More Information
Submitted: October 02, 2022 | Approved: October 13, 2022 | Published: October 14, 2022
How to cite this article: Jiménez RM, Rius MG. State of the science in diabetic foot: subjective screening vs. objective diabetic neuropathy examination in primary care. J Neurosci Neurol Disord. 2022; 6: 049-051.
DOI: 10.29328/journal.jnnd.1001069
Copyright License: © 2022 Jiménez RM, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Diabetic foot; Neuropathy; Primary care
State of the science in diabetic foot: subjective screening vs. objective diabetic neuropathy examination in primary care
Rafael Medrano Jiménez1* and Mª del Mar Gili Rius2
and Mª del Mar Gili Rius2
1Podiatrist in Private Practice, Joaquin Ruyra 8-10 Badalona cp. 08918, Barcelona, Spain
2Catalan Institute of Health ICS, La Sagrera Primary Care Center, C/ de Garcilaso, 1, cp.08027, Barcelona, Spain
*Address for Correspondence: Rafael Medrano Jiménez, Podiatrist in Private Practice, Joaquin Ruyra 8-10 Badalona CP. 08918, Barcelona, Spain, Email: medrano.vascular@gmail.com
Among the conditioning factors of Diabetic Foot (DF), neuropathy is considered the main factor, arteriopathy the aggravating factor, and foot deformities the triggering factor. The preventive interventions for DF and its complications are distributed by levels of care. At the higher level, hospital care focuses on reducing DF amputations. At the lower level, Primary Care (PC) and Podiatry, focused on preventing DF. PC is considered the ideal place to identify the conditioning factors of DF. In this area, prevention follows the recommendations of the International Working Group on Diabetic Foot (IWGDF) by screening neuropathy focused on the sensitive or insensitive foot. The American Diabetes Association (ADA) a recommends person-centered assessment of neuropathy by clinical examination of symptoms and signs testing sensory, motor, and autonomic neuropathy. This controversy lead us to investigate which methodology (screening or clinical examination) could be more accurate in identifying the conditioning factors of DF in a group of people recruited in the TERMOPIEDI study. Neuropathy was assessed following the definition of diabetic neuropathy, the Young MJ diagnostic criteria, and the Toronto Council diagnostic category. These results allowed us to know the applicability of this procedure in PC within nursing competencies, detecting a greater number of patients with neuropathy compared to the screening method. People with neuropathy presented higher plantar temperature, concluding that neuropathy interferes with foot thermoregulation.
In relation to foot problems in people with Diabetes Mellitus (DM), there are two well-differentiated clinical situations. On one hand, Diabetic Foot (DF) when an ulcer is present ly defined as “Total destruction of the layers of skin located between the malleoli and toes”. On the other hand, Foot at risk or patient at risk (RP), when in the absence of an active ulcer there is a probability of ulceration secondary to peripheral neuropathy, structural deformities of the foot or arterial disease, coexisting DM [1-3].
The DF continues to be an important health problem, limiting the quality of life of these people and generating a high social and health cost whose mortality can reach 55% 5 years after major amputation. Although a reduction in major amputations has been observed in recent years, there is still a trend of increased reulcerations and minor amputations [4-7].
The complex pathophysiology of DF is multifactorial, making it difficult to approach this health problem. Therefore, epidemiological studies are heterogeneous with great variability of results depending on the geographical area, population , and scope of the study [8]. All of these, the multidisciplinary approach to DF at the hospital level, the advances in the local treatment of DF, and the new technologies open a hopeful path to the prevention of DF and its complications [7,9,10].
However, the prevention of DF has not followed the same evolution in the field of Primary Care (PC).
Currently, the American Diabetes Association (ADA) and the International Diabetic Foot Work Group (IWGDF) emphasize prevention as the only way to reduce the incidence of DF and its complications, distributing preventive interventions by care levels. At the higher level, specialized care is located in the hospital environment, whose main objective is to reduce amputations due to FD. At the lower level, Primary Care (PC) and Podiatric care focus on identifying RP and controlling foot disorders, respectively. PC is considered the ideal setting in which to identify RP among the population treated for DM and to establish selective interventions for multidisciplinary prevention of DF [1-3].
This responsibility can lead to a controversy between the recommendations of the main groups of experts. The IWGDF recommends screening for RP focused on the sensitive or insensitive foot through two subjective sensory tests (Pressure and Vibration) considering neuropathy as absent or severe, the ADA recommends the identification of person-centered neuropathy through physical examination including symptoms and objective signs of neuropathy related to fine and thick fiber innervation [1,2,11].
The IWGDF screening model is a powerful predictor of DF. However, it may be insufficient for the diagnostic categorization of diabetic neuropathy, which could mean an underestimation of this complication in PC. Considering that a person with neuropathy presents a n RP due to neuropathy and, in the case of DF, a neuropathic ulcer, the ADA recommendations allow us to know the pathophysiological characteristics of this complication and its clinical manifestations codified in the International Classification of Diseases (ICD) related to DM [1,2,11-13].
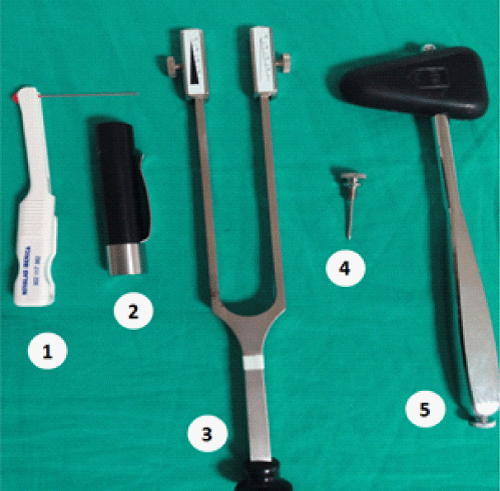
It is known that diabetic neuropathy reduces or cancels the patient’s ability to respond to small injuries to the feet that can lead to ulceration and subsequent complications [12,14,15 ]. Evaluation of sensory peripheral neuropathy is based on the physiological responses of sensory neuronal receptors in the dermis that can be stimulated, through direct contact with the foot, by selective manual instruments Figure 1.
Figure 1: Instrumented Peripheral Neuropathy Evaluation. Note: Use of applied instruments: Selective.
1: Semens Westein 5.07 monofilament (pressor sensitivity). 2: Thermal discriminator (cold, less cold) (Thermal sensitivity).
3: Rydel Scheifer ruled tuning fork (Vibratory sensitivity). 4: Blunt tip needle (Painful sensitivity). 5: Reflex hammer (Achilles, patellar reflexes).
Stimulation Neuronal fine fiber receptors respond to thermal stimuli through the terminal bulbs of Krause (cold) and corpuscles of Rufini (heat). The sensitivity Pain, recognized by stimulation of free nerve fibers, to this day it is not been tested in PC. Large fiber neuronal receptors sense vibratory stimulation via Meisner’s corpuscles and pressor stimulation is detected via Pacini and corpuscles (2.12). In relation to symptomatology, the symptoms expressed as “Pain, Burning or Cramps” are related to alterations of the sensitive peripheral nerves of fine fiber, and those expressed as “numbing or tingling”, to thick fiber [2,12,15-19].
Based on this knowledge and the importance of early identification of RP in PC [1-3], we carried out the TERMOPIEDI study [17,18] oriented to Knowing the plantar temperature variations associated with the conditioning factors of the DF. Neuropathy was assessed following the definition of diabetic neuropathy [1,2] the Young MJ assessment model [15] and the Toronto Council diagnostic category [16]. The joint score of the scales of signs of disability (Neuropathy Disability Score) NDS and scale of symptomatic reduced NSS (Neuropathy Symptoms Score) [15], allowed us to apply for the maximum diagnostic category of neuropathy that can be assumed in CP as “Probability” [16].
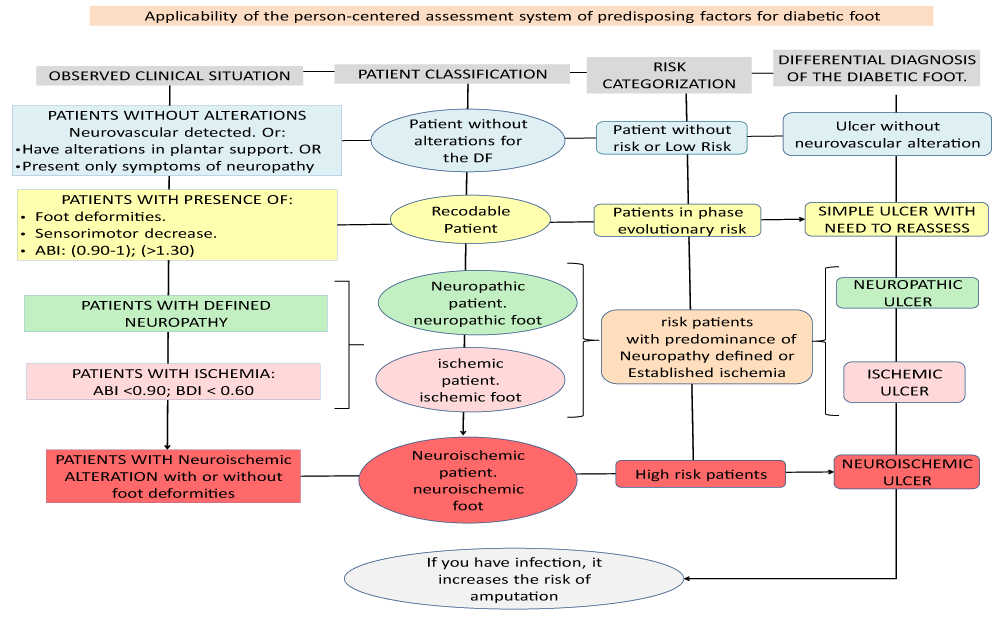
The NDS scale is made up of two domains (sensory and motor). The sensory items assess thermal, pain (fine fiber) vibration (thick fiber) sensitivities. The motor item is sensed through the Achilles reflex. As a novelty in the TERMOPIEDI study [17,18], pressor sensitivity (thick fiber) was incorporated into the NDS scale reinforcing the sensitive domain and following the recommendations of both groups of experts to identify RP in PC. This procedure makes it possible to assess symptoms and signs of sensory neuropathy in relation to the type of nerve fiber involved, demonstrating that the quantitative neuropathy scoring system is a better predictor of DF than the separate screening method [19]. In addition, the NDS scale discriminates between the right and left foot which allows knowing the sensory evolution over time and establishing a differential diagnosis between other types of non-diabetic neuropathy. The joint score of the NDS and NSS scales identifies different clinical manifestations of DM neuropathy, improving the categorization of risk and the etiological diagnosis of DF as shown in Figure 2.
Figure 2: Algorithm of the clinical situations detected with the neurovascular assessment model of the TERMOPIEDI study. Note: Own elaboration. The neurovascular assessment model of the TERMOPIEDI study would allow an early diagnosis of the etiology of Diabetic Foot.
The TERMOPIEDI [17,18], study, presented an objective evaluation model of conditioning factors for DF applicable in PC and manageable by Nursing. People with detected neuropathy presented a higher plantar temperature than people without this complication, associating neuropathy as a conditioning factor of foot thermoregulation. The TERMOPIEDI conclusions showed that the objective evaluation of RP detected neuropathy much better than the screening method.
- Schaper NC, van Netten JJ, Apelqvist J, Sicco A. Bus, Robert J. Hinchliffe, Benjamin A. Lipsky on behalf of the International Working Group on the Diabetic Foot (IWGDF)IWGDF Practical guidelines on the prevention and management of diabetic foot disease. Part of the 2019 IWGDF Guidelines on the Prevention and Management of Diabetic Foot Disease.
- American Diabetes Association. 11. Microvascular Complications and Foot Care: Standards of Medical Care in Diabetes-2020. Diabetes Care. 2020 Jan;43(Suppl 1):S135-S151. doi: 10.2337/dc20-S011. PMID: 31862754.
- Reig-Viader R, Espallargues M. Review and proposal of the diabetic foot care model in Catalonia. Barcelona: Health Quality and Evaluation Agency of Catalonia. Department of Health. Government of Catalonia; 2019.
- Khunkaew S, Fernandez R, Sim J. Health-related quality of life among adults living with diabetic foot ulcers: a meta-analysis. Qual Life Res. 2019 Jun;28(6):1413-1427. doi: 10.1007/s11136-018-2082-2. Epub 2018 Dec 18. PMID: 30565072.
- Rubio JA, Jiménez S, Álvarez J. Clinical characteristics and mortality of patients cared for in a Multidisciplinary Diabetic Foot Unit. Endocrinology, Diabetes and Nutrition. 2017; 64(5): 241-249. doi: 10.1016 / j.endinu.2017.02.012
- Jiménez S, Rubio JA, Álvarez J, Lázaro-Martínez JL. An Analysis of reulcerations in a multidisciplinary unit of diabetic foot after the implementation of an integrated foot care program. Endocrinolog, Diabet and Nutrition. 2018; doi: 10.1016/ j.endinu.2018.03.012
- Jiménez S, Rubio JA, Álvarez J, Ruiz Grande F. Trend in the incidence of lower limb amputations after the implementation of a Multidisciplinary Diabetic Foot Unit. Endocrinology, Diabetes and Nutrition. 2017; 64(4): 188–197.
- Zhang P, Lu J, Jing Y, Tang S, Zhu D, Bi Y. Global epidemiology of diabetic foot ulceration: a systematic review and meta-analysis †. Ann Med. 2017 Mar;49(2):106-116. doi: 10.1080/07853890.2016.1231932. Epub 2016 Nov 3. PMID: 27585063.
- Tardáguila-García A, García-Morales E, García-Alamino JM, Álvaro-Afonso FJ, Molines-Barroso RJ, Lázaro-Martínez JL. Metalloproteinases in chronic and acute wounds: A systematic review and meta-analysis. Wound Repair Regen. 2019 Jul;27(4):415-420. doi: 10.1111/wrr.12717. Epub 2019 Mar 27. PMID: 30873727.
- Shu X, Shu S, Tang S, Yang L, Liu D, Li K, Dong Z, Ma Z, Zhu Z, Din J. Efficiency of stem cell based therapy in the treatment of diabetic foot ulcer: a meta-analysis. Endocr J. 2018 Apr 26;65(4):403-413. doi: 10.1507/endocrj.EJ17-0424. Epub 2018 Jan 22. PMID: 29353870.
- Alonso Fernández M, Mediavilla Bravo JJ, López Simarro F, Comas Samper JM, Carramiñana Barrera F, Mancera Romero J. Assessment of diabetic foot screening in Primary Care. Endocrinol. Nutr. 2014;61(6):311-317.
- Dyck PJ, Herrmann DN, Staff NP, Dyck PJ. Assessing decreased sensation and increased sensory phenomena in diabetic polyneuropathies. Diabetes. 2013 Nov;62(11):3677-86. doi: 10.2337/db13-0352. PMID: 24158999; PMCID: PMC3806590.
- International Classification of Diseases 10th Revision, Clinical Modification. 4th Spanish edition Ministry of Health. https://eciemaps.mscbs.gob.es/ecieMaps/browser/index_10_mc.html
- Crawford F, Nicolson DJ, Amanna AE, Martin A, Gupta S, Leese GP, Heggie R, Chappell FM, McIntosh HH. Preventing foot ulceration in diabetes: systematic review and meta-analyses of RCT data. Diabetologia. 2020 Jan;63(1):49-64. doi: 10.1007/s00125-019-05020-7. Epub 2019 Nov 27. PMID: 31773194; PMCID: PMC6890632.
- Young MJ, Boulton AJ, MacLeod AF, Williams DR, Sonksen PH. A multicentre study of the prevalence of diabetic peripheral neuropathy in the United Kingdom hospital clinic population. Diabetologia. 1993 Feb;36(2):150-4. doi: 10.1007/BF00400697. PMID: 8458529.
- Tesfaye S, Boulton AJ, Dyck PJ, Freeman R, Horowitz M, Kempler P, Lauria G, Malik RA, Spallone V, Vinik A, Bernardi L, Valensi P; Toronto Diabetic Neuropathy Expert Group. Diabetic neuropathies: update on definitions, diagnostic criteria, estimation of severity, and treatments. Diabetes Care. 2010 Oct;33(10):2285-93. doi: 10.2337/dc10-1303. Erratum in: Diabetes Care. 2010 Dec;33(12):2725. PMID: 20876709; PMCID: PMC2945176.
- Medrano Jiménez R, Gili Rius MM, García Castillo O, Ruiz Messeguer M, Medrano Baeza B, Anglà Vendrell M. Plantar thermometry and diabetic foot risk in primary care. Results of the thermopiedi study. Butlletí.
- Medrano Jiménez R, Gili Riu MM, Herrera Diaz MA. Identify the risk foot in patients with diabetes. A space for improvement in primary care, Family Medicine. Semergen. 2022. https://doi.org/10.1016/j.semerg.2022.01.007
- Abbott CA, Carrington AL, Ashe H, Bath S, Every LC, Griffiths J, Hann AW, Hussein A. North-West Diabetes Foot Care Study representation. The North-West Diabetes Foot Care Study: incidence of, and risk factors for, new diabetic foot ulceration in a community-based patient cohort. Diabet Med. 2002 May;19(5):377-384.