Presurgical techniques for the treatment of cleft lip and palate in infants – a review of the literature
Abstract
Patients with cleft lip and palate require long-term, multistage and multidisciplinary treatment whose first step is presurgical orthopaedic (PSO) treatment. The reconstruction of the lip, alveolar process and nose in these patients are major plastic surgery challenges. Various presurgical procedures are undertaken to achieve optimal surgical outcomes. The aim of this article is to present selected techniques for the presurgical cleft lip and palate treatment in infants and critically evaluate the benefits, limitations and drawbacks of the methods used. The research was based on the literature review using keywords: presurgical treatment of cleft lip and palate in infants, presurgical orthopaedics in the treatment of cleft lip and palate in infants in PubMed, Google Scholar databases, and publications in orthodontics and infant orthopaedics out of these databases. PSO is a minimally invasive therapy performed between birth and first surgery. Anatomical and functional cleft palate disorders constitute indications for PSO. There are positive reports on PSO techniques and some of them can be implemented by the child’s caregivers at home. The authors of studies disagree on the PSO effectiveness. The lack of long-term research results, high costs of therapy and few therapy centres negatively influence the decision to undertake the therapy.
Citation
Górska J., Kalinowska J., Racka-Pilszak B. Presurgical techniques for the treatment of cleft lip and palate in infants – a review of the literature Eur J Transl Clin Med 2022;5(2)67-74Introduction
Cleft lip and palate is one of the most common developmental defects, which manifests as an anatomical discontinuity and underdevelopment of the tissues involved in this disorder. Due to abnormalities in the morphology of the skeleton and dentition it causes numerous functional problems (e.g. with breathing, sucking, swallowing, chewing, and speech) and promotes infections of the respiratory tract and middle ear [1]. Often the cleft is also the cause of varying degrees of self-esteem issues and social exclusion. The loss of anatomical continuity of the tissues due to cleft implies a disruption of the harmonious pre- and postnatal growth of all the anatomical structures that are interconnected and control further growth, resulting in deformities of the facial elements, jaws and nose.
The incidence of clefts varies. They are most common in Asians (Indians 3.6/1000, Japanese 2.1/1000, Chinese 1.7/1000) and are less common in African-Americans (0.3/1000). Among Caucasians, the average incidence is about 1/1000, with a fairly high incidence in Europe (Sweden 2/1000 and Denmark 1.9/1000) [2-4].
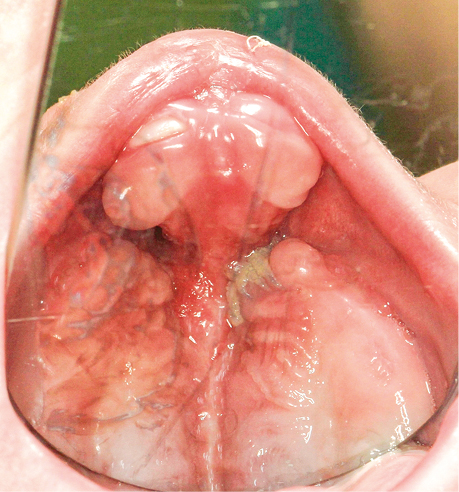
Cleft lip and palate causes numerous morphological abnormalities in the craniofacial region. Deformities observed in unilateral cleft lip and palate are a more or less pronounced cupid’s bow, a poorly marked or absent philtral ridge, shortening of the lip on the cleft side compared to its height on the unaffected side, an often-hypertrophied lip frenulum, the depth of the nasolabial fold usually only marked on the non-cleft side, a protrusion of the cutaneous part of the lip due to the retraction of the underlying muscles which have lost their grip. The nasal deformities associated with this cleft are flattening and widening of the nostril opening on the cleft side, tilt of the columella toward the affected side, upturned base of the nasal wing, deviation of the anterior nasal spike toward the normal side, and asymmetry of the nasal tip. In bilateral cleft lip and palate, the cupid’s bow is generally absent and the cutaneous portion of the lip is a convex lens-shaped surface. There is no visible philtral ridge and the prolabium is usually devoid of properly developed muscle fibres. Visible nasal deformities include a flattened and dilated nasal tip, shortened columella, and poorly developed septal nasal cartilage. The premaxilla is protruded, while the cleft jaw fragments collapse towards the midline [5] (Fig. 1).

Figure 1. Bilateral cleft palate in an infant
The treatment of cleft lip and palate in infants requires a multistage, multidisciplinary approach and cooperation between physicians of many specialties. Presurgical orthopaedic (PSO) treatment is one of the earliest stages of this treatment plan. Whereas presurgical orthodontic techniques are used to model the tissues of the jaw, alveolar process, and nose of an infant with unilateral or bilateral cleft lip and palate. According to many authors, infants who have a complete osseous cleft may benefit from PSO treatment applied prior to cleft lip and palate suturing procedures. The expected outcome of PSO treatment techniques is primarily an attempt to achieve better surgical outcomes by reducing the cleft gap and improving jaw growth, making the tissues of the lip and nasal region more flexible [6-7].
Other expected effects of PSO techniques mentioned in the literature are improvement of jaw growth, facilitation of intraoral feeding, improvement of speech function, and reduction of nasal deformity [6-7].
The literature suggests that the use of PSO by the orthodontist early in the child’s development, due to the high flexibility of the soft tissues, may offer the possibility of a better surgical treatment outcome. On the other hand, PSO techniques often raise several doubts and there is much discussion in the literature. The aim of this article was to review the literature about selected presurgical treatment techniques for cleft lip and palate in infants and to critically evaluate the their benefits, limitations and drawbacks.
Materials and methods
The literature from 1987-2021 was reviewed using the key words: presurgical treatment of cleft lip and palate in infants, presurgical orthopaedics in the treatment of cleft lip and palate in infants in the PubMed and Google Scholar databases and publications in the field of orthodontics and infant orthopaedics that were not available in the mentioned databases. Based on the analysis of 75 publications, 35 articles, and 2 textbooks related to the topic of the study were selected. Case reports and literature of Polish authors were included in the literature.
Results
PSO (Presurgical Orthopaedic) treatment is a clinical technique which has its beginning in the seventeenth century, when Hoffman used a headgear with straps which caused the retraction of the premaxilla and narrowing of the cleft fissure. Desault wanted to achieve the same effect with a similar technique in children with bilateral clefts. Later, Hullihen (1844) used adhesive tapes in the presurgical phase to help bring the cleft soft tissues together and Brophy (1927) used a silver wire passing through both cleft segments of the alveolar process, tightening the wire led to approximation of the segments [8]. A little later, McNeil (1950) used acrylic plates to form the cleft segments of the alveolar process [8-9]. Among the methods introduced for the presurgical treatment of clefts we should also mention the acrylic plates immobilised with pins aimed at simultaneous retraction of the premaxilla and expansion of the posterior cleft segments, used by Georgiade and Latham (1975) and the passive acrylic plates used by Hotz (1987). A method combining correction of cleft palate, alveolar process, lip, and nose was proposed in 1993 by B.H. Grayson and was based on the use of an acrylic plate fitted with a nasal stent and tapes [9-11]. Effective treatment of cleft lip and palate should lead primarily to restoration of the continuity of the alveolar ridge, normal oral function, development of the speech apparatus, and improvement of hearing and aesthetics. PSO techniques in their assumption aim to prepare the patient for surgical treatment. The authors of these publications suggest that combining PSO with surgery may contribute to favourable treatment outcomes, increasing the likelihood of improving the quality of life [7, 12].
The application of the chosen PSO therapy depends on the type of cleft and the preference of the treating physician. In the literature the most frequently mentioned PSO techniques are alveolar modelling with palatal plates, tape therapy, massage, and NAM [7].
Alveolar modelling with a palatal plate
Alveolar modelling with a palatal plate takes advantage of the increased formability of the maxillary segments in infants and the possibility of their repositioning. The aim of this treatment is to achieve an end-to-end alveolar position prior to surgical treatment. Active and passive, intraoral or extraoral appliances are used in the treatment. Active plates move the alveolar segments in a specific way with controlled forces, whereas passive appliances do not provide force but act as a support point for the forces generated during surgical suturing of the lip to contour and form the alveolar segments [13-14].
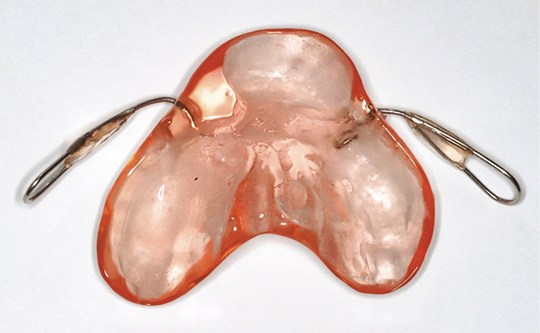
The plates used in PSO have two handles (wires) fused into the anterior part, lying on the cheeks. The plate located in the oral cavity covers the palate and alveolar ridge and covers the cleft fissure, separating the nasal and oral cavities (Fig. 2-3). In patients not treated with a plate, the tongue is located in the cleft fissure, impairs the growth of the jaw and reduces the size of the cleft fissure [15]. Depending on the type of cleft, the plate is relieved accordingly resulting in displacement of the cleft segments [16]. Numerous modifications of the palatal plate are described in the literature, e.g.: Perczyńska-Partyka (with a hole for a dummy), Burston (with a bite shaft), Perzynowa (with an orthodontic screw), Penkalowa (concerning bilateral clefts, with the use of an acrylic pad on the premaxilla) [16]. The following advantages of alveolar modelling with a palatal plate were reported in the literature:
- reduction of cleft fissure size due to growth of alveolar ridges and bones medially [7, 15],
- improved sucking and swallowing function and the possibility of replacing probe feeding in favour of breastfeeding [7, 16].
Whereas the following disadvantage of this technique was also noted: the headpiece or cloth straps (needed to keep the plate in the correct position) may cause discomfort for the patient [16].

Figure 2. Palate plate made of acrylic. View from the inside

Figure 3. Palate plate made of acrylic. Front view
Orthopaedic taping
Orthopaedic taping is commonly used in the presurgical management of cleft treatment. It can both complement another technique or be used as a separate therapeutic tool. External taping is used in conjunction with intraoral plates and is a source of external forces used in the process of alveolar ridge repositioning. The aim of orthopaedic taping is to approximate the soft tissues located in the immediate area of the cleft. The tapes mimic the flexibility and functionality of the muscles. In bilateral clefts, the tapes are placed on the patient’s cheeks and apply pressure on the protruding premaxilla to retract it. The forces acting on the cleft segments improve their position. In the case of unilateral clefts, lip protectors attached to the tape are used to facilitate the repositioning of the segments into the correct position. The desired effect of using this method is to change the shape of the lip edges and improve the muscular strength of this area [7, 17-18]. Among the advantages of orthopaedic taping technique is beneficial effect on muscle development, muscle mass gain and enhancement of the child’s facial expression [7, 18]. The following disadvantages of this technique are reported in the literature:
- frequent complications: skin irritations, ulcerations [8-9],
- difficulties in maintaining hygiene of the treated area [8, 19],
- mistakes in tape replication by the caregiver [19].
Massage
A PSO technique rarely described in the orthodontic and dental literature is cleft lip massage. The recommended PSO treatment for children with cleft is to massage both parts of the cleft lip. It is recommended that the massage be performed by the child’s caregiver several times a day. The massage should be performed in accordance with the recommendations of the orthodontist. Massages are intended to stretch and make soft tissues more flexible before surgery. Szeląg et al. describe the method of massage which depends on the type of cleft [16]. It is recommended to perform massages 3-5 times a day with 30 movements bringing the cleft lips together during one massage [16]. The main advantage of massage is increasing tissue elasticity and stretching, which facilitates surgical procedures (fusion of the cleft parts and formation of the lip) [15]. It should be noted that this is the least invasive of the techniques described [16].
Nasoalveolar Molding (NAM)
The NAM technique is a method particularly popular in the United States and is also used in many European and Asian countries. The aim of the technique is to reduce the oro-nasal deformity prior to primary surgery. The NAM technique uses a palatal plate and wire elements, as well as extraoral nasal stents, supported by surgical tapes. The elements used can lead to narrowing of the cleft fissure, formation of the nasal cartilage, the premaxilla, and the alveolar process. The desired outcome of treatment is to achieve the correct position of the replaced structures and a shape suitable for the neonatal-infant period [9]. According to the authors Grayson et al. [9] in infants with bilateral cleft lip and palate with alveolar involvement, the goals of presurgical NAM are non-surgical elongation of the columella, positioning of the premaxilla in the sagittal plane, and retraction of the premaxilla in a slow and gentle process to achieve continuity with the posterior segments of the alveolar cleft [9]. Additional objectives include reducing the width of the nasal tip, improving its projection, and reducing the width of the nasal wing base [9, 20].
The basis for the NAM concept was a study by Matuso et al. (1984), according to which hormones in infants (higher levels of oestrogen) have a significant effect on the ability to form cartilage tissue [8-10, 13]. The palatal plate is formed depending on the type of cleft, considering the areas of potential pressure and relief. Additionally, it is provided with a retention arm[s] usually ending in a retention button, which allows the attachment of flexible elements: orthodontic extractors, orthodontic elastics and surgical tapes stretched between the retention button and soft tissues of the cheeks. At a later stage of treatment (cleft fissure reduced to 5-6 mm), a stent is added to the plate, which should be beneficial in improving nasal symmetry and protrusion [8].
The NAM technique has many modifications regarding the construction of the palatal plate, the stent, and the treatment procedure. These include, for example, the PENAM technique described by Qi Wang et al. [21] using a nasal frame and stent, without the use of a palatal modelling plate, and the Figueroa NAM technique described by Y-F Chen and Y-F Liao [22] using a passive modelling plate [21-22].
Advantages of the NAM technique reported in the literature are:
- approximation of the cleft segments, alignment of the soft tissues, improved symmetry of the nasal cartilage which allows for better postoperative results with less risk of scarring [8-9, 23],
- a more favourable position of the alveolar process allows bone formation, which in the further development of the child gives a chance for teeth to erupt in the correct positions and the possibility of better alignment of the dentition and periodontal support [8, 24],
- the potential stimulation of immature nasal chondroblasts and their interstitial expansion, resulting in improved nasal morphology [8, 13].
Disadvantages of the technique reported in the literature:
- irritation and ulceration of the oral mucosa, gums, nose, and cheek skin, due to excessive pressure of the plate in the oral vestibular area and on the labial side of the premaxilla, Inflammation of the nasal tip area due to excessive force applied to the nasal stent and fungal infections resulting from poor tissue hygiene [8-9, 13, 25],
- he need for precise fabrication of the plate and its adjustment each time during the follow-up visit [8].
Discussion
A study on the effectiveness of the PSO techniques using a palatal plate was conducted by Mishima et al. [26]. The study involved 20 children (up to 18 months of age) with unilateral complete cleft lip and palate. Twelve children were treated with PSO using a palatal plate. The following parameters were assessed: degree of palatal dislocation, size of segment migration and shape of the alveolar process arch. Compared to the control group, an increase in the size of the palate with a decrease in the gap between the maxillary segments (sagittal axis), a reduction in the angle of the segments towards the nasal cavity and an increase in the migration of the smaller segment towards the larger segment were obtained. According to the authors Mishima et al. [26], the use of braces in PSO can stimulate segment growth and prevent the jaw arch from collapsing under the force of lip closure [26].
A study on the effectiveness of using PSO techniques with the NAM technique was described by Padovano et al. [27], who reviewed 12 studies on the long-term effects of using this technique in patients with unilateral cleft lip and palate. According to the analysis of the data, the use of the NAM technique was found to be beneficial in improving the aesthetic aspect compared to no presurgical treatment with braces [27]. According to Maull et al. [28], the NAM technique has a beneficial effect on nasal shape in patients with unilateral complete cleft. The use of this technique up to 4 months of age followed by primary surgery resulted in better nasal symmetry compared to the control group. The treatment effect persisted into early childhood [28]. Lee et al. [29] compared the results of patients with bilateral cleft treated with surgery with patients treated according to the NAM protocol. They found that non-surgical columella lengthening (NAM) followed by primary retrograde nasal reconstruction had a beneficial effect on columella length and significantly reduced the need for repeat nasal surgery [29].
Based on a long-term evaluation, Lee et al. [30] analysed the effects of alveolar modelling and gingivoperiosteoplasty (modified Millard type) on the growth of the midface in the prepubertal period. They found that presurgical nasoalveolar molding (NAM) and gingivoperiosteoplasty (Millard type) did not affect the growth of the midface in the sagittal or vertical planes (until the age of 9-13 years) [30]. Ringdahl [31], who compared the long-term effects of treatment using the NAM technique with patients in the control group, found no significant difference in midface growth [31].
It should be noted that in numerous articles the authors point out that the use of the NAM technique is associated with the risk of an abnormal process of movement of the larger segment without changing or with a weaker change in the position of the smaller segment, so that the smaller segment becomes blocked. Furthermore, excessive nostril dilatation, resulting from too early placement of the nasal stent, is noticeable [20, 29]. There are also opinions that, despite the beneficial effect on approximation of cleft maxillary segments in the NAM technique or other PSO methods, there are no clear long-term results indicating the benefits of the therapies [7].
Studies on the effectiveness of PSO techniques using kinesiotaping were described by Dajewee et al. [19]. The application of tapes transverse to the cleft fissure with their replacement every 1-3 days depending on the clinical condition of the patient (25% tape tension), applied until the child was 6 weeks old, led to a reduction in the cleft angle (on average from 57.53˚ to 31.3˚) and narrowing of its subnasal width (on average from 36.41 mm to 21.69 mm) as well as approximation of the tissues within the vermillion border (on average from 47.84 mm to 25.48) [19].
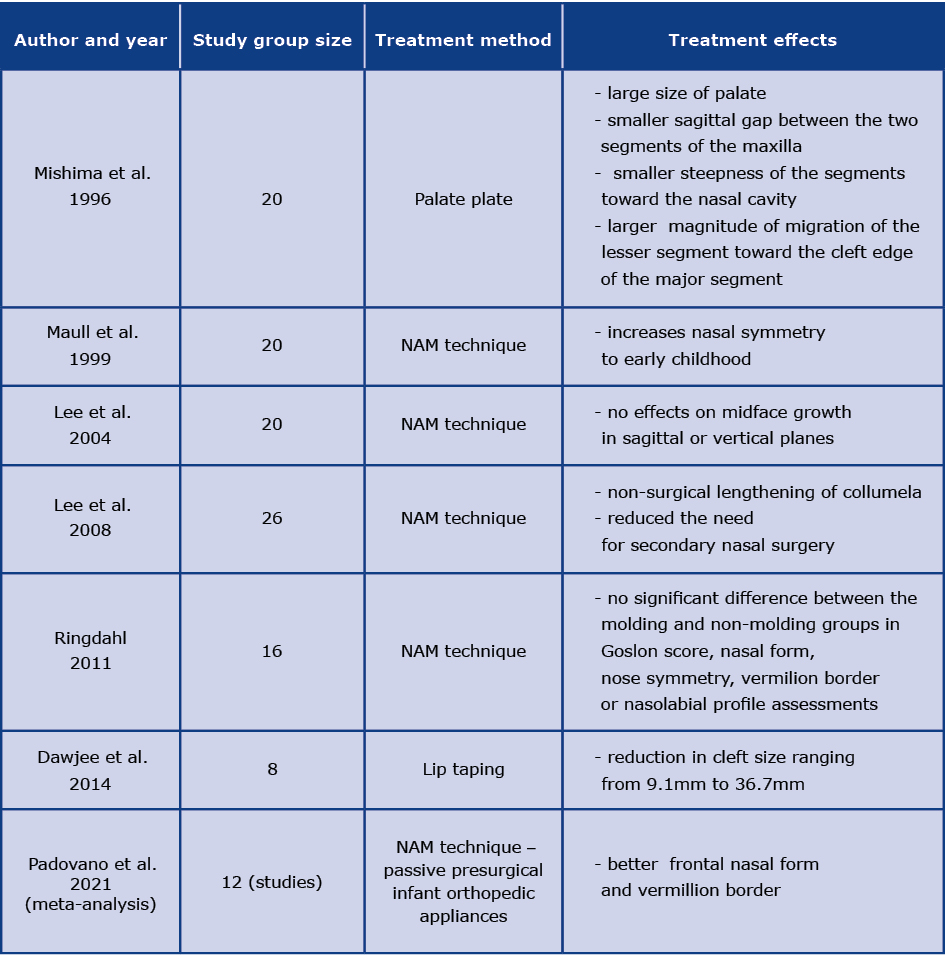
Table 1 summarizes the results of studies on the effect of presurgical therapy (see Table 1).
Table 1. Summary table of the described methods and effects of presurgical therapies

The effectiveness of using PSO techniques is controversial. The literature suggests that there is limited evidence on the long-term effects of the techniques discussed, which may be due to, for instance, the experience of the orthodontist [30]. Authors of publications also point out the need for detailed long-term studies on the efficacy of PSO, as they are mostly conducted with a small study group of a few to a dozen infants [26, 29-30, 32-33]. Certainly, treatment with PSO is a complex and costly therapy, with its effectiveness not unequivocally confirmed. There are few centres applying PSO, which often forces long travelling and generates high treatment costs [6]. According to Ross, a marked visual improvement in the faces of infants treated with PSO compared to those not treated becomes imperceptible over time [34]. Adali et al. found that the use of PSO techniques does not significantly affect the shape of the dental arch in the treatment of children with clefts [35]. Significant changes in its shape were only noticed after surgery [35]. Another argument against PSO is its negative impact on speech development due to delayed surgical closure of the hard palate [7, 36].
Presurgical techniques for the treatment of cleft lip and palate have been used for more than 60 years. The aim of PSO is to shape the segments of the cleft jaw and stimulate their growth and development. PSO is a preparation for further surgical treatment. Among the indications for PSO are anatomical abnormalities including cleft fissure size and various functional disorders [16]. It is important to note that the authors of the publications are divided and that there are different attitudes regarding the effectiveness of PSO. Published studies prove the effectiveness of PSO and the validity of the use of these techniques as well as those that undermine them.
Conclusion
Based on the analysis of the literature, we concluded that in favour of the use of PSO are multidisciplinary care of the child with a cleft and starting treatment from the first days of life, before surgery, its relatively low invasiveness, the possibility of performing it by the patient's caregivers (e.g., massages, kinesiotaping) and the reports on the potential effectiveness of PSO therapies. Whereas against the use of PSO techniques are contradictory reports of outcomes, lack of long-term evaluation of their effectiveness, limited availability and high cost of treatment.
Acknowledgements
All figures from Department of Orthodontics, University Dental Centre of the Medical University of Gdańsk.
Funding
None.
Conflicts of interests
None.
References
| 1. |
Ilczuk-Rypuła D, Pietraszewska D, Kempa M, Zalewska-Ziob M, Wiczkowski A. Methods of cleft lip and palate treatment over the centuries – a historical view. Ann Acad Medicae Silesiensis. 2017;(71):399–406.
|
| 2. |
Bellis TH, Wohlgemuth B. The Incidence of Cleft Lip and Palate Deformities in the South-east of Scotland (1971-1990). Br J Orthod [Internet]. 1999 Jun 16;26(2):121–5. Available from: http://www.tandfonline.com/doi/full/10.1093/ortho/26.2.121.
|
| 3. |
Vallino-Napoli LD, Riley MM, Halliday J. An Epidemiologic Study of Isolated Cleft Lip, Palate, or Both in Victoria, Australia from 1983 to 2000. Cleft Palate-Craniofacial J [Internet]. 2004 Mar 15;41(2):185–94. Available from: https://pubmed.ncbi.nlm.nih.gov/14989685/.
|
| 4. |
Kim S, Kim WJ, Oh C, Kim JC. Cleft lip and Palate Incidence Among the Live Births in the Republic of Korea. J Korean Med Sci [Internet]. 2002;17(1):49–52. Available from: https://jkms.org/DOIx.php?id=10.3346/jkms.2002.17.1.49.
|
| 5. |
Kummer A. Anatomy and Physiology of the orofacial structures and velopharyngeal valve in Cleft palate and craniofacial anomalies: Effects on Speech and Resonance. 2nd ed. New York: Thomas Delimar Learning; 2008. 2–35 p.
|
| 6. |
Prahl C, Kuijpers-Jagtman AM, Van ’T Hof MA, Prahl-Andersen B. A randomised prospective clinical trial into the effect of infant orthopaedics on maxillary arch dimensions in unilateral cleft lip and palate (Dutchcleft). Eur J Oral Sci [Internet]. 2001 Oct;109(5):297–305. Available from: http://doi.wiley.com/10.1034/j.1600-0722.2001.00056.x.
|
| 7. |
Alzain I, Batwa W, Cash A, Murshid ZA. Presurgical cleft lip and palate orthopedics: an overview. Clin Cosmet Investig Dent [Internet]. 2017 May;Volume 9:53–9. Available from: https://www.dovepress.com/presurgical-cleft-lip-and-palate-orthopedics-an-overview-peer-reviewed-article-CCIDE.
|
| 8. |
Retnakumari N, Divya S, Meenakumari S, Ajith PS. Nasoalveolar molding treatment in presurgical infant orthopedics in cleft lip and cleft palate patients. Arch Med Heal Sci [Internet]. 2014;2(1):36. Available from: http://www.amhsjournal.org/text.asp?2014/2/1/36/133804.
|
| 9. |
Grayson BH, Maull D. Nasoalveolar Molding for Infants Born with Clefts of the Lip, Alveolus, and Palate. Semin Plast Surg [Internet]. 2005;19(04):294–301. Available from: http://www.thieme-connect.de/DOI/DOI?10.1055/s-2005-925902.
|
| 10. |
Altug AT. Presurgical Nasoalveolar Molding of Bilateral Cleft Lip and Palate Infants: An Orthodontist’s Point of View. Turkish J Orthod [Internet]. 2017 Dec 22;30(4):118–25. Available from: https://turkjorthod.org/en/presurgical-nasoalveolar-molding-of-bilateral-cleft-lip-and-palate-infants-an-orthodontist-s-point-of-view-13911.
|
| 11. |
Mossey PA, Little J, Munger RG, Dixon MJ, Shaw WC. Cleft lip and palate. Lancet [Internet]. 2009 Nov;374(9703):1773–85. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0140673609606954.
|
| 12. |
Mosahebi A, Kangesu L. Cleft lip and palate. Surg [Internet]. 2006 Jan;24(1):33–7. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0263931906701740.
|
| 13. |
Murthy PS, Deshmukh S, Bhagyalakshmi A, Srilatha K. Pre surgical nasoalveolar molding: changing paradigms in early cleft lip and palate rehabilitation. J Int oral Heal JIOH [Internet]. 2013 Apr;5(2):70–80. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24155594.
|
| 14. |
Santiago PE, Schuster LA, Levy-Bercowski D. Management of the Alveolar Cleft. Clin Plast Surg [Internet]. 2014 Apr;41(2):219–32. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0094129814000029.
|
| 15. |
Piekarczyk B, Młynarska-Zduniak, E Winiarska-Majczyno M. Rozszczep wargi i podniebienia. Poradnik dla rodziców [in Polish]. Warszawa: Wydawnictwo Learskie PZWL; 2003. 25–29 p.
|
| 16. |
Szeląg J, Penkala J, Mikulewicz M, Antoszewska J. Leczenie ortodontyczne rozszczepów [in Polish]. In: Matthews-Brzozowska T, editor. Rozszczepy wargi i podniebienia. Wrocław: Uniwersytet Medyczny we Wrocławiu; 2007. p. 50–7.
|
| 17. |
Tollefson T, Gere R. Presurgical Cleft Lip Management: Nasal Alveolar Molding. Facial Plast Surg [Internet]. 2007 May;23(2):113–22. Available from: http://www.thieme-connect.de/DOI/DOI?10.1055/s-2007-979280.
|
| 18. |
Szarejko K, Kuć J, Aleksandrowicz K, Gołębiewska M. The essence of kinesiotaping in cranio-mandibular and cranio-facial area. Literature review. Part II. Prosthodontics [Internet]. 2016 Dec 21;66(6):437–44. Available from: https://doi.org/10.5604/.1226739.
|
| 19. |
Dawjee SM, Julyan JC, Krynauw JC. Lip tape therapy in patients with a cleft lip--a report on eight cases. SADJ [Internet]. 2014 Mar;69(2):62, 64–8, 70. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24974519.
|
| 20. |
Grayson BH, Shetye PR. Presurgical nasoalveolar moulding treatment in cleft lip and palate patients. Indian J Plast Surg [Internet]. 2009 Oct 15;42(S 01):S56–61. Available from: http://www.thieme-connect.de/DOI/DOI?10.1055/s-0039-1699377.
|
| 21. |
Wang Q, Zhou L, Zhao J-Z, Ko EW-C. An Extraoral Nasoalveolar Molding Technique in Complete Unilateral Cleft Lip and Palate. Plast Reconstr Surg Glob Open [Internet]. 2013 Jul;1(4):e26. Available from: http://journals.lww.com/01720096-201307000-00003.
|
| 22. |
Chen Y-F, Liao Y-F. A modified nasoalveolar molding technique for correction of unilateral cleft nose deformity. J Cranio-Maxillofacial Surg [Internet]. 2015 Dec;43(10):2100–5. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1010518215003340.
|
| 23. |
Grayson BH, Garfinkle JS. Early cleft management: The case for nasoalveolar molding. Am J Orthod Dentofac Orthop [Internet]. 2014 Feb;145(2):134–42. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0889540613009815.
|
| 24. |
Sharma MP, Sandhu BH, Kumar MA. Presurgical nasoalveolar molding in unilateral cleft lip and palate patient. Indian J Dent Adv [Internet]. 2012;4(4):1024–9. Available from: http://rep.nacd.in/ijda/pdf/4.4.1024.pdf.
|
| 25. |
Shetye PR, Grayson BH. NasoAlveolar molding treatment protocol in patients with cleft lip and palate. Semin Orthod [Internet]. 2017 Sep;23(3):261–7. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1073874617300233.
|
| 26. |
Mishima K, Sugahara T, Mori Y, Sakuda M. Three-Dimensional Comparison between the Palatal Forms in Infants with Complete Unilateral Cleft Lip, Alveolus, and Palate (UCLP) with and without Hotz’s Plate. Cleft Palate-Craniofacial J [Internet]. 1996 Jan 15;33(1):77–83. Available from: http://journals.sagepub.com/doi/10.1597/1545-1569_1996_033_0312_tdcbtp_2.3.co_2.
|
| 27. |
Padovano WM, Skolnick GB, Naidoo SD, Snyder-Warwick AK, Patel KB. Long-Term Effects of Nasoalveolar Molding in Patients With Unilateral Cleft Lip and Palate: A Systematic Review and Meta-Analysis. Cleft Palate-Craniofacial J [Internet]. 2021 Apr 22;59(4):462–74. Available from: https://doi.org/10.1177/10556656211009702.
|
| 28. |
Maull DJ, Grayson BH, Cutting CB, Brecht LL, Bookstein FL, Khorrambadi D, et al. Long-Term Effects of Nasoalveolar Molding on Three-Dimensional Nasal Shape in Unilateral Clefts. Cleft Palate-Craniofacial J [Internet]. 1999 Sep 15;36(5):391–7. Available from: http://journals.sagepub.com/doi/10.1597/1545-1569_1999_036_0391_lteonm_2.3.co_2.
|
| 29. |
Lee CTH, Garfinkle JS, Warren SM, Brecht LE, Cutting CB, Grayson BH. Nasoalveolar Molding Improves Appearance of Children with Bilateral Cleft Lip–Cleft Palate. Plast Reconstr Surg [Internet]. 2008 Oct;122(4):1131–7. Available from: https://journals.lww.com/plasreconsurg/Fulltext/2008/10000/Nasoalveolar_Molding_Improves_Appearance_of.18.aspx.
|
| 30. |
Lee CTH, Grayson BH, Cutting CB, Brecht LE, Lin WY. Prepubertal Midface Growth in Unilateral Cleft Lip and Palate following Alveolar Molding and Gingivoperiosteoplasty. Cleft Palate-Craniofacial J [Internet]. 2004 Jul 1;41(4):375–80. Available from: https://doi.org/10.1597/03-037.1.
|
| 31. |
Ringdahl L. The Long-term effect of nasoalveolar molding on midface Growth and nasolabial esthetics in complete unilateral cleft lip and palate patients [Internet]. Nova Southeastern University; 2011. Available from: https://www.proquest.com/openview/739693d20851f233f35a58b4c2b675f9/1?cbl=18750&pq-origsite=gscholar&parentSessionId=iaWMlERNQThZDCP%2BV2s%2BnNrmHCpMjFjWoUvdoEQRG8k%3D.
|
| 32. |
Ma L, Hou Y, Liu G, Zhang T. Effectiveness of presurgical orthodontics in cleft lip and palate patients with alveolar bone grafting: A systematic review. J Stomatol Oral Maxillofac Surg [Internet]. 2021;122(1):13–7. Available from: https://www.sciencedirect.com/science/article/pii/S2468785520301737.
|
| 33. |
Abbott MM, Meara JG. Nasoalveolar Molding in Cleft Care. Plast Reconstr Surg [Internet]. 2012 Sep;130(3):659–66. Available from: https://journals.lww.com/plasreconsurg/Fulltext/2012/09000/Nasoalveolar_Molding_in_Cleft_Care__Is_It.30.aspx.
|
| 34. |
Ross RB. Treatment variables affecting facial growth in complete unilateral cleft lip and palate. Cleft Palate J [Internet]. 1987 Jan;24(1):5–77. Available from: http://www.ncbi.nlm.nih.gov/pubmed/3542303.
|
| 35. |
Adali N, Mars M, Petrie A, Noar J, Sommerlad B. Presurgical orthopedics has no effect on archform in unilateral cleft lip and palate. Cleft Palate Craniofac J [Internet]. 2012 Jan;49(1):5–13. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21823827.
|
| 36. |
Konst EM, Weersink-Braks H, Rietveld T, Peters H. An intelligibility assessment of toddlers with cleft lip and palate who received and did not receive presurgical infant orthopedic treatment. J Commun Disord [Internet]. 2000;33(6):483–501. Available from: https://www.sciencedirect.com/science/article/pii/S0021992400000356.
|