Head-up Tilt Test Mornitoring System (SHUT-100) of Jiangsu Standard Medical Technology Co., Ltd. after overnight fasting between 8:00 a.m. and 12:00 p.m. The subjects were asked to lay still for 10 min, and then baseline heart rate (HR), blood pressure (BP), and ECG were recorded. Subjects were tilted at 60° with head upward, and HR, BP, and ECG were recorded continuously until either 45 min duration, or the development of syncope or intolerable near syncope symptoms. If syncope occurred, patients were rapidly placed in the supine position.
2.4.5.3. Sublingual nitroglycerin HUTT (SNHUT)
If the subjects did not develop syncope or pre-syncope, they underwent SNHUT. A tilted posture was maintained, subjects were medicated with nitroglycerin 4–6 μg/kg (maximum ≤ 300 μg), and HR, BP, and ECG were recorded for 20 min or until syncope or pre-syncope occurred.
2.4.5.4. Diagnosis of VVS and response types
VVS was defined as the development of syncope or pre-syncope accompanied by hypotension (systolic BP ≤ 80 mmHg and/or diastolic BP ≤ 50 mmHg, or over 25% decrease in mean BP), bradycardia (HR < 75 bpm for children at 4–6 years of age, <65 bpm for children at 6–8 years of age, and <60 bpm for children at 8 years of age and older), or cardiac arrest >3 s. VVS was further classified into three responses: vasoinhibitory type VVS (VVS-VI) (significant reduction in BP but insignificant change in HR), cardioinhibitory type VVS (VVS-CI) (significant reduction in HR but insignificant change in BP), and mixed type VVS (VVS-M) (significant reduction both in BP and HR).
2.5. Statistical analysis
The continuous variables were characterized by mean ± standard deviation, or as median and interquartile range, as appropriate. The categorical variables were presented as a number (n) and percentages (%). The Student's t-test, Chi-square test, Fisher's exact test, or Mann–Whitney U test were conducted to compare factors between two groups, as appropriate. Univariate binary Logistic regression was used to briefly evaluate the approximate effects of factors on the efficacy and direction of both subjective efficacy and objective efficacy. Multifactor Logistic regression to analyze the possible association between subjective efficacy and objective efficacy and many factors was used and constructed two models to illustrate the stability of this relationship: Model 1 adjusted for sociodemographic data (sex, age); Mode 2 adjusted for sociodemographic data and parental sex and age and education level, hemodynamic type of VVS. All the analyses were performed with the statistical software packages R (version 3.6.1) (http://www.R-project.org, The R Foundation) and EmpowerStats (http://www.empowerstats.com, X & Y Solutions, Inc, Boston, MA). P-values < 0.05 (two-sided) were considered statistically significant.
3. Results
3.1. General data and questionnaire data analysis
There were no significant differences in age and sex of the children and their parents between the research group and the control group (P > 0.05). The satisfaction on health education, the awareness rate of health education, the compliance of health education, the satisfaction score, the knowledge score, the compliance score, the subjective efficacy and the objective efficacy of the research group were higher than those of the control group (P < 0.01). There was no statistical difference in hemodynamic types of VVS and parental education between the research group and the control group (P > 0.05) (Table 1).
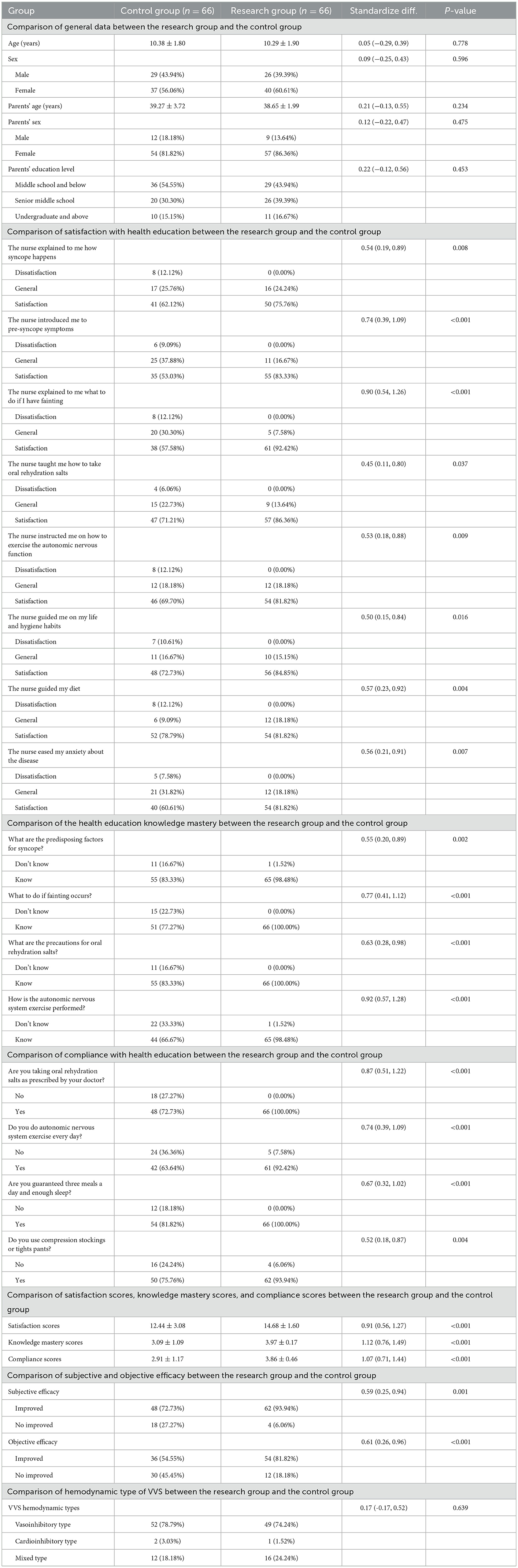
Table 1. General data of the study population and description of questionnaire data [Mean ± SD/n (%)].
3.2. Univariate analysis of subjective efficacy and objective efficacy
The research group was the protective factor of subjective efficacy and objective efficacy. The ages of the children and their parents were the risk factors of subjective efficacy, the education level of the parents in high school was the protective factor of subjective efficacy and objective efficacy, the satisfaction score and the knowledge mastery score and the compliance score were the protective factor of subjective efficacy and objective efficacy (P > 0.05) (Table 2).
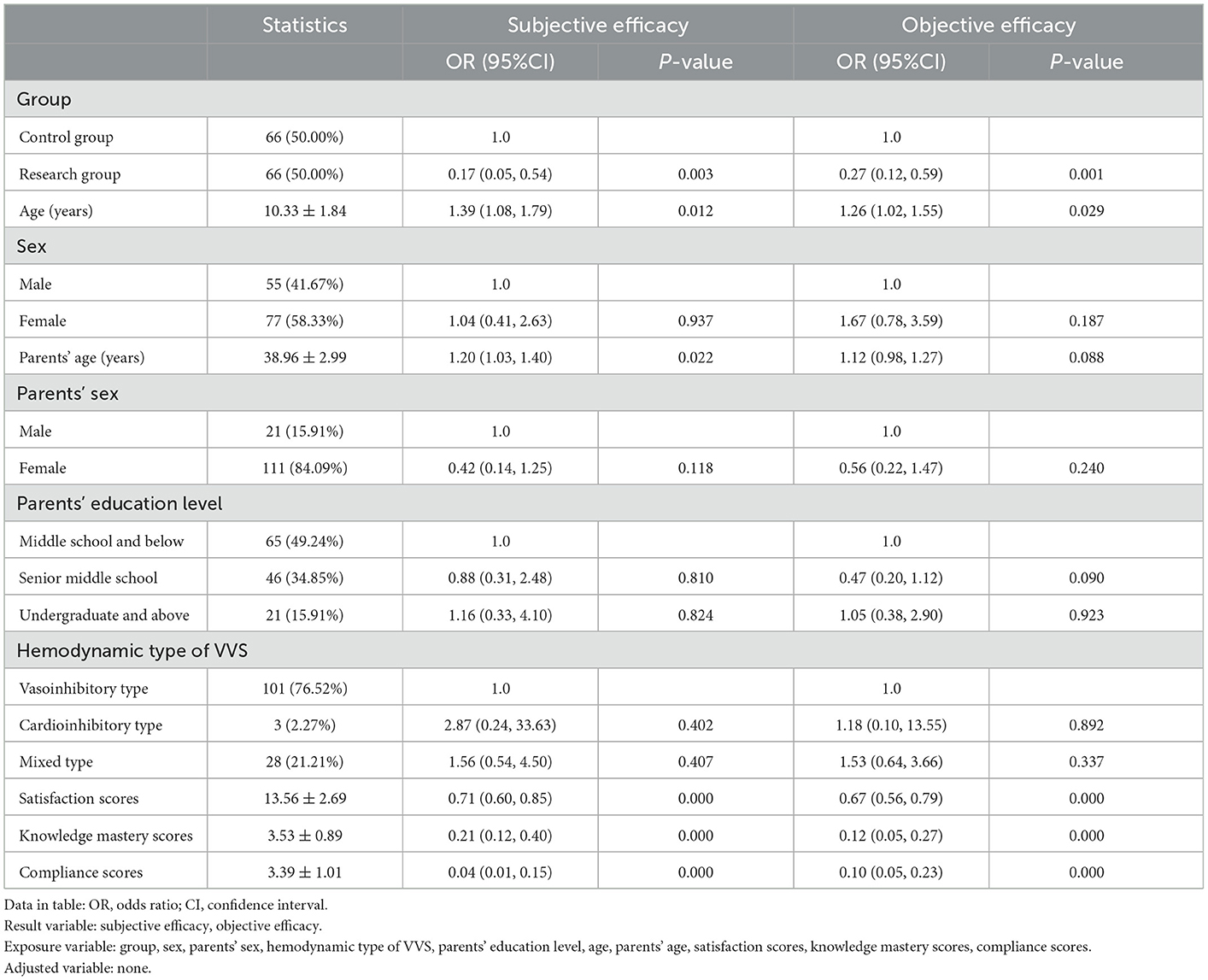
Table 2. Univariate analysis of subjective efficacy and objective efficacy [n = 132, Mean ± SD/n (%)].
3.3. Comparison of multifactor regression equations of subjective efficacy and objective efficacy
In order to further clarify whether satisfaction score, knowledge mastery score and compliance score had independent and stable influences on subjective and objective efficacy in univariate analysis, we conducted a comparison of multifactor binary Logistic regression equations. After adjusting different confounding factors, the model still showed good stability and small fluctuation of effect value. The satisfaction score, knowledge mastery score, and compliance score increased by 1 point, the risk of poor subjective efficacy was reduced by 48, 91, and 99%, respectively, and the risk of poor objective efficacy was reduced by 44, 92, and 93%, respectively (Table 3).
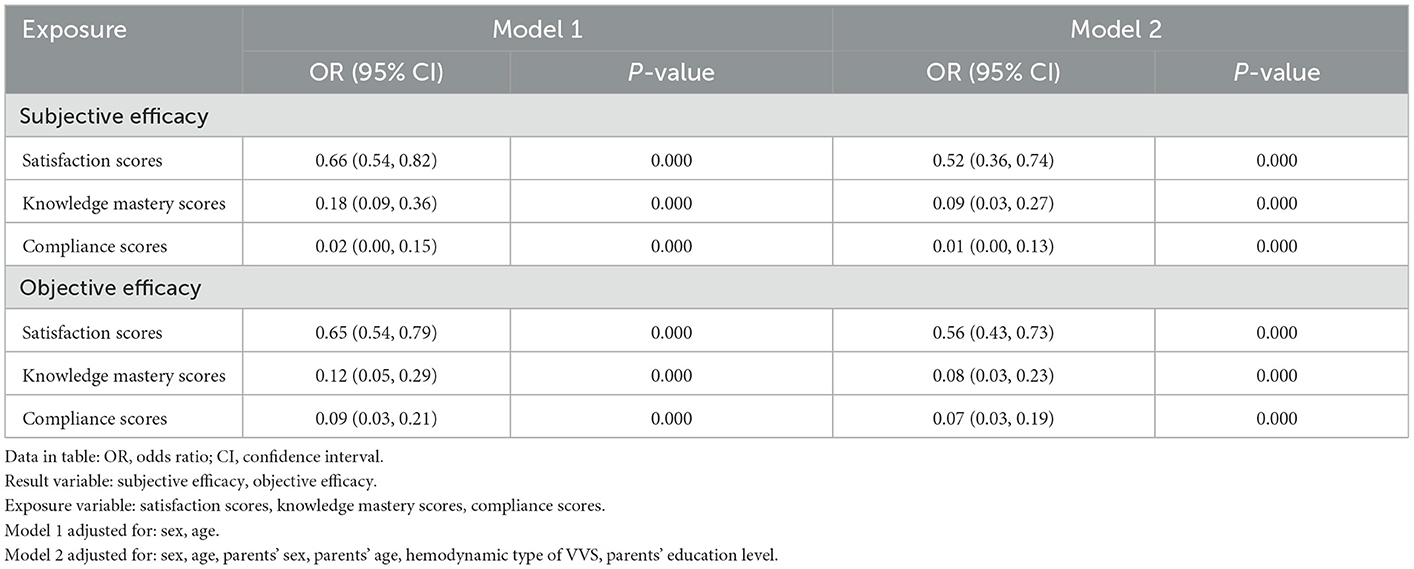
Table 3. Comparison of multifactor regression equations of subjective efficacy and objective efficacy.
4. Discussion
VVS is a common neurally mediated syncope in clinical practice, and health education is the basic measure for intervention of VVS (8). Although the prognosis of VVS is good, due to the lack of knowledge of the disease and health education of the children and their parents, the compliance of the intervention and the rehabilitation effect are affected, which can lead to the recurrence of syncope or pre-syncope. In addition to seriously affecting the physical and mental health and quality of life of the children, the parents are also under great psychological pressure. Therefore, paying attention to the psychological feelings and service requirements of children with VVS and their parents, especially the health education of children and their parents, and improving their compliance, are the key links to promoting the rehabilitation of children (20, 21).
The purpose of health education is not only to “educate knowledge,” but also to establish “medical compliance behavior or healthy behavior” through guidance. Its effect is closely related to factors such as health educators, health education methods and health education objects. In order to avoid the omission of information or unclear expression due to the differences in theoretical knowledge and language expression ability of health educators, the health education practitioners in this study are all highly educated nurses who have undergone unified training and have worked in clinical practice for at least 3 years. Individuals have different abilities to understand and accept information, and people have limited short-term memory, and the content of oral education is easy to forget, which may lead to children and their parents lack of information acceptance or lack of understanding, resulting in reduced compliance. The mind map used in this study can make up for this deficiency. Mind map can turn boring information into colorful and well-organized diagrams to help understand memory (13, 22) (Figure 2).
4.1. Health education method based on mind map can improve the satisfaction of children with VVS and their parents with health education
The results of this study showed that the research group's satisfaction score for health education was increased compared with the control group (P < 0.01), and the risk of poor subjective efficacy was decreased by 48% and the risk of poor objective efficacy was decreased by 44% for each point increase of satisfaction score of health education in clinical nursing work in the research group. It is suggested that the health education method based on mind mapping can improve the satisfaction of health education and intervention effect of children with VVS and their parents. Zhang et al. (23) applied mind map to the health education of parents of children with infectious mononucleosis, and found that the research group was significantly higher than the control group in terms of nursing satisfaction in nurse-patient communication, health education, and nursing technology (P < 0.01). This may be related to the simplicity and clarity of the mind map, focusing on prominent features, which is more conducive to the transmission of information. Targeted health education can promote emotional communication between nurses and patients, increase the trust between nurses and patients, and thus improve the satisfaction of children and their parents with clinical nursing work. Gakhal et al. (13) also reported that the use of audiovisual presentations and mind map exercises to improve the information recall ability of orthodontic patients and their parents and found that the use of audiovisual presentations and written information can improve the information recall rate of orthodontic patients and their parents, and thought mind map is a better form than written information. It can be seen that the health education method based on mind mapping can improve the health education effect of children with VVS and their parents.
4.2. The health education method based on mind map can improve the mastery of health education knowledge and compliance in children with VVS and their parents
Through the health education knowledge questionnaire, it was found that the research group had significantly higher scores on the mastery of health education knowledge and compliance than the control group (P < 0.01). And in research group, the risk of poor subjective efficacy was decreased by 91 and 99% for each point increase of the score of mastery knowledge and compliance, respectively. The risk of poor objective efficacy was decreased by 92 and 93% for each point increase of the score of mastery knowledge and compliance, respectively. The above results suggested that the health education based on mind map can improve the compliance of children with VVS and their parents to health education, avoid possible clinical inducements and triggers, effectively increase the intake of water and salt, and ensure the effectiveness of the intervention. Studies have shown that the application of mind map in pediatric VVS health education can improve the compliance of children and their parents. Sesanelvira et al. (24) reported the educational effect of using mind map method on school-age children's food safety behavior, and found that the use of mind map method has a significant impact on school-age children's food safety knowledge, attitudes and skills. It is believed that the mind map method can be applied to improve the clean and healthy living behaviors of school-age children. Yang et al. (25) reported the application of mind map health education in extended care for children with caries, and found that the use of mind map health education method could significantly improve the caries knowledge of children with caries and their parents, and improve their compliance to health education. Therefore, mind mapping is an appropriate health education tool that can be used for extended care of children with dental caries. In conclusion, health education based on mind map can carry out effective cognitive and behavioral intervention for children and their parents, thereby significantly improving the cognitive level of children and their parents in dealing with disease-related knowledge, and effectively improving the compliance and quality of life of children.
4.3. The health education method based on mind map can improve the subjective efficacy and objective efficacy of VVS children
In this study, both the subjective efficacy and objective efficacy of the research group and the control group were improved, and the subjective and objective efficacy of the research group were better than those of the control group (P < 0.01). And the research group was the protective factor of subjective efficacy and objective efficacy, the satisfaction score, the knowledge mastery score and the compliance score were the protective factor of subjective efficacy and objective efficacy, which was related to the improvement of patient compliance behavior with mind map (26). The mind map is easy to understand and can make up for the unclear explanations and understandings in oral health education. It can carefully let children with VVS and their parents clarify the rehabilitation knowledge of VVS, and provide guidance for effective rehabilitation and improved prognosis. This study shows that the parents' education level in high school is a protective factor for both subjective efficacy and objective efficacy, indicating that the group with higher education levels has a higher acceptance level and understanding ability of health education, which is conducive to improving compliance. The ages of the children and their parents were risk factors for subjective efficacy, which may be related to the obvious anxiety about syncope or pre-syncope episodes in older age.
It can be seen that the application of a mind map in the health education of children with VVS and their parents can increase the clinical intervention effect.
5. Shortcomings and prospects
However, this study had certain limitations. It was a single-center-based research, the subjects were younger and the sample size was not large enough. At the same time, due to the impact of the COVID-19 epidemic, the research group did not recruit the research subjects at the same time, which needs to be avoided in the future research. Therefore, further large sample and multi-center studies can be conducted in the future, and the outcome indicators can be added to verify the educational program. It is recommended to promote and establish patient health records in pediatric cardiovascular outpatient clinics, record the progress of health education during patient follow-up, and lay a foundation for follow-up research.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee of The Second Xiangya Hospital, Central South University. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author contributions
PL and WM had primary responsibility for the protocol development, patient enrollment, data collecting preliminary data analysis, and writing the manuscript. MZ was responsible for the drawing. TZ was responsible for language polishing. YW and RZ completed the head-up tilt test. PL and CW assisted with critical revision for important content and edited the draft. CW supervised the design, execution of the study, checked the data analysis, and contributed to a final approval of the manuscript submitted. All authors have read and approved the final manuscript and assumed full responsibility for its contents.
Funding
This work was supported by grants from National High Level Hospital Clinical Research Funding (Multi-Center Clinical Research Project of Peking University First Hospital) (2022CR59) and Hunan Province Clinical Medical Technology Innovation Guidance Project (2020SK53405 and 2020SK53406).
Acknowledgments
Thanks to Dr. Shuo Wang from the Department of Neonatology, Xiangya Hospital, Central South University for the help in statistical work of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Li HX, Gao L, Yuan Y. Advance in the understanding of vasovagal syncope in children and adolescents. World J Pediatr. (2021) 17:58–62. doi: 10.1007/s12519-020-00367-z
2. Wang Y, Wang Y, He B, Tao C, Han Z, Liu P, et al. Plasma human growth cytokines in children with vasovagal syncope. Front Cardiovasc Med. (2022) 9:1030618. doi: 10.3389/fcvm.2022.1030618
3. Hu E, Liu X, Chen Q, Wang C. Investigation on the incidence of syncope in children and adolescents aged 2–18 years in Changsha. Front Pediatr. (2021) 9:638394. doi: 10.3389/fped.2021.638394
4. Xu WR, Du JB, Jin HF. Can pediatric vasovagal syncope be individually managed? World J Pediatr. (2022) 18:4–6. doi: 10.1007/s12519-021-00495-0
5. Jorge JG, Pournazari P, Raj SR, Maxey C, Sheldon RS. Frequency of injuries associated with syncope in the prevention of syncope trials. Europace. (2020) 22:1896–903. doi: 10.1093/europace/euaa246
6. Hino S, Yamada M, Araki R, Kaneko T, Horie N. Effects of loss of consciousness on maxillofacial fractures in simple falls. Dent Traumatol. (2019) 35:48–53. doi: 10.1111/edt.12452
7. Ng J, Sheldon RS, Ritchie D, Raj V, Raj SR. Reduced quality of life and greater psychological distress in vasovagal syncope patients compared to healthy individuals. Pacing Clin Electrophysiol. (2019) 42:180–8. doi: 10.1111/pace.13559
8. Wang C, Li Y, Liao Y, Tian H, Huang M, Dong X, et al. 2018 Chinese Pediatric Cardiology Society (CPCS) guideline for diagnosis and treatment of syncope in children and adolescents. Sci Bull. (2018) 63:1558–64. doi: 10.1016/j.scib.2018.09.019
9. Chu W, Wang C, Wu L, Lin P, Li F, Zou R. Oral rehydration salts: an effective choice for the treatment of children with vasovagal syncope. Pediatr Cardiol. (2015) 36:867–72. doi: 10.1007/s00246-015-1097-5
10. Wen C, Wang S, Zou R, Wang Y, Tan C, Xu Y, et al. Duration of treatment with oralrehydration salts for vasovagal syncope in children and adolescents. Turk J Pediatr. (2020) 62:820–5. doi: 10.24953/turkjped.2020.05.014
11. Aghajani F, Tavolinejad H, Sadeghian S, Bozorgi A, Jalali A, Vasheghani-Farahani A, et al. Implementation of supervised physical training to reduce vasovagal syncope recurrence: a randomized controlled trial. J Cardiovasc Electrophysiol. (2022) 33:1863–70. doi: 10.1111/jce.15578
13. Gakhal MK, Kwon O. Improving orthodontic patients' and parents' information recall with use of audio-visual presentation and mind mapping exercises. Evid Based Dent. (2020) 21:34–5. doi: 10.1038/s41432-020-0073-y
14. Michelini CA. Mind map: a new way to teach patients and staff. Home Healthc Nurse. (2000) 18:318–22. doi: 10.1097/00004045-200005000-00012
15. Farrand P, Hussain F, Hennessy E. The efficacy of the 'mind map' study technique. Med Educ. (2002) 36:426–31. doi: 10.1046/j.1365-2923.2002.01205.x
16. Walker D, Adebajo A, Heslop P, Hill J, Firth J, Bishop P, et al. Patient education in rheumatoid arthritis: the effectiveness of the ARC booklet and the mind map. Rheumatology. (2007) 46:1593–6. doi: 10.1093/rheumatology/kem171
17. Li X, Zhao J, Fu S. SBAR standard and mind map combined communication mode used in emergency department to reduce the value of handover defects and adverse events. J Healthc Eng. (2022) 2022:8475322. doi: 10.1155/2022/8475322
18. Zou R, Wang S, Li F, Lin P, Zhang J, Wang Y, et al. The application of head-up tilt test to diagnose hemodynamic type of orthostatic intolerance in children aged between 3 and 5 years old. Front Pediatr. (2021) 9:623880. doi: 10.3389/fped.2021.623880
19. Zou R, Wang S, Wen W, Cai H, Wang Y, Liu P, et al. Risk factors and prognostic follow-up of vasovagal syncope children with seizure-like activities during head-up tilt test induced-syncope. Front Cardiovasc Med. (2022) 9:916542. doi: 10.3389/fcvm.2022.916542
20. Liu P, Zeng X, Mei W, Wang Y, Zou R, Wang C. The predictive value of urine specific gravity in the diagnosis of vasovagal syncope in children and adolescents. Ital J Pediatr. (2021) 47:93. doi: 10.1186/s13052-021-01043-2
21. Zhao T, Wang S, Wang M, Cai H, Wang Y, Xu Y, et al. Research progress on the predictive value of electrocardiographic indicators in the diagnosis and prognosis of children with vasovagal syncope. Front Cardiovasc Med. (2022) 9:916770. doi: 10.3389/fcvm.2022.916770
22. Liu T, Yuizono T. Mind mapping training's effects on reading ability: detection based on Eye Tracking Sensors. Sensors. (2020) 20:4422. doi: 10.3390/s20164422
23. Zhang B, Xie A, Wang C, Yang Y, Sun Y. Application of mind mapping in health education for parents of children with infectious mononucleosis. J Nurs Admin. (2021) 21:757–60. doi: 10.3969/j.jssn.1671-315x.2021.10.015
24. Sesanelvira ADIM, Mulyono S, Sukihananto S. Improving food safety behavior through mind map methods in school-age children. Compr Child Adolesc Nurs. (2019) 42:97–107. doi: 10.1080/24694193.2019.1578301
25. Yang H, Gao XB Li MH, Ye Q, Sun Y, Huang Y. The use of mind mapping in health education in extended care for children with caries. J Int Med Res. (2020) 48:300060519898053. doi: 10.1177/0300060519898053
Keywords: children, vasovagal syncope, health education, effect, mind map
Citation: Liu P, Mei W, Zhou M, Zhao T, Wang Y, Zou R and Wang C (2023) Application of mind map can promote the health education effect of children with vasovagal syncope. Front. Cardiovasc. Med. 10:1051677. doi: 10.3389/fcvm.2023.1051677
Received: 23 September 2022; Accepted: 27 January 2023;
Published: 16 February 2023.
Edited by:
Zhen-Yu Zhang, KU Leuven, BelgiumReviewed by:
Jesus Melgarejo, KU Leuven, BelgiumOswin Grollmuss, Université Paris-Sud, France
Shikai Yu, Tongji University, China
Shohreh Naderimagham, Tehran University of Medical Sciences, Iran
Copyright © 2023 Liu, Mei, Zhou, Zhao, Wang, Zou and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Cheng Wang,  wangcheng2nd@csu.edu.cn
wangcheng2nd@csu.edu.cn
†ORCID: Cheng Wang orcid.org/0000-0002-7120-0654
 Ping Liu
Ping Liu Wanzhen Mei
Wanzhen Mei Mengying Zhou
Mengying Zhou Ting Zhao
Ting Zhao Yuwen Wang
Yuwen Wang Runmei Zou
Runmei Zou Cheng Wang
Cheng Wang