-
- Academic Editor
-
-
-
†These authors contributed equally.
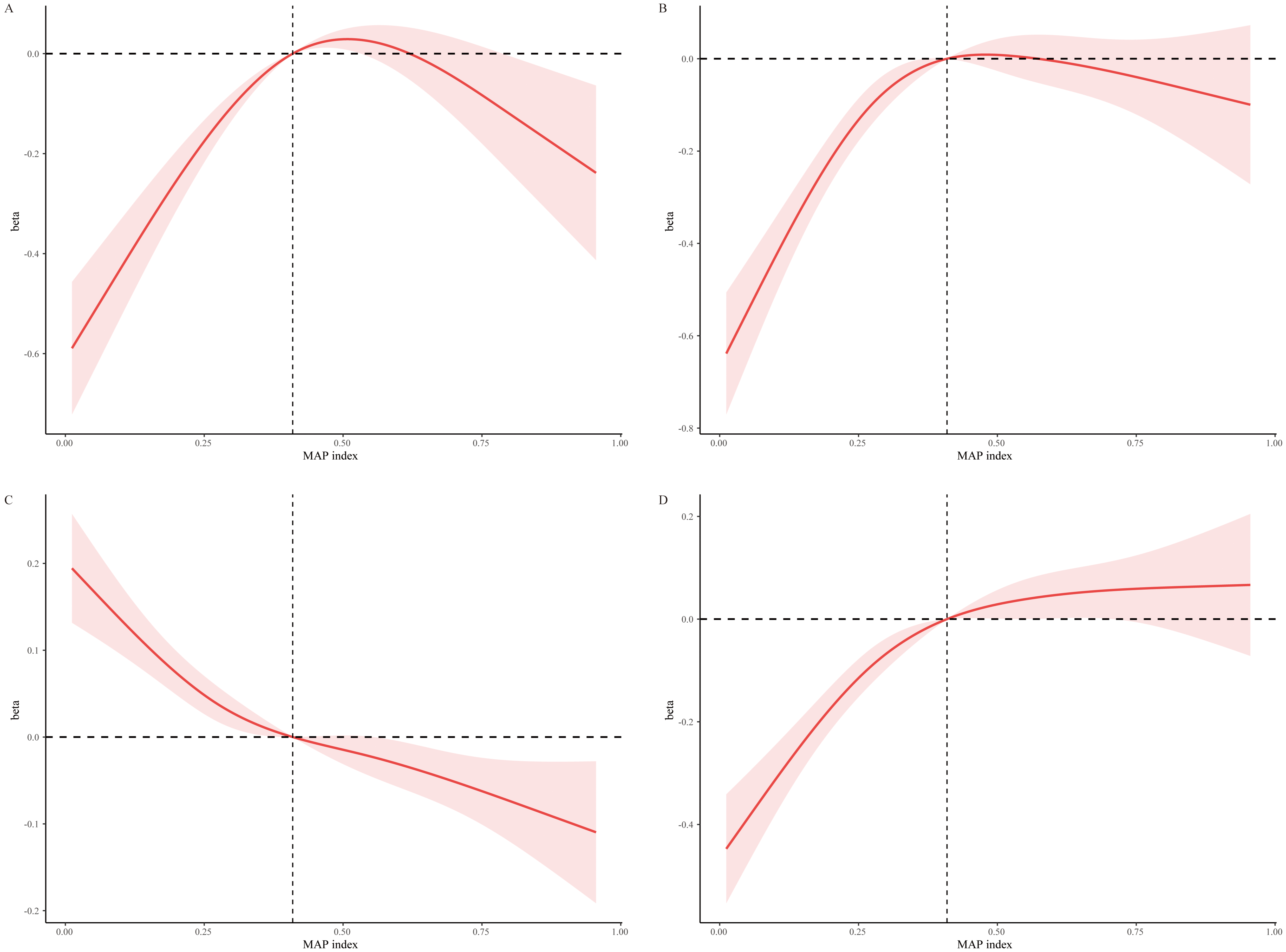
Background: The relationship between
the multivariable apnea prediction (MAP) index and lipid levels was examined
using a cross-sectional and retrospective study of National Health and Nutrition
Examination Surveys (2015–2018). A total of 3195 participants with MAP scores
were included in the analysis. Methods: The MAP index, an algorithm
leveraging sleep apnea symptom frequency, body mass index (BMI), age, and sex,
estimates the risk of obstructive sleep apnea (OSA). We investigated the
associations between the MAP index and lipid profiles—specifically,
high-density lipoprotein cholesterol (HDL-C), total cholesterol (TC), low-density
lipoprotein cholesterol (LDL-C), and triglycerides (TG) —using weighted linear
regression and restricted cubic splines (RCS) analysis. Additionally, mediation
analysis was conducted to explore the potential mediating role of physical
activity on the link between OSA risk, hyperlipidemia, and cardiovascular
mortality. Results: A non-linear relationship was observed between OSA
severity and lipid profiles, including elevated levels of TC, increased LDL-C,
higher TG, and decreased HDL-C (All p for non-linearity