Incidence and outcomes of acute high-risk chest pain diseases during pregnancy and puerperium
- 1Department of Military Health Statistics, Navy Medical University, Shanghai, China
- 2Department of Cardiology, Changhai Hospital, Navy Medical University, Shanghai, China
- 3Department of Gynecology and Obstetrics, Changhai Hospital, Navy Medical University, Shanghai, China
Aim: To investigate the incidence and outcomes of acute high-risk chest pain diseases, including acute myocardial infarction (AMI), aortic dissection (AD), and pulmonary embolism (PE) during pregnancy and puerperium.
Methods: The National Inpatient Sample was queried to identify pregnancy-related hospitalizations from January 1, 2008 to December 31, 2017. Temporal trends in the incidence and mortality of AMI, AD and PE were extracted.
Results: Among 41,174,101 hospitalizations, acute high-risk chest pain diseases were diagnosed in 40,285 (0.098%). The incidence increased from 79.92/100,000 in 2008 to 114.79/100,000 in 2017 (Ptrend < 0.0001). The most frequent was PE (86.5%), followed by AMI (9.6%) and AD (3.3%). The incidence of PE in pregnancy decreased after 2014 and was lower than AMI and AD, while its incidence in puerperium was higher than AMI and AD consistently (Ptrend < 0.0001). Subgroup analysis showed the incidence of these diseases was higher in black women, lowest-income households, and elderly parturients (Ptrend < 0.0001). The mortality decreased from 2.24% in 2008 to 2.21% in 2017 (Ptrend = 0.0240), exhibiting 200-fold higher than patients without these diseases. The following factors were significantly associated with these diseases: aged ≥ 45 years (OR, 4.25; 95%CI, 3.80–4.75), valvular disease (OR, 10.20; 95%CI, 9.73–10.70), and metastatic cancer (OR, 9.75; 95%CI, 7.78–12.22). The trend of elderly parturients increased from 14.94% in 2008 to 17.81% in 2017 (Ptrend < 0.0001), while no such up-trend was found in valvular disease and metastatic cancer.
Conclusion: The incidence of acute high-risk chest pain diseases, especially PE in puerperium, increased consistently. Although mortality has shown a downward trend, it is still at a high level. We should strengthen monitoring and management of acute high-risk pain diseases in pregnancy and puerperium, especially for black women, lowest-income households, and elderly parturients in the future.
Highlights
– The incidence of acute high-risk chest pain diseases, especially PE in the puerperium, increased consistently. Among the three diseases, the most frequent disease was PE, almost 10-fold higher than AMI and 26-fold higher than AD.
– The mortality of acute high-risk chest pain diseases slightly decreased from 2.24% in 2008 to 2.21% in 2017, exhibiting 200-fold higher than patients without these diseases. Although mortality has shown a downward trend, it’s still at a high level.
– We highlight that black women, lowest-income households, and advanced maternal age are the risk factors for acute high-risk chest pain diseases during pregnancy and puerperium. Advanced maternal age is a significant risk factor for acute high-risk chest pain diseases, and the number of elderly parturients is still growing. Reducing health care disparities is a huge project for the government and health care system, but at least now, we could increase physician awareness of these high-risk patients.
Introduction
Acute high-risk chest pain diseases, including acute myocardial infarction (AMI), aortic dissection (AD), and pulmonary embolism (PE), are the major cardiovascular diseases leading to high morbidity and mortality worldwide (1). AMI, AD, and PE have usually been studied and managed as three different diseases. During pregnancy and puerperium, these diseases have a closer relationship involving some common underlying pathophysiological mechanisms (2). Compared with non-pregnant women, pregnant women face a several-fold higher risk of acute high-risk chest pain diseases with potentially devastating outcomes for both the mother and the fetus or baby (3, 4).
Pregnancy puts women into a hypercoagulable state and changes the hemodynamics of the cardiovascular system significantly. In addition, hypertension and diabetes contribute to an increase in the risk of cardiovascular diseases during pregnancy. These risks extend for several months, even into the puerperium period. Acute high-risk chest pain diseases are the leading causes of maternal death in developed countries (5, 6). Early diagnosis and treatment of acute high-risk chest pain diseases are crucial for reducing morbidity and mortality in pregnancy and puerperium.
Much of the previous research focused on just one of the acute high-risk chest pain diseases in pregnancy. Comparing the three diseases and investigating the differences between pregnancy and puerperium are particularly challenging because of the low incidence and heterogeneous clinical presentations. To address these knowledge gaps, we utilized the Nationwide Inpatient Sample (NIS) database to evaluate the incidence, outcomes and risk factors of acute high-risk chest pain diseases during pregnancy and puerperium.
Materials and methods
Data source
The NIS database was queried for all patients during pregnancy and puerperium (6 weeks after delivery) between January 1, 2008, to December 31, 2017. The NIS is the largest publicly available all-payer database in the United States which was collected and cleaned by the Healthcare Cost and Utilization Project (HCUP), capturing approximately 20% of inpatient hospitalizations from all community hospitals (7). According to the guidelines of the HCUP, this study does not require Ethical approval because all data from the NIS were de-identified.
Study population
Of all 371,604,379 patients contained in the NIS between January 1, 2008, to December 31, 2017, all hospitalizations women aged ≥ 18 years who had diagnoses about pregnancy, labor, or postpartum period were identified using the International Classification of Diseases-9th Revision-Clinical Modification (ICD-9-CM) diagnostic or International Classification of Diseases-10th Revision-Clinical Modification (ICD-10-CM) diagnostic. Acute high-risk chest pain diseases were defined as the diagnosis of hospitalizations containing AD, AMI, or PE, identified by ICD-9-CM or ICD-10-CM (Supplementary Table 1). The selection steps are shown in Figure 1. All demographics and the comorbidities of the hospitalizations and hospital-level characteristics were included in our study.
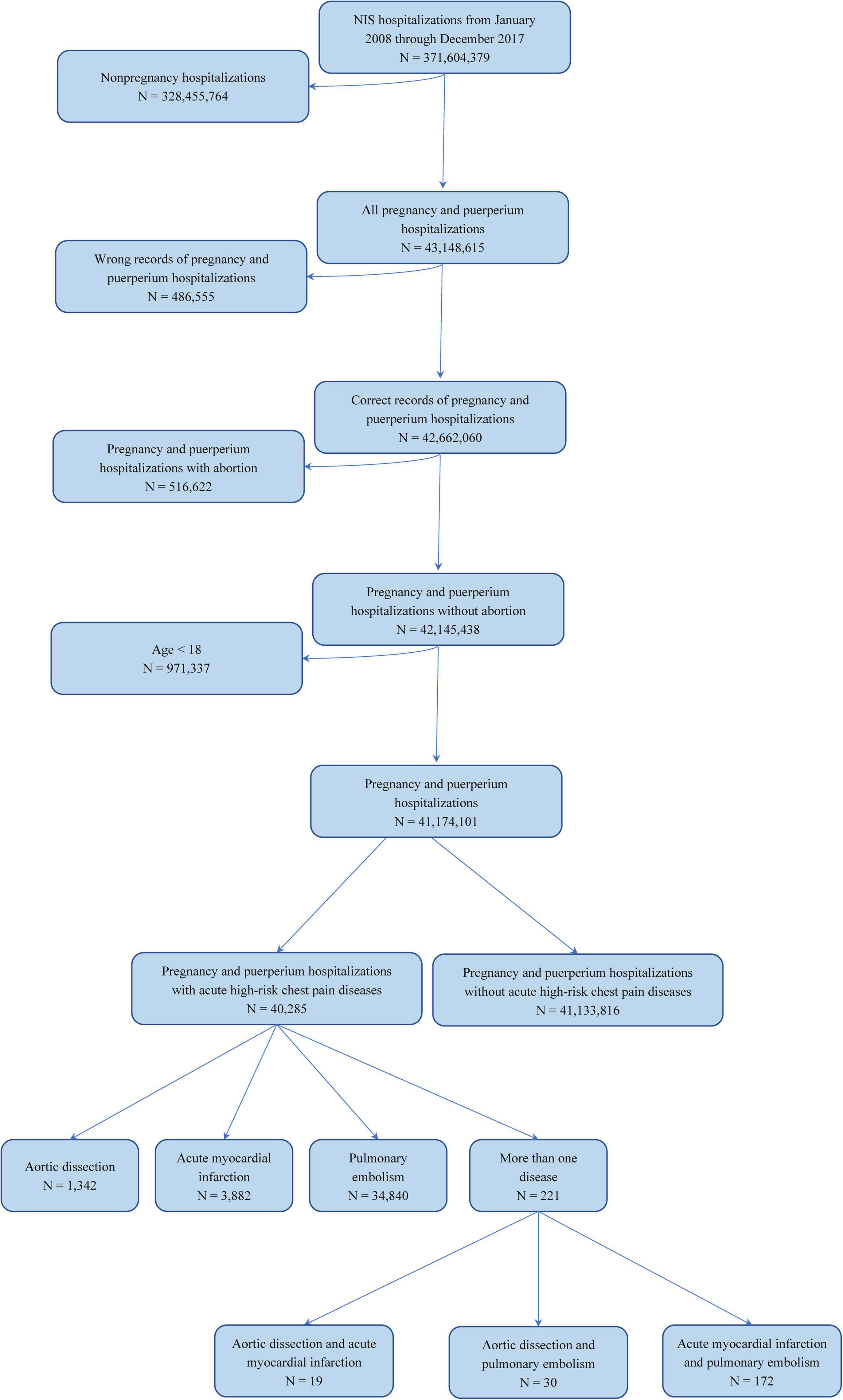
Figure 1. Selection flow diagram of target population. Flow diagram to identify how the study cohort was identified.
Primary and secondary outcomes
The primary outcomes were the temporal trends in the incidence of acute high-risk chest pain diseases during pregnancy and puerperium.
The secondary outcomes included: (1) the temporal trends in the mortality of acute high-risk chest pain diseases during pregnancy and puerperium; (2) risk factors of acute high-risk chest pain diseases during pregnancy and puerperium; (3) the association between acute high-risk chest pain diseases and adverse outcomes, cost, and length of stay (LOS).
Statistical analysis
The characteristics and demographics were compared between patients with and without acute high-risk chest pain diseases. Using weights provided by NIS, we calculated the overall incidence of acute high-risk chest pain diseases during pregnancy and puerperium. Meanwhile, we analyzed the incidence in subgroups, including status (pregnancy or puerperium), race, household income, and age. The Cochran-Armitage trend test was used to evaluate the significance of trends in these diseases over time. Univariate analysis of the comparisons between two groups was determined by Student’s t-test or Mann–Whitney U test for normal distributed or non-normal distributed continuous variables, and Pearson Chi-Square test or Mann–Whitney U test for unordered categorical variable or ordinal categorical variable.
Using the same covariates, logistic models were constructed to explore the relationship between acute high-risk chest pain diseases and adverse outcomes. Model 1 used the data after missing variables imputed, while model 2 used the original data. To avoid the effect of malignancy on mortality, we built model 3 using data excluding patients with metastatic cancer to explore the relationship between acute high-risk chest pain diseases and death. To evaluate whether the diseases related to the cost and LOS of the hospitalization, we constructed multivariate linear models, adjusting for the same covariate assessment as model 1. Univariate and two multivariate logistic models were constructed to explore the clinical factors associated with acute high-risk chest pain diseases and the three diseases as model 1 and model 2 in all cohort and high incidence subgroups. All tests were two-tailed, and P < 0.05 was considered significant unless otherwise specified. Statistical analysis was performed using SAS version 9.4 (SAS Institute Inc.).
Patient and public involvement
Causing of the nature of this study, there were no patients or the public involved around the design, recruitment, measuring, or writing of the research.
Missing variables
Most values were missing for < 2% of all hospitalizations, while race and cost were missing for 9.36% and 2.17% (Supplementary Table 2). The missing data of the categorical variables were imputed by the dominant category and the continuous variables by the median.
Results
Included population
Among 41,174,101 hospitalizations for pregnancy and puerperium from 2008 to 2017, acute high-risk chest pain diseases were diagnosed in 40,285 patients (0.098%). The most frequent disease was PE (N = 34,840, 86.5%), almost 10-fold higher than AMI (N = 3,882, 9.6%) and 26-fold higher than AD (N = 1,342, 3.3%). A total of 221 patients had more than one disease. A comparison of demographics, hospital characteristics, and outcomes between patients with and without acute high-risk chest pain diseases was presented (Table 1). Patients with acute high-risk chest pain diseases were more likely to be older, black individuals, and had higher proportions of coagulopathy, metastatic cancer, and valvular disease.
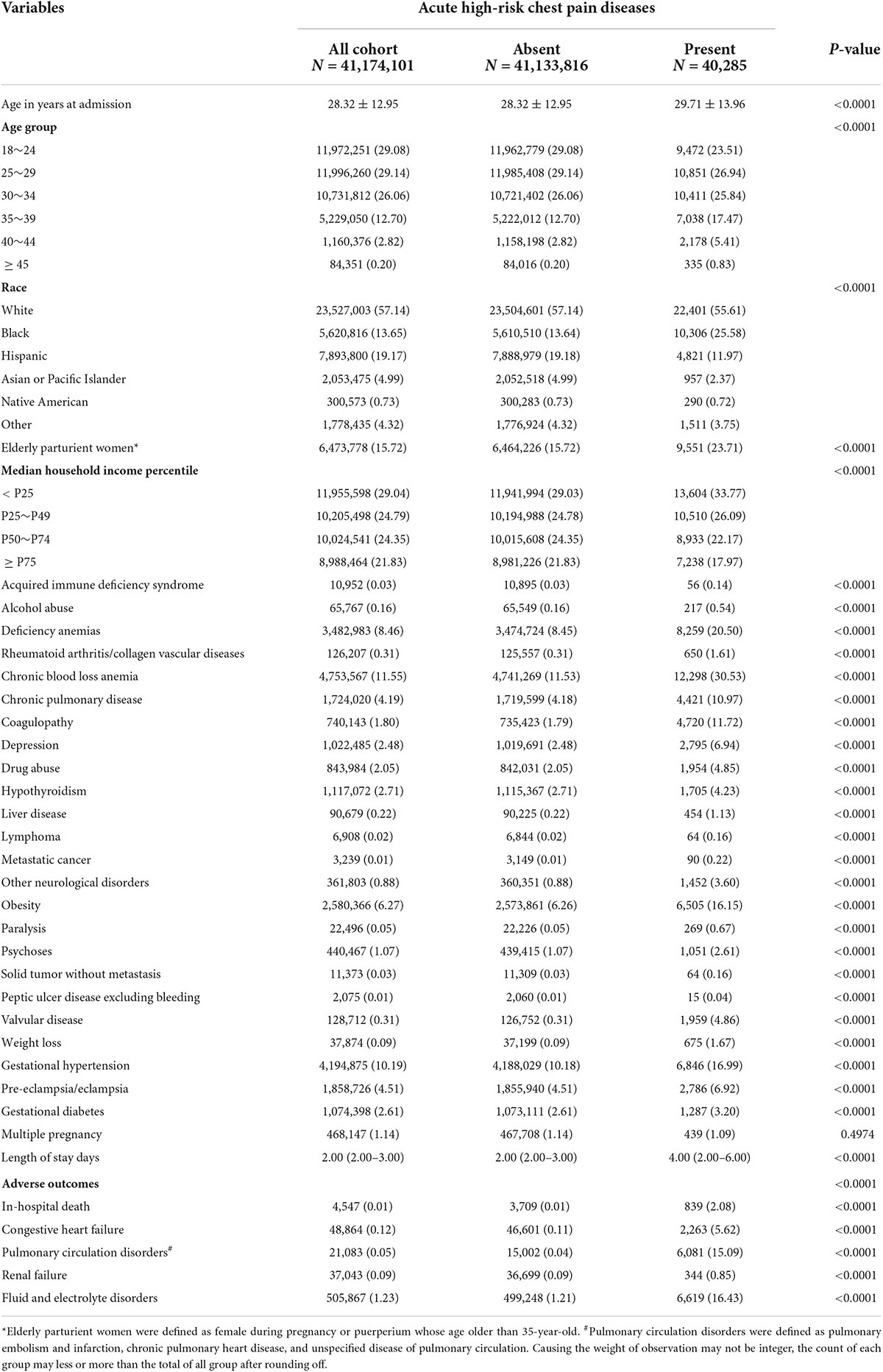
Table 1. Characteristics and outcomes in acute high-risk chest pain diseases during pregnancy and puerperium.
Primary outcomes
As shown in Figure 2A, the incidence of acute high-risk chest pain diseases during pregnancy and puerperium increased from 79.92 per 100,000 hospitalizations in 2008 to 114.79 per 100,000 hospitalizations in 2017 (Ptrend < 0.0001) (Supplementary Table 3). The incidence of these diseases in pregnancy decreased notably since 2015, while the incidence in puerperium increased consistently (Supplementary Table 4). The incidence of PE in pregnancy decreased after 2014 and was lower than AMI and AD, while its incidence in puerperium was significantly higher than AMI and AD (Ptrend < 0.0001). As shown in Figure 2B, the incidence of acute high-risk chest pain diseases in puerperium surpassed that in pregnancy since 2015. The incidence of PE in puerperium increased sustainedly and was consistently higher than that in pregnancy. The incidence of AMI and AD in pregnancy was higher than that in the puerperium, respectively.
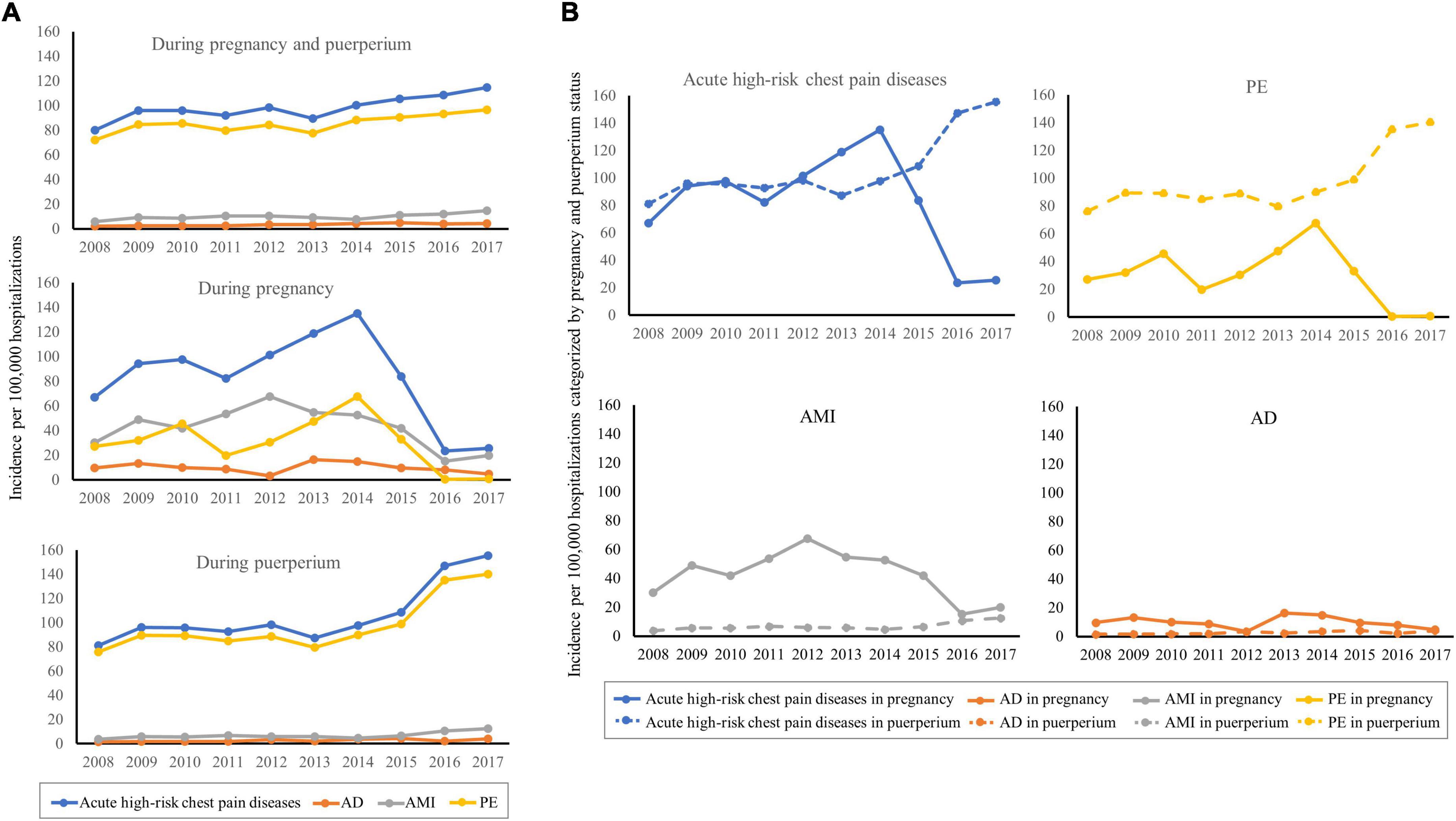
Figure 2. Temporal trends of the incidence in acute high-risk chest pain diseases during pregnancy and puerperium. (A) Temporal trends during pregnancy and puerperium, during pregnancy, and during puerperium, respectively (All Ptrend < 0.0001). (B) Temporal trends of the incidence in acute high-risk chest pain diseases, PE, AMI, and AD categorized by pregnancy and puerperium status (All Ptrend < 0.0001).
As shown in Figures 3A–C, the subgroup analyses categorized by race, household income, and elderly/non-elderly parturients showed that temporal trends of most subgroups increased. Most of them presented with Ptrend < 0.0001 (Supplementary Table 4), except for elderly parturient (Ptrend = 0.0017), Asian or Pacific Islander (Ptrend = 0.0004), other race (Ptrend = 0.0213), household income: P50∼P74 (Ptrend = 0.7509). Black women had the highest incidence, whereas Asian or Pacific Islanders had the lowest incidence. The socio-economic status of patients affected the risk of these diseases. The incidence was highest in the lowest median household income category (0–25th percentile). Elderly parturient women (> 35 years old) were more likely to suffer from these diseases when compared to young women. The incidence increased with age, reaching a peak of 397.28/100,000 hospitalizations at ages over 45 years (Figure 3D).
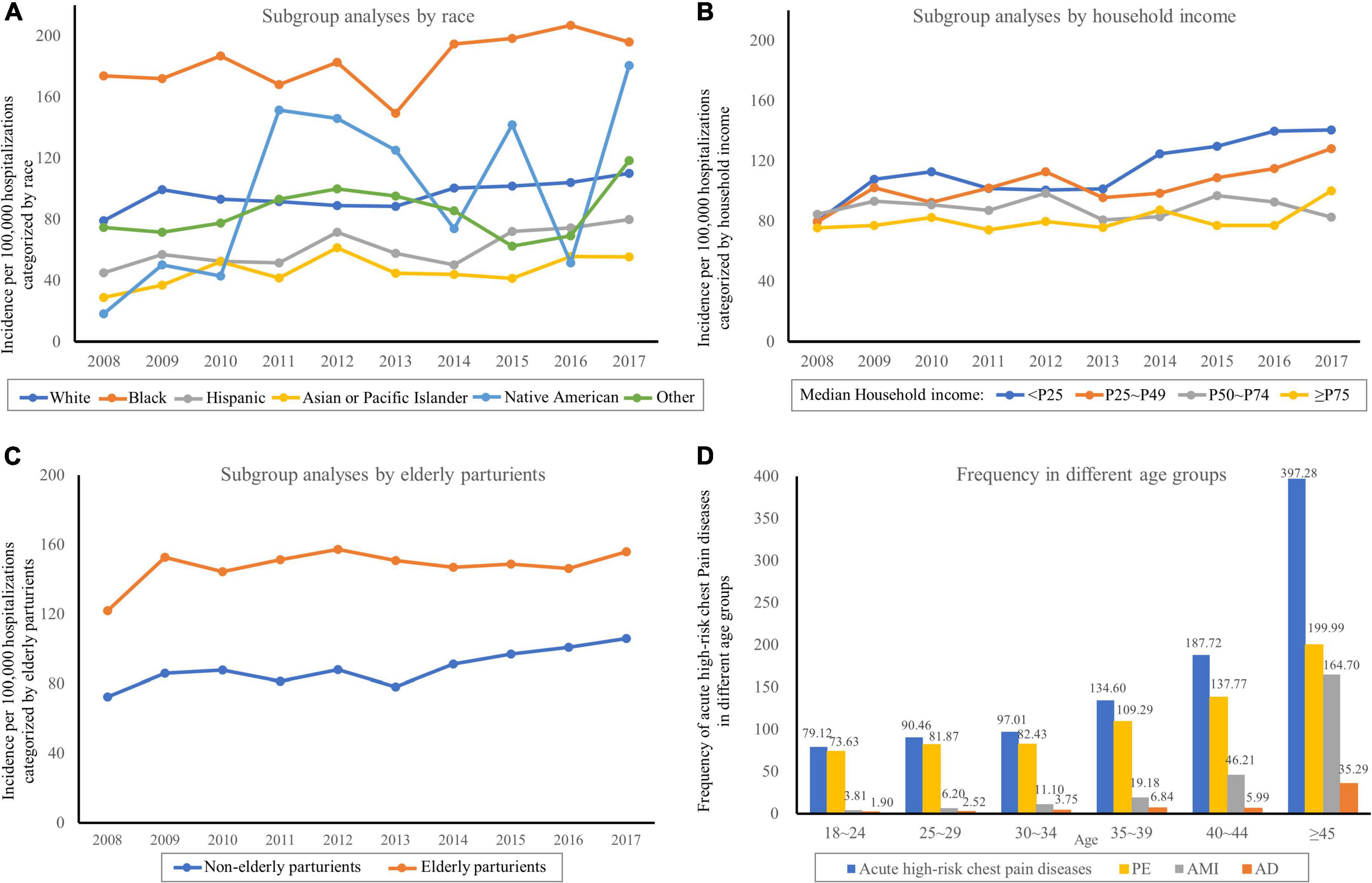
Figure 3. Temporal trends of acute high-risk chest pain diseases in Subgroups. (A) Subgroup analyses categorized by race. (B) Subgroup analyses categorized by household income. (C) Subgroup analyses categorized by elderly parturients. (D) The incidence increased with age.
Secondary outcomes
A total of 839 (2.08%) hospitalizations with acute high-risk chest pain diseases died, while the death rate of patients without these diseases was just 0.01% (Table 1). During the study period, the mortality of these diseases mildly decreased but remained high (2.24% in 2008 vs. 2.21% in 2017; Ptrend = 0.0240) (Supplementary Table 5 and Figure 4). The mortality of AMI decreased from 5.51% in 2008 to 2.56% in 2017 (Ptrend < 0.0001), while the trends in AD and PE were not statistically significant. Acute high-risk chest pain diseases were associated with an increased cost of $35,789 and an increased LOS of 2.488 days after adjustment confounders (Supplementary Table 6).
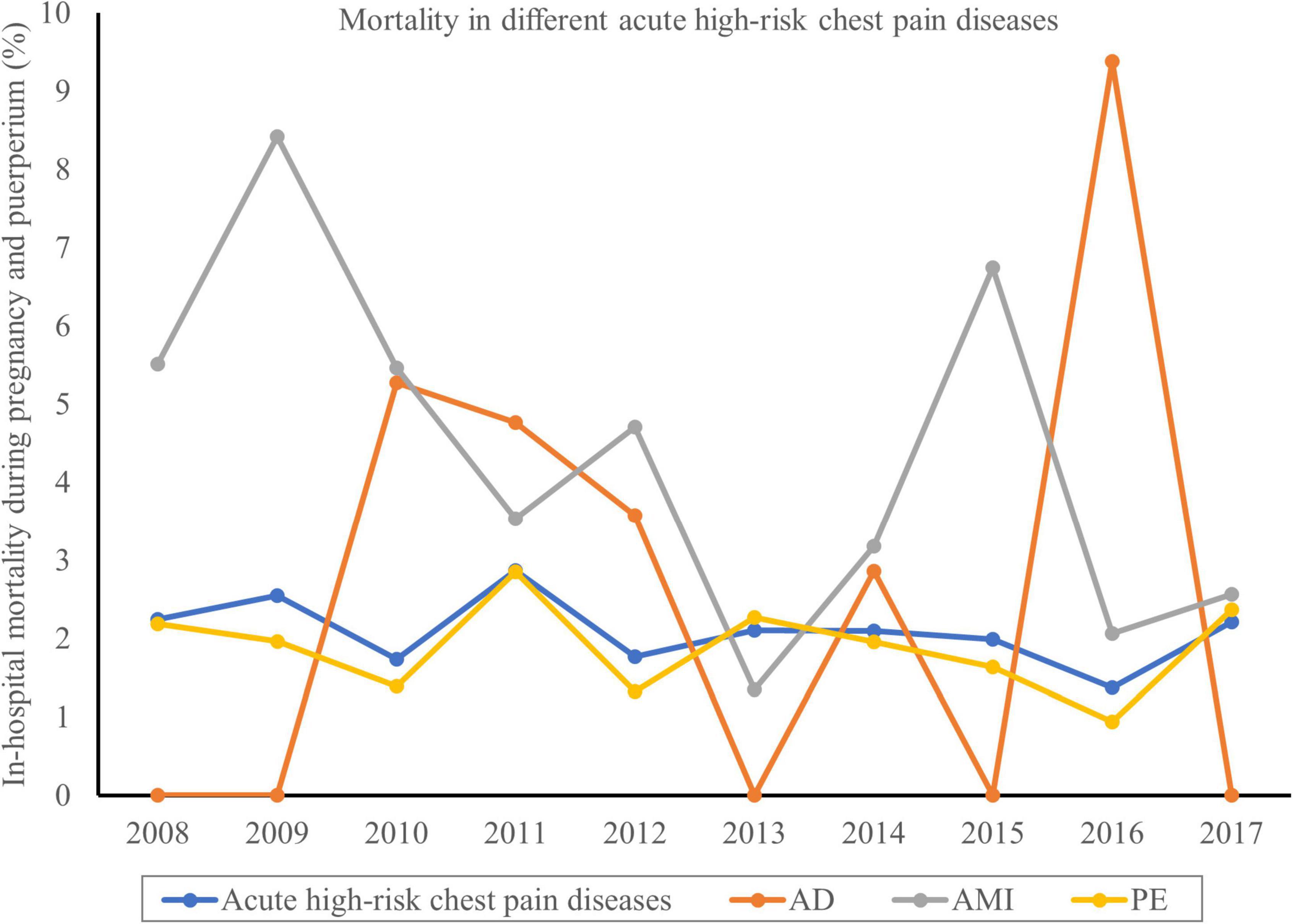
Figure 4. Temporal trends of the mortality in acute high-risk chest pain diseases during pregnancy and puerperium. The in-hospital mortality of acute high-risk chest pain diseases mildly decreased but still remained high (2.24% in 2008 vs. 2.21% in 2017; Ptrend = 0.0240).
After excluding the effect of metastatic cancer on mortality, acute high-risk chest pain diseases were significantly associated with increased in-hospital death (OR, 57.42; 95%CI, 52.43–62.87; Supplementary Table 7). Acute high-risk chest pain diseases were also associated with pulmonary circulation disorders (OR, 255.96; 95%CI, 246.32–265.97; Supplementary Table 8), congestive heart failure (OR, 13.80; 95%CI, 13.09–14.56; Supplementary Table 9), renal failure (OR, 2.80; 95%CI, 2.50–3.14; Supplementary Table 10) and fluid and electrolyte disorders (OR, 8.06; 95%CI, 7.82–8.30; Supplementary Table 11).
The following factors were independently associated with acute high-risk chest pain diseases: over 45 years old (OR, 4.25; 95%CI, 3.80–4.75), valvular disease (OR, 10.20; 95%CI, 9.73–10.70), and metastatic cancer (OR, 9.75; 95%CI, 7.78–12.22) (Table 2). In the further analysis of clinical factors associated with AD, we found that over 45 years old (OR, 7.55; 95%CI, 5.06–11.26) and valvular disease (OR, 86.48; 95%CI, 76.77–97.43) were highly associated with the onset of disease (Supplementary Table 12). The following factors were highly associated with AMI, including over 45 years old (OR, 33.14; 95%CI, 27.16–40.43), valvular disease (OR, 16.82; 95%CI, 15.08–18.76), and metastatic cancer (OR, 11.83; 95%CI, 7.07–19.78) (Supplementary Table 13). The following factors were highly associated with PE, including over 45 years old (OR, 2.34; 95%CI, 2.00–2.73), coagulopathy (OR, 5.23; 95%CI, 5.06–5.41), valvular disease (OR, 6.78; 95%CI, 6.38–7.21) and metastatic cancer (OR, 10.22; 95%CI, 8.05–12.98) (Supplementary Table 14).
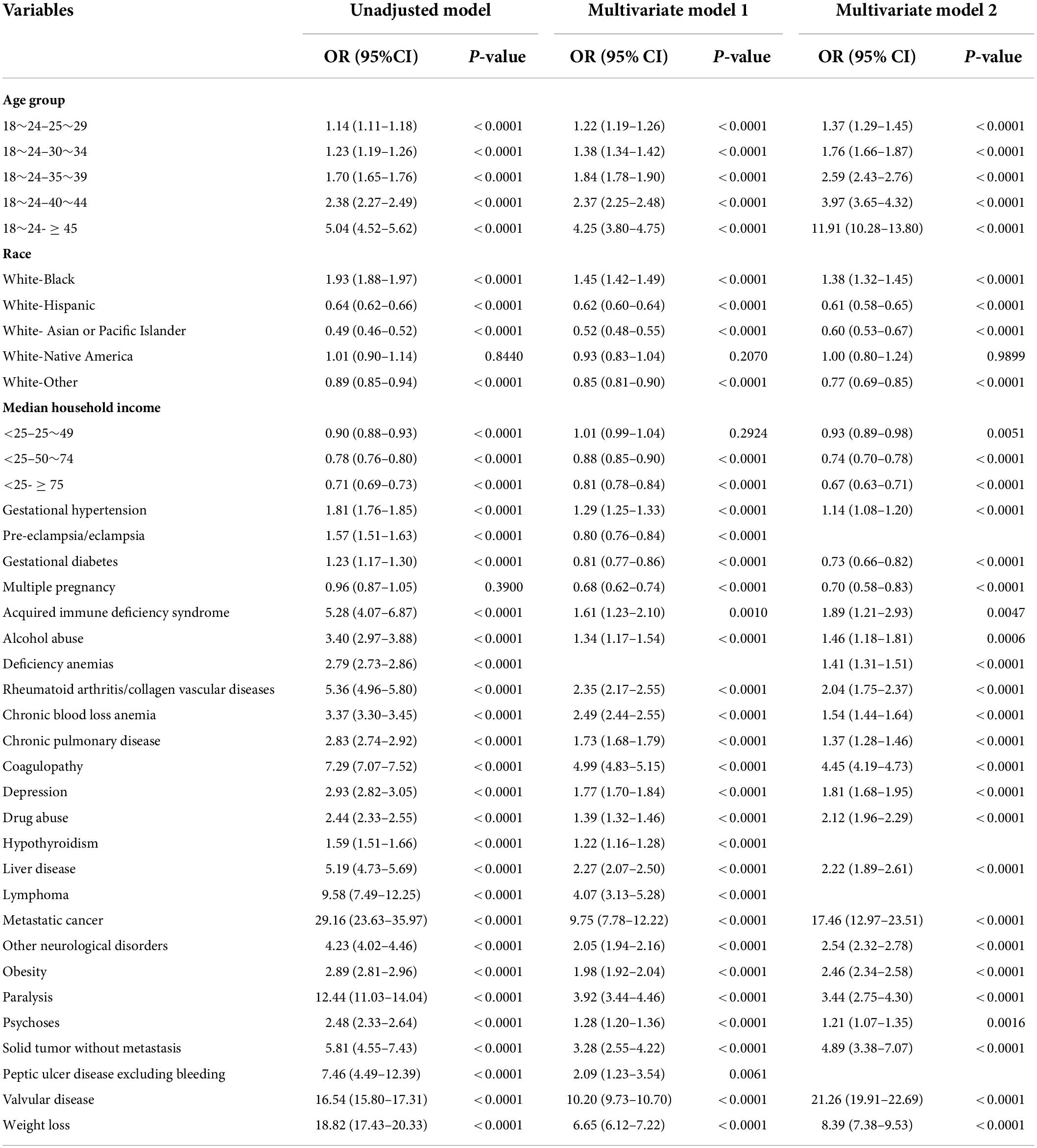
Table 2. Association of clinical factors with acute high-risk chest pain diseases during pregnancy and puerperium.
The trends of most clinical factors increased from 2008 to 2017 (all Ptrend < 0.0001, Supplementary Table 15), except valvular disease, lymphoma, and metastatic cancer. The trend of elderly parturients increased from 14.94% in 2008 to 17.81% in 2017 (Ptrend < 0.0001).
Discussion
In this nationwide observational analysis of 41,174,101 hospitalizations for pregnancy and puerperium from 2008 to 2017, acute high-risk chest pain diseases were diagnosed in 40,285 patients (0.098%). The incidence increased from 79.92/100,000 in 2008 to 114.79/100,000 in 2017. The incidence of acute high-risk chest pain diseases in puerperium consistently increased and even surpassed the incidence in pregnancy since 2015. Among the three diseases, the most frequent disease was PE, almost 10-fold higher than AMI and 26-fold higher than AD. The incidence of PE in puerperium increased consistently and was significantly higher than that in pregnancy. The high portion of PE among the three diseases and its increased incidence in puerperium lead to the overall upward trend of acute high-risk chest pain diseases in puerperium. The mortality of acute high-risk chest pain diseases slightly decreased from 2.24% in 2008 to 2.21% in 2017, exhibiting 200-fold higher than patients without these diseases. The following factors were significantly associated with acute high-risk chest pain diseases: aged ≥ 45 years (OR, 4.25; 95%CI, 3.80–4.75), valvular disease (OR, 10.20; 95%CI, 9.73–10.70), and metastatic cancer (OR, 9.75; 95%CI, 7.78–12.22). The trend of elderly parturients increased from 14.94% in 2008 to 17.81% in 2017 (Ptrend < 0.0001), while no such up-trend was found in valvular disease and metastatic cancer.
Pregnancy is a hypercoagulable state characterized by increased prothrombotic factors. In addition, dilated veins, decreased or obstructed venous flow by the enlarging uterus lead to deep vein thrombosis and pregnancy-related PE. PE is the first leading cause of maternal death in the United Kingdom and the sixth in the United States (8, 9). In our data, the incidence of PE was 0.0846% and was significantly higher than AD and AMI. The incidence we presented was mildly higher than the previously reported incidence of 0.03% (5). Elgendy et al. (10) reported that the incidence of PE remained unchanged from 2007 to 2015. We found that the incidence of PE in puerperium increased consistently from 2008 to 2017 and was significantly higher than that in pregnancy. This can be due to multiple reasons. First, not only the PE, but we also observed a decrease in AMI and AD during pregnancy. We believe this results from adequate attention to these diseases during pregnancy over the past 20 years. Second, vascular trauma, assistive devices, and cesarean section heighten postpartum thrombotic risk during delivery (11). The risk of venous thromboembolism increases in the immediate postpartum period and returns to the non-pregnant level until the sixth week postpartum (5). In a previous population-based study from 1966 to 1995, the postpartum period was also found to be the highest risk period for PE (3). We confirmed the high risk of PE in puerperium and demonstrated its continuous upward trend from 2008 to 2017. Management of PE in puerperium may not be given sufficient attention after discharge and should be strengthened in the future.
Mechanisms of AMI in pregnancy include plaque rupture or erosion, coronary dissection, and thrombus (12, 13). In our data, the incidence of AMI during pregnancy and puerperium increased from 5.9/100,000 in 2008 to 14.8/100,000 in 2017. Similar findings reported that the incidence of AMI in pregnancy and puerperium increased from 7.1/100,000 in 2002 to 9.5/100,000 in 2014 (Ptrend < 0.001) (14). Accordingly, we concluded that the incidence of AMI increased from 2002 to 2017. Moreover, we could not ignore that some women with suspected AMI during pregnancy did not undergo coronary angiography for radiation risks to the mother and fetus. In addition, detailed angiographic findings or intracoronary imaging results were not available for patients who underwent invasive management due to the limitation of ICD-9/10 codes from the NIS data set. We could not identify the mechanisms of AMI from the available data. The true incidence and mechanisms of AMI during pregnancy and puerperium warrants further exploration.
In our study, the incidence of AD in pregnancy and puerperium was 0.003%, which was the lowest among the three diseases. The rate of AD in pregnancy was reported at 0.0004% between 1998 and 2008, representing 0.1% of all cases of AD (15). Population-based studies demonstrated a similarly rare AD occurrence in pregnancy (16, 17). Although rare, the incidence of AD has increased in the past 20 years. We believe that the period of pregnancy and puerperium are portended independent risk time for AD. During pregnancy, high cardiac output, hormonal changes, gestational hypertension, hereditary connective tissue diseases, coarctation of the aorta, and previous aortic surgery increase AD susceptibility (18–20). Sometimes, AD symptoms may mimic AMI and PE, resulting in inadvertent use of antiplatelet and anticoagulant therapy and devastating outcomes. Thus, we must always maintain a strong suspicion of high-risk women prone to AD during pregnancy and puerperium.
The increasing incidences of acute high-risk chest pain diseases indicate we must identify the risk factors behind the rise, including modifiable and unmodifiable factors. Previous population-based studies reported that maternal age, hypertension, and diabetes were independent risk factors associated with AMI during pregnancy (4, 21). We observed a consistently higher incidence of acute high-risk chest pain diseases in the elderly (> 35 years old) than non-elderly parturient women. The incidence increased with age, reaching a peak of 397.28/100,000 hospitalizations at ages over 45 years. In the multivariable analysis, age over 45 was closely related to acute high-risk chest pain diseases (OR, 4.25; 95%CI, 3.80–4.75). Compared with AD (OR, 7.55; 95%CI, 5.06–11.26) and PE (OR, 2.34; 95%CI, 2.00–2.73), age over 45 years old was significantly associated with AMI (OR, 33.14; 95%CI, 27.16–40.43). A previous study reported that advanced maternal age was closely related to AMI, with up to 30-fold odds in pregnant women aged ≥ 40 than women < 20 years (4, 22). These data are in agreement with our results. We also found that the trend of elderly parturients increased from 14.94% in 2008 to 17.81% in 2017 (Ptrend < 0.0001). Our findings highlight that advanced maternal age is a significant risk factor for acute high-risk chest pain diseases, especially AMI, and the number of elderly parturients is still increasing. The upward trend in the number of elderly parturients is of concern. Maternal health policies should focus on advanced maternal age pregnancies in the future.
Besides age, race is another unmodifiable factor for acute high-risk chest pain diseases. Previous studies reported that the black race was independently associated with AMI during pregnancy and puerperium (12, 14). In pregnant women with PE, the black race was contributed to a higher proportion of deaths than white women from 2007 to 2016 (23). In our study, black women were significantly associated with acute high-risk chest pain diseases (OR, 1.44; 95% CI, 1.40–1.48). In the multivariable analysis of each disease, the black race was highly associated with AMI (OR, 1.65; 95%CI, 1.52–1.79) and PE (OR, 1.48; 95%CI, 1.44–1.52). Compared with white women, black women had a low risk of AD (OR, 0.53; 95%CI, 0.45–0.63), while native Americans were highly associated with AD (OR, 1.56; 95%CI, 0.99–2.47). However, due to the rare incidence of AD in pregnancy, the association between race and AD warrants further investigation. The socio-economic status of patients also affected the risk of acute high-risk chest pain diseases. The incidence was highest in the lowest median household income category (0 to 25th percentile). Our study may inform interventions to promote health equity for patients with the lowest median household income. Reducing health care disparities is a huge project for the government and health care system, but at least now, we could increase physician awareness of these high-risk patients.
In multivariable analysis, valvular disease (OR, 10.20; 95%CI, 9.73–10.70) and metastatic cancer (OR, 9.75; 95%CI, 7.78–12.22) were independently associated with acute high-risk chest pain diseases. The valvular disease can be rheumatic, congenital, or degenerative during pregnancy (5). In particular, valvular disease was significantly associated with AD (OR, 86.48; 95%CI, 76.77–97.43). Valvular disease is a common cause inducing AD. Pregnant woman with valvular diseases, especially aortic stenosis and regurgitation, is at increased risk for aortic aneurysms and AD (24). Malignancy is a primary reason leading to coagulation system activation (25). In turn, coagulation activation and platelet aggregation might facilitate metastasis. Our study found that metastatic cancer was significantly related to AMI (OR, 11.83; 95%CI, 7.07–19.78) and PE (OR, 10.22; 95%CI, 8.05–12.98), and there was no association between metastatic cancer and AD.
Moreover, we found that gestational hypertension was positively associated with acute high-risk chest pain diseases (OR, 1.29; 95%CI, 1.25–1.33) while gestational diabetes was negatively associated with acute high-risk chest pain diseases (OR, 0.81; 95%CI, 0.77–0.86). The incidence of driving risk factors is different in different races and regions, which makes the occurrence of diseases in various manners. Asians and Pacific Islanders comprise 5% of the total population in the United States and have a high incidence of gestational diabetes. However, we found that Asian and Pacific Islanders had the lowest incidence of acute high-risk chest pain diseases, whereas black women had the highest incidence. Our study seems inconsistent with previous findings that hypertension and diabetes are strong risk factors for cardiovascular diseases. We speculate that patients with gestational hypertension or diabetes might attract more attention due to the high risk leading to cardiovascular complications and thus improve outcomes in these patients. Taken together, the interaction of risk factors and concomitant diseases can lead to the development of acute high-risk chest pain diseases. Management of risk factors and concomitant diseases may reduce the incidence of acute high-risk chest pain diseases in pregnant or puerperal women.
In brief, we highlight that black women, lowest-income households, advanced maternal age, valvular disease, and metastatic cancer are the risk factors of acute high-risk chest pain diseases during pregnancy and puerperium. The trend of elderly parturients increased from 2008 to 2017, while no such up-trend was found in valvular disease and metastatic cancer. A recent survey has revealed that cardiovascular disease is the leading cause of pregnancy-related deaths in the United States, accounting for 15.5% of all pregnancy-related deaths from 2014 to 2017 (9). In our study, acute high-risk chest pain diseases were significantly associated with increased in-hospital death after excluding the effect of metastatic cancer. Although the mortality has shown a downward trend (2.24% in 2008 vs. 2.21% in 2017), it is still at a high level with a 200-fold higher risk. Among these diseases, the mortality of AMI decreased from 5.51% in 2008 to 2.56% in 2017. No such trend was found in AD and PE patients. Thus, more efforts should be made to reduce mortality among these populations. Sufficient attention should be paid to patients presenting chest pain during pregnancy and puerperium, especially for black women, lowest-income households, and elderly parturients.
Limitations
Despite its strengths, there are several limitations to the current analysis. First, limited by the data elements of the NIS database, some vital information such as medication administration, procedural details, and genetic testing are not collected, which may cause bias in outcome evaluation. Second, it should be noted that approximately one-third of pregnancy-related deaths occurred outside a medical facility (26). These patients who died outside the hospital would not be reported in the NIS and represent missing data. Third, the NIS database is representative of the American population. The incidence of driving risk factors is different in different races and regions. Our results may not be generalized to the populations outside the United States. Fourth, due to the low incidence of AD, there were only 1,342 patients queried from the database, which may lead to dramatic fluctuations in mortality and biased estimates of overall trends. Fifth, the diagnoses of each disease relying on ICD codes may have coding errors and cannot be confirmed from standard criteria. Sixth, there is a coding shift from ICD-9 to ICD-10 in 2015. Considering this, we queried the variables to be included in the initial trial design process of the study with ICD-9 and ICD-10 respectively, achieving one-to-one correspondence and all relevant codes included as possible. Despite these limitations, our study offers essential information on acute high-risk chest pain diseases using a nationally representative sample of women during pregnancy and puerperium. This database reflects the current real-world practice and avoids the potential biases originating from specialized centers.
Conclusion
In conclusion, we found that the incidence of acute high-risk chest pain diseases in puerperium consistently increased during the study period and even surpassed the incidence in pregnancy since 2015. The most frequent disease was PE, and the incidence of PE in puerperium increased consistently. Although the mortality of acute high-risk chest pain diseases has shown a downward trend, it is still at a high level with a 200-fold higher risk. Advanced maternal age is a significant risk factor for acute high-risk chest pain diseases, and the number of elderly parturients is still growing. We should strengthen monitoring and management of acute high-risk pain diseases in pregnancy and puerperium, especially for black women, lowest-income households, and elderly parturients in the future.
Data availability statement
The original contributions presented in this study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
SW, XX, QH, YQ, RW, JC, and CC had full access to the data and verified the data. SL and CW were responsible for the decision to submit the manuscript and contributed to the concept, design, and supervision. SW and XX drafted the manuscript. QH, YQ, and RW contributed to the statistical analysis. All authors contributed to critical revision of the manuscript for important intellectual content.
Funding
This work was supported by 3-Year Action Plan for Strengthening Public Health System in Shanghai (2020–2022) Subject Chief Scientist (GWV-10.2-XD05), National Natural Science Foundation of China (No. 82003558), and Shanghai Science and Technology Development Funds (22QA1411400).
Acknowledgments
The data underlying this article were provided by NIS database under license to the Navy Medical University.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2022.968964/full#supplementary-material
References
1. Bautz B, Schneider JI. High-risk chief complaints I: Chest pain-the big three (an update). Emerg Med Clin N Am. (2020) 38:453–98. doi: 10.1016/j.emc.2020.01.009
2. Ramlakhan KP, Johnson MR, Roos-Hesselink JW. Pregnancy and cardiovascular disease. Nat Rev Cardiol. (2020) 17:718–31. doi: 10.1038/s41569-020-0390-z
3. Heit JA, Kobbervig CE, James AH, Petterson TM, Bailey KR, Melton LJ III. Trends in the incidence of venous thromboembolism during pregnancy or postpartum: A 30-year population-based study. Ann Intern Med. (2005) 143:697–706. doi: 10.7326/0003-4819-143-10-200511150-00006
4. James AH, Jamison MG, Biswas MS, Brancazio LR, Swamy GK, Myers ER. Acute myocardial infarction in pregnancy: A united states population-based study. Circulation. (2006) 113:1564–71. doi: 10.1161/CIRCULATIONAHA.105.576751
5. Regitz-Zagrosek V, Roos-Hesselink JW, Bauersachs J, Blomstrom-Lundqvist C, Cifkova R, De Bonis M, et al. 2018 Esc guidelines for the management of cardiovascular diseases during pregnancy. Eur Heart J. (2018) 39:3165–241. doi: 10.1093/eurheartj/ehy340
6. Mehta LS, Warnes CA, Bradley E, Burton T, Economy K, Mehran R, et al. Cardiovascular considerations in caring for pregnant patients: A scientific statement from the American heart association. Circulation. (2020) 141:e884–903. doi: 10.1161/CIR.0000000000000772
8. Konstantinides SV, Meyer G, Becattini C, Bueno H, Geersing GJ, Harjola VP, et al. 2019 Esc guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European respiratory society (Ers). Eur Heart J. (2020) 41:543–603. doi: 10.1093/eurheartj/ehz405
9. Centers for Disease Control and Prevention. Pregnancy mortality surveillance system. Atlanta, GA: Centers for Disease Control and Prevention (2021).
10. Elgendy IY, Gad MM, Mansoor H, Mahmoud AN, Elbadawi A, Saad A, et al. Acute pulmonary embolism during pregnancy and puerperium: National trends and in-hospital outcomes. Mayo Clin Proc. (2021) 96:2102–13. doi: 10.1016/j.mayocp.2021.01.015
11. Nichols KM, Henkin S, Creager MA. Venous thromboembolism associated with pregnancy: JACC focus seminar. J Am Coll Cardiol. (2020) 76:2128–41. doi: 10.1016/j.jacc.2020.06.090
12. Balgobin CA, Zhang X, Lima FV, Avila C, Parikh PB, Yang J, et al. Risk factors and timing of acute myocardial infarction associated with pregnancy: Insights from the national inpatient sample. J Am Heart Assoc. (2020) 9:e016623. doi: 10.1161/JAHA.120.016623
13. Saw J, Mancini GBJ, Humphries KH. Contemporary review on spontaneous coronary artery dissection. J Am Coll Cardiol. (2016) 68:297–312. doi: 10.1016/j.jacc.2016.05.034
14. Smilowitz NR, Gupta N, Guo Y, Zhong J, Weinberg CR, Reynolds HR, et al. Acute myocardial infarction during pregnancy and the puerperium in the United States. Mayo Clin Proc. (2018) 93:1404–14. doi: 10.1016/j.mayocp.2018.04.019
15. Sawlani N, Shroff A, Vidovich MI. Aortic dissection and mortality associated with pregnancy in the United States. J Am Coll Cardiol. (2015) 65:1600–1. doi: 10.1016/j.jacc.2014.12.066
16. Thalmann M, Sodeck GH, Domanovits H, Grassberger M, Loewe C, Grimm M, et al. Acute type a aortic dissection and pregnancy: A population-based study. Eur J Cardiothorac Surg. (2011) 39:e159–63. doi: 10.1016/j.ejcts.2010.12.070
17. Nienaber CA, Fattori R, Mehta RH, Richartz BM, Evangelista A, Petzsch M, et al. Gender-related differences in acute aortic dissection. Circulation. (2004) 109:3014–21. doi: 10.1161/01.CIR.0000130644.78677.2C
18. Evangelista A, Isselbacher EM, Bossone E, Gleason TG, Eusanio MD, Sechtem U, et al. Insights from the international registry of acute aortic dissection: A 20-year experience of collaborative clinical research. Circulation. (2018) 137:1846–60. doi: 10.1161/CIRCULATIONAHA.117.031264
19. Kamel H, Roman MJ, Pitcher A, Devereux RB. Pregnancy and the risk of aortic dissection or rupture: A cohort-crossover analysis. Circulation. (2016) 134:527–33. doi: 10.1161/CIRCULATIONAHA.116.021594
20. Poniedzialek-Czajkowska E, Sadowska A, Mierzynski R, Leszczynska-Gorzelak B. Aortic dissection during pregnancy – obstetric perspective. Ginekol Pol. (2019) 90:346–50. doi: 10.5603/GP.2019.0052
21. Ladner HE, Danielsen B, Gilbert WM. Acute myocardial infarction in pregnancy and the puerperium: A population-based study. Obstet Gynecol. (2005) 105:480–4. doi: 10.1097/01.AOG.0000151998.50852.31
22. Roth A, Elkayam U. Acute myocardial infarction associated with pregnancy. J Am Coll Cardiol. (2008) 52:171–80. doi: 10.1016/j.jacc.2008.03.049
23. Petersen EE, Davis NL, Goodman D, Cox S, Syverson C, Seed K, et al. Racial/ethnic disparities in pregnancy-related deaths – United States, 2007-2016. Morb Mortal Wkly Rep. (2019) 68:762–5. doi: 10.15585/mmwr.mm6835a3
24. Goldfinger JZ, Halperin JL, Marin ML, Stewart AS, Eagle KA, Fuster V. Thoracic aortic aneurysm and dissection. J Am Coll Cardiol. (2014) 64:1725–39. doi: 10.1016/j.jacc.2014.08.025
25. Stein PD, Beemath A, Meyers FA, Skaf E, Sanchez J, Olson RE. Incidence of venous thromboembolism in patients hospitalized with cancer. Am J Med. (2006) 119:60–8. doi: 10.1016/j.amjmed.2005.06.058
Keywords: acute myocardial infarction, aortic dissection, pulmonary embolism, pregnancy, puerperium
Citation: Wu S, Xu X, He Q, Qin Y, Wang R, Chen J, Chen C, Wu C and Liu S (2022) Incidence and outcomes of acute high-risk chest pain diseases during pregnancy and puerperium. Front. Cardiovasc. Med. 9:968964. doi: 10.3389/fcvm.2022.968964
Received: 14 June 2022; Accepted: 14 July 2022;
Published: 11 August 2022.
Edited by:
Rajeev Gupta, Medicilinic, United Arab EmiratesReviewed by:
Magdy Elmasry, Tanta University, EgyptSivasankaran Sivasubramonian, Sree Chitra Tirunal Institute for Medical Sciences and Technology (SCTIMST), India
Copyright © 2022 Wu, Xu, He, Qin, Wang, Chen, Chen, Wu and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Cheng Wu, wucheng@smmu.edu.cn; Suxuan Liu, suxuan.liu@qq.com
†These authors have contributed equally to this work and share first authorship
‡These authors have contributed equally to this work
 Shengyong Wu1†
Shengyong Wu1†  Xudong Xu
Xudong Xu Qian He
Qian He Yingyi Qin
Yingyi Qin Chenxin Chen
Chenxin Chen Suxuan Liu
Suxuan Liu