Learning clinical reasoning skills during the transition from a medical graduate to a junior doctor
Submitted: 1 May 2023
Accepted: 21 December 2023
Published online: 2 April, TAPS 2024, 9(2), 5-17
https://doi.org/10.29060/TAPS.2024-9-2/OA3053
WCD Karunaratne1, Madawa Chandratilake2, Kosala Marambe3
1Centre for Medical Education, School of Medicine, University of Dundee, United Kingdom; 2Department of Medical Education, Faculty of Medicine, University of Kelaniya, Sri Lanka; 3Department of Medical Education, University of Peradeniya, Sri Lanka
Abstract
Introduction: The literature confirms the challenges of learning clinical reasoning experienced by junior doctors during their transition into the workplace. This study was conducted to explore junior doctors’ experiences of clinical reasoning development and recognise the necessary adjustments required to improve the development of clinical reasoning skills.
Methods: A hermeneutic phenomenological study was conducted using multiple methods of data collection, including semi-structured and narrative interviews (n=18) and post-consultation discussions (n=48). All interviews and post-consultation discussions were analysed to generate themes and identify patterns and associations to explain the dataset.
Results: During the transition, junior doctors’ approach to clinical reasoning changed from a ‘disease-oriented’ to a ‘practice-oriented’ approach, giving rise to the ‘Practice-oriented clinical skills development framework’ helpful in developing clinical reasoning skills. The freedom to reason within a supportive work environment, the trainees’ emotional commitment to patient care, and their early integration into the healthcare team were identified as particularly supportive. The service-oriented nature of the internship, the interrupted supervisory relationships, and early exposure to acute care settings posed challenges for learning clinical reasoning. These findings highlighted the clinical teachers’ role, possible teaching strategies, and the specific changes required at the system level to develop clinical reasoning skills among junior doctors.
Conclusion: The ‘Practice-oriented clinical skills development framework’ is a valuable reference point for clinical teachers to facilitate the development of clinical reasoning skills among junior doctors. In addition, this research has provided insights into the responsibilities of clinical teachers, teaching strategies, and the system-related changes that may be necessary to facilitate this process.
Keywords: Clinical Reasoning, Medical Decision Making, Medical Graduates, Junior Doctor Transition, Hermeneutic Phenomenology, Qualitative Research
Practice Highlights
- A safe environment and early healthcare team integration facilitate learning clinical reasoning.
- Adopting a comprehensive approach to reasoning can overcome specialty-specific reasoning challenges.
- Trainees’ emotional commitment toward patients could help them learn clinical reasoning skills.
- Interrupted supervisory relationships and early acute care exposure can hamper learning reasoning.
- Ensuring junior doctor training is both service and learning oriented is of paramount importance.
I. INTRODUCTION
Clinical reasoning is composed of cognitive processes, metacognitive processors, and behaviour during the application of critical thinking to a clinical situation and is heavily influenced by numerous contextual factors related to the doctor, patient, and the clinical environment (Durning et al., 2011; Durning et al., 2013; Norman, 2005).
The clinical reasoning of learners evolves along the continuum of medical education with unique challenges associated with major transition phases, the progression from non-clinical to clinical stage, medical graduate to junior doctor, and specialist trainee to medical specialist (Teunissen & Westerman, 2011). Notably, the medical graduate to junior doctor transition presents more pronounced difficulties (Brennan et al., 2010), primarily due to changing roles and responsibilities towards patient care, limited experience in navigating clinical uncertainties, and the need to work within multi-professional teams with limited support. Consequently, these factors have contributed to a steep learning curve for developing clinical reasoning skills (Brennan et al., 2010; Lempp et al., 2005; Prince et al., 2004; Tallentire et al., 2017). The challenges in developing reasoning skills are associated with the reduced applicability of undergraduate training in clinical practice (Cave et al., 2009; Monrouxe et al., 2017), coordinating and organising clinical and administrative responsibilities (Cameron et al., 2014; Teunissen & Westerman, 2011), and dealing with diverse contextual factors in practice. These factors encompass navigating hierarchical relationships and meeting the expectations of seniors, difficulties in recognising disease severity, uncertainty regarding their role, and tension in interpersonal relationships with team members (Cameron et al., 2014; Tallentire et al., 2011, 2017). When these challenges are not resolved, they could boil down to deficits in clinical reasoning and diagnostic error leading to adverse patient outcomes (Graber et al., 2005; Huckman & Barro, 2005; Jen et al., 2009).
The challenging nature of the junior doctor transition is shared across many similar contexts globally (Prince et al., 2000; Teunissen & Westerman, 2011) calling for a coherent approach to facilitate learning clinical reasoning. Concerns around clinical reasoning deficits of doctors continue to soar even today in resourceful developed countries (Health Services Safety Investigation Body, 2022; Huckman & Barro, 2005; Jen et al., 2009), emphasising the need for faculty to take decisive actions to resolve it! Unless for the limited research on clinical reasoning outside the western region (Lee et al., 2021), the situation could have been the same elsewhere.
There is ample evidence of numerous factors that may improve the development of clinical reasoning skills. Accordingly, work experience (Ericsson, 2004; Norman, 2005; Norman et al., 2007), a strong foundation on basic biomedical concepts (Woods, 2007), reflective practice (Mamede et al., 2008, 2012), feedback (Hattie & Timperley, 2007), learning from others during practice, and conducive organisational context for learning (Goldacre et al., 2003; Hattie & Timperley, 2007; Lempp et al., 2005) are found to be central in learning clinical reasoning. This evidence, however, is not specific to junior doctors. The learning needs of junior doctors in transition may vary from other trainee doctors and other health professions staff. Therefore, it has become critical that the clinical reasoning experiences, challenges, and practices of junior doctors as a vulnerable group of trainees are understood well to be able to better support their development of clinical reasoning.
When exploring this period of transition, the five-stage model of adult skill acquisition from novice to expert (Dreyfus, 2004), can help understand how junior doctors progress in relation to these stages. The situated learning theory (S. J. Durning & Artino, 2011; Lave, 1991) can provide the basis for understanding the social nature of learning clinical reasoning. The influence of contextual factors on mediating internal motivation for learning clinical reasoning can be understood through the self-determination theory (Ryan & Deci, 2000; Taylor & Hamdy, 2013). Therefore, to gain a better understanding of the transition experiences from medical graduates to junior doctors, a longitudinal study was designed using the above theoretical models as the conceptual framework to explore the following research questions:
(1) How do junior doctors evaluate their learning experiences of clinical reasoning development?
(2) What adjustments in the application of different educational means into the learning environment are necessary to improve the development of clinical reasoning skills?
II. METHODS
A. Methodology
The methodological approach of hermeneutic phenomenology (Crotty, 1998; Laverty, 2003) was employed in this study (Kafle, 2011; Laverty, 2003). Such an approach to clinical reasoning was adopted by other researchers exploring clinical reasoning (Ajjawi & Higgs, 2007; Langridge et al., 2015; Robertson, 2012).
B. Study Setting
The study was conducted at the North Colombo Teaching Hospital, Ragama, Sri Lanka with ethical clearance (P/11/01/16) from the Faculty of Medicine, University of Kelaniya.
In Sri Lanka, medical undergraduate training is a five-year programme with two pre-clinical and three clinical years. After graduation, medical graduates follow a 12-month internship where they work under a consultant for six months each in any of the two main clinical specialities, namely, Medicine, Surgery, Paediatrics, and Gynaecology & Obstetrics before obtaining full registration as a medical doctor.
C. Study Design and Sampling
The study participants were junior doctors during the 12 months of internship following graduation. Maximum variation sampling (Cohen et al., 2017), which enabled purposefully selecting the widest range of variation on dimensions of interest relevant to learning and practicing clinical reasoning was employed. The concept of ‘information power’ which sought not theoretical saturation but sufficient information to address the research questions informed the sample size (Malterud et al., 2016; Varpio et al., 2017). Hence, junior doctors working in the four main clinical specialties, in both university clinical wards staffed by university clinical academics and other clinical wards composed of medical consultants under the Ministry of Health and according to gender were enrolled in the study following informed consent.
Accordingly, eighteen junior doctors (n=18, males=8, females=10) from the four main clinical specialities (Medicine-4, Surgery-5, Paediatrics-4, Obstetrics and Gynaecology-5) were enrolled in the first stage of the study. The second stage of the study imposed heavy demands on the study participants because it involved recording multiple doctor-patient encounters and subsequent discussions based on stimulated recall. Therefore, out of the initially recruited participants, only the well-articulated consenting participants (n=8), who could proficiently express their thoughts and reasoning to obtain a good insight into the nature of practicing clinical reasoning were enrolled in this stage.
D. Data Collection
The data collection proceeded in two stages.
During the first stage, a combination of individual semi-structured interviews with narrative interviews were conducted. Semi-structured interviews allowed probing where necessary (Cohen et al., 2017), while the narratives allowed participants to tell their stories of clinical reasoning (Muylaert et al., 2014). Each lasted for 45-50 minutes.
The second stage included audio-recording the patient consultations of the selected participants on predefined dates during the first and second six months of their internship. The consultations were replayed, and post-consultation discussions were conducted soon afterward by employing a stimulated recall method, to account for a total of 48 post-consultation discussions. As clinical reasoning is a concept revealed only in action (Charlin et al., 2000), employing such an approach was considered essential during this study.
E. Data Analysis
All interviews and discussions were transcribed verbatim. The data analysis followed phenomenological and hermeneutic strategies, which required a thorough description of lived experiences (Ajjawi & Higgs, 2007) and employing a hermeneutic circle for data interpretation by moving back and forth between the parts and the whole of the experience to reach a deeper understanding of the experience (Laverty, 2003).
Thematic data analysis (Braun & Clarke, 2012) was conducted to generate themes explaining the data set as a whole.
The principal researcher developed two thematic frameworks for the two stages of the study. The two supervisors of the project re-coded selected transcripts from each stage. These independently derived frameworks were discussed, themes refined, and new themes identified until an agreement was reached. The finalised thematic framework was employed to code all the transcripts using the Atlas.ti qualitative data analysis tool.
III. RESULTS
A total of 18 individual interviews and 48 post-consultation discussions were analysed giving rise to seven themes. During analysis, it was noted that the factors that inform the development of clinical reasoning could be condensed together as a model. This is presented later in the text.
Each theme is elaborated below with quotations. When more than one quotation is required to describe a theme, these are presented within a table. Additional supportive quotations are openly available in Figshare at https://doi.org/10.6084/m9.figshare.23536548.v2 (Karunaratne et al., 2023).
A. A Safe and Supportive Working Environment Empowers Junior Doctors to Develop Clinical Reasoning Skills
It was the collective view that a ‘safe’ work environment is characterised by easy access to more experienced doctors, and the presence of a safety net of seniors who review junior doctors’ work and understand their reasoning challenges. It provided junior doctors the opportunity and freedom to practice clinical reasoning independently, learn from errors, and arrive at their own reasoning decisions.
Such a conducive work environment also provided them with opportunities to emulate seniors and receive real-time feedback while actively participating in authentic tasks and applying knowledge and skills acquired during their undergraduate training.
“I’m working in a unit where each admission is clerked by the registrar. So, in that case, we are always in feedback…What I usually do is sometimes I clerk the patients first, and after that, I compare it with the registrar’s clerking. So, in that case, we can easily adapt their clerking.”
(MP3, Medicine, Male, Phase-1)
B. Learning to Reason with Clinical Problems is Situated and Facilitated by Work Experience
Work experience provided the opportunity to learn from repeated exposure to clinical presentations and their variations, learn from seniors, and lapses of reasoning. However, work experience alone is not solely sufficient, and it is the collective influence of many other factors that help learn clinical reasoning. These factors are captured by the model developed from this study.
With work experience, junior doctors’ approach to reasoning changed from a ‘disease-oriented approach’ developed through undergraduate education to a ‘practice-oriented approach’. In the practice-oriented approach, junior doctors actively analyse clinical problems instead of matching them with memorised configurations of disease presentations.
They also developed ‘instincts’ for swift decision-making, sharpened through experience in recognising contextual factors in patient presentations. This was especially valuable for identifying acute cases requiring urgent care. In addition, they recognised the impact of the previous disease burden in formulating differential diagnoses, leading to a broader approach in their clinical reasoning.
Table 1 illustrates participant quotations that shed light on the role of work experience in learning clinical reasoning skills.
|
“…This approach in the ward is always problem-based. We’re dealing with problems. We try to solve the problems. That approach as a student was trying to fit the history into one of the long cases we have studied…Now we are not worried about that broad category. We will instead deal with the different problems that they have.” (MP2, Medicine, Male, Phase-1) |
|
“I think it’s just being with the patients. You realise that … it’s not just what’s written in the book…I mean now, if you’re just walking past a patient, you realise that this patient is not well. Whereas initially, you would have to go through the ward round and… go through the records, and then only you’ll see it. I don’t know how you get that but…” (MP2, Medicine, Male, Phase-1) |
|
“…Once a child with hypovolemic shock came to the ward. I was in the ward alone. I was very afraid at that time as I was in my first week of internship. So, nothing was on my mind, and I called my senior and he asked me to give (fluid) boluses until he came…. (There was another emergency at the same time). An Angioedema child came to the ward. I thought of (laughing)… running away from the ward. Because it was the initial period, it was very difficult, and our clinical knowledge was also poor. But now, we can manage any emergencies until the senior comes.” (PP, Paediatrics, Female, Phase-1) |
|
(When enquired on the reasons for commencing consultations with comorbidities?) “… Even the presenting complaint may be related to past medical conditions as well…and even this patient has diabetes… so, they can present in various ways… As an intern, I developed that. As an undergraduate, we are asking for name, age, where are you from, and then go on to take the history first…” (MP4, Medicine, Female, Phase-2) |
Table 1. Quotes illuminating that learning clinical reasoning is situated and facilitated by work experience
C. Internal Motivation and the Ability to Reflect and Employ Self-directed Learning are Powerful Tools for Developing Clinical Reasoning Skills
Learning clinical reasoning necessitated junior doctors to be internally driven for learning. Such internal motivation made them willing to learn from any source and be self-directed in their own learning. These individuals progressed rapidly in learning to reason with clinical problems compared to others who were not internally motivated.
Maintenance of internal motivation throughout the internship necessitated external encouragement even for the motivated particularly from the senior staff. There was a similar effect when the work environment fostered a culture of learning with the inclusion and recognition of junior doctors as a group of learners.
Table 2 presents participant quotations that highlight the significance of internal motivation in developing clinical reasoning skills.
|
“(reasoning with a complicated presentation) …With this kind of patient, it’ll refresh our memory. Going through how to take the history, how to use the basics, and how you investigate and manage…It is not like people coming with gastritis, or headache. Those are just simple things. (MP3, Medicine, Male, Phase-2) |
|
“I think you don’t need people who are good at what they do, I mean, you need people who are competent, but er…, you need a pleasant environment. Even if, there are, like 50 patients, if the people you work with are good, you can go through it. But then, if someone is really unpleasant, then that day is ruined.” (MP1, Medicine, Female, Phase-1) |
Table 2. Quotes illuminating internal motivation, reflective practice, and being self-directed as central to learning clinical reasoning skills
D. Caring and Compassionate Attitudes towards Patients Facilitate Developing Clinical Reasoning Skills
The individual caring and compassionate attitudes towards patients and the positive role modeling of senior doctors motivated junior doctors to learn clinical reasoning. Work experience nurtured these attitudes irrespective of gender, reflecting the potential to learn them during practice. However, a heavy workload and orientation towards efficiency in practice hindered the development of such attitudes among junior doctors.
“We’ve realised that although we’re members of a team, even individually, we can always do something for the patients. So, we always try to do something at our level. But we’re always willing to take the feeling from everyone above us to help.”
(MP1, Medicine, Female, Phase-1)
E. Collaborating within a Healthcare Team and Engaging in Ward Activities and Procedures Help Expedite the Development of Clinical Reasoning Skills
Junior doctors learn mostly from registrars, who are the immediate seniors and near-peers. In addition, peers and other healthcare staff contribute to their learning by timely sharing of information and working as a team. Patients’ unique characteristics which demand variation in reasoning also provide learning opportunities.
“I think the main influence is probably the registrars. Because we’re mostly in contact with them…So, in a way through working with them, I think I have learned quite a lot. Different ones will teach you different skills. Some are good at acute medicine and how to do that, and some are very willing to teach us how to do a pleural tap… So, from different people, we have learned different things.”
(MP2, Medicine, Male, Phase-1)
F. The Increasing Recognition of Professional Responsibility and Accountability towards Patient Care Drives Learning Clinical Reasoning
This was a strong theme commonly experienced by all junior doctors. During this transition, junior doctors recognised the patient care responsibilities vested in them and experienced a change of role from an undergraduate to a medical doctor. This led them to internalise their role and work towards meeting these expectations, whilst learning from all opportunities.
“We realise that somehow, we’ve got to do something. It wasn’t like that as students. (Now, as doctors) If we can’t take an ABG (Arterial Blood Gas) once, we will try ten times and somehow take the ABG. We realise- we have that ownership, “This is my patient. I will do something for her.” So, I think that’s a good thing. We didn’t have that as students.”
(MP1, Medicine, Female, Phase-1)
Parallel to the change of role, they were accepted as members of a community of doctors actively involved in providing patient care, which gave them a sense of inclusion and prestige and they worked hard towards meeting the expectations, which in turn helped them learn clinical reasoning.
G. Diversity of Personal, Interpersonal, and Contextual Factors Impede the Development of Clinical Reasoning Skills
Several negative influences on learning clinical reasoning exist.
The personal factors that can diminish learning clinical reasoning are related to a lack of internal motivation to learn and limited use of reflective practice.
In addition, external factors such as lack of encouragement and limited recognition of their contribution as doctors further demotivate junior doctors. Settings supervised by several senior clinicians provide better learning opportunities, but they also expose them to experience individual variations of reasoning due to staff working patterns and hinder their ability to appreciate the continuity of care.
Moreover, as junior doctors, they handle a heavy workload and work under time constraints, which gives them limited opportunity to reflect and learn from experience. Junior doctors also experience the presence of a power gap between juniors and seniors within the healthcare team and maintenance of this hierarchy is a barrier to learning during practice.
Table 3 presents participant quotes highlighting the diversity of contextual factors that hinder learning clinical reasoning skills.
|
“…usually hiccups occur with failures of… all types of failures… I do not have much knowledge about those things. Actually, I got to know that hiccups occur due to organ failure also, after this patient… (laughs)” (no intentions to learn more expressed) (SP2, Medicine, Male, Phase-2) |
|
“…here I think, in our unit, because the consultant changes daily, I think that is a negative point. The fact that you don’t have that connection with one person, and the fact that there is no continuity in care…” (MP1, Medicine, Female, Phase-1) |
|
“…I mean, there are too many admissions some days and you’re just trying to get through from one patient to the next one. So, you don’t really have that much time to analyse the problem as such. I mean, when the ward is less heavy, I’m trying to figure out what’s wrong but some days it’s a little bit… like going through.” (MP2, Medicine, Male) |
Table 3. Quotes illuminating contextual factors that impede the development of clinical reasoning skills
In addition, the discussions with junior doctors revealed that their main goal during the internship was to arrive at a diagnosis and/or manage patients’ clinical problems. No learning-related goals were readily verbalised.
(When enquired about the goals of reasoning during the internship)
“That…..err…is… coming to a final diagnosis and starting the treatment…Basically, we are supposed to recognise life-threatening conditions and treat them.”
(MP3, Medicine, Male, Phase-2)
Similarly, the informal discussions with senior clinicians revealed their limited expectations of the contribution of the internship towards facilitating the development of clinical reasoning skills among juniors. This could be due to the service orientation of the internship leaving ‘learning to happen’ concurrently without being actively encouraged. This is not conducive to learning clinical reasoning.
H. The Construction of the ‘practice-oriented clinical reasoning skills development framework’
Embedded within the seven themes were a multitude of factors that could be clearly categorised as ‘Facilitators’, ‘Drivers’, ‘Sources’, and ‘Challenges’ of developing clinical reasoning skills. These factors helped junior doctors to migrate from a disease-oriented to a practice-oriented approach to clinical reasoning (Figure 1).
The categorisation was informed by how these factors influenced the development of clinical reasoning skills. ‘Facilitators’ actively support learning, while ‘drivers’ exert strong internal pressure to motivate learning clinical reasoning. A ‘source’ is an individual or an activity, that helps learn clinical reasoning through interacting with them. ‘Challenges’ are either internal or external to an individual and negatively influence the development of clinical reasoning skills.
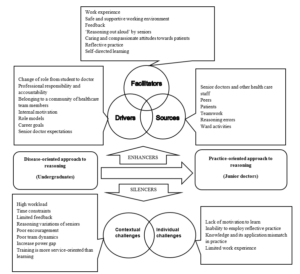
Figure 1. ‘Practice-oriented clinical reasoning skills development framework’ highlighting the factors that influence the development of clinical reasoning skills during the transition from medical graduates to junior doctors
IV. DISCUSSION
Aligned with existing literature (Brennan et al., 2010; Lempp et al., 2005; Prince et al., 2000; Teunissen & Westerman, 2011), this study identified a steep learning curve for junior doctors in developing clinical reasoning skills upon commencing the internship. A ‘disjunction’ (Koufidis et al., 2020) was evident between knowledge acquired during medical undergraduate education and the demands of effective reasoning in clinical practice (Cave et al., 2009; Monrouxe et al., 2017). The ‘practice-oriented clinical reasoning skills development framework’ derived from this study shed light on the factors serving as ‘enhancers’ and ‘silencers’ of learning clinical reasoning skills during this critical period. This classification helps consolidate existing knowledge specific to this period and offers insights for addressing disconnections and facilitating the development of clinical reasoning skills.
In this study, novice doctors initially faced clinical reasoning challenges due to limited contextual understanding and reliance on rule-based reasoning comparable to the Dreyfus model of adult skill acquisition (2004). With increased work experience, they were able to promptly recognise contextual features distinguishing acute from non-acute presentations requiring urgent care. Additionally, they acknowledged the significance of the patient’s past medical history in forming a broader approach to reasoning. Some even acquired instincts for prompt clinical decision-making, a form of non-analytic reasoning identified by clinical experts (Norman et al., 2007) and blending non-analytic reasoning with occasional rule-based confirmation (analytic reasoning). This dual-process approach (Croskerry, 2009; Eva, 2004; Pelaccia et al., 2011), incorporating both analytic and non-analytic reasoning is recognised to overcome challenges associated with each approach. Such development of clinical reasoning skills with work experience is reflective of the advancement of reasoning skills along the first four stages of the Dreyfus model, from novice to proficiency stages. This contrasts with the limited value placed on the internship for developing clinical reasoning skills among some clinical supervisors and needs addressing during staff development initiatives.
It was also noted that junior doctors revert to the novice stage using more analytical rule-based reasoning with uncommon presentations or at the start of a new rotation in another specialty (Groves, 2012). This highlights the complexity of developing clinical reasoning skills, varying with the nature of the presentation and the clinical specialty, requiring more support for its development. This aligns with the ‘context-specific nature’ of clinical reasoning (Eva et al., 1998), the variation of reasoning outcomes of an individual due to contextual factors unique to clinical situations. The study revealed a clear influence of clinical specialty on reasoning, confining the development of clinical reasoning to a few focused clinical problems common to a particular specialty. This limits the overall development of clinical reasoning and hinders the momentum of clinical reasoning development entering a new clinical specialty. Therefore, clinical teachers should promote a comprehensive approach, considering differential diagnoses beyond a single specialty. Given the need for promptly recognising contextual features of disease severity in acute care settings coupled with early internship challenges, delaying trainees’ placement in acute care settings until later in a clinical rotation is a reasonable approach, contrary to current clinical practice.
Work experience was central to developing clinical reasoning skills (Charlin et al., 2007; Schmidt & Rikers, 2007; Schmidt & Boshuizen, 1993), but benefiting from experience required junior doctors to be internally motivated. According to the self-determination theory, when an individual experiences a feeling of being able to do something successfully (competence), when their actions are controlled internally or self-determined (autonomy), and when there is a sense of safety, belonging, and supportive relationships (relatedness), it enhances the intrinsic motivation of an individual (Ryan & Deci, 2000) and this was clearly noted during this study. The ‘drivers’, ‘facilitators’, and ‘sources’ of learning clinical reasoning identified during this study enabled fulfilling these three basic psychological needs required to be motivated to learn clinical reasoning. Hence, the ‘practice-oriented clinical skills development framework’ could serve as a valuable reference for clinical teachers supporting junior doctors in developing clinical reasoning skills during their transition to the workplace.
Echoing the evidence in the field (Ajjawi & Higgs, 2008; Gruppetta & Mallia, 2020), junior doctors recognised the change in their role from student to medical doctor and subsequent absorption into the healthcare team which made them internalise their responsibility and accountability towards patient care. Their engagement in patient care gradually increased to finally becoming valued members of this community, collaborating with other like-minded colleagues to develop a more deliberate understanding of reasoning and methods of using it. This aligns with the principles of legitimate peripheral participation and community of practice of the Situated Learning Theory (O’Brien & Battista, 2020). The community of practice created a safe learning environment, motivating junior doctors to learn clinical reasoning actively. This emphasises the significance of early integration of junior doctors as valued members of the healthcare team. A team-oriented approach to patient care, acknowledging every team member’s contribution, proves more beneficial here than an individual-focused hierarchical approach.
The junior doctors of this study learned through their interactions with senior doctors, peers, and other healthcare staff, as well as by actively participating in ward activities, revealing learning as a dynamic social act. The opportunity to observe, listen to, and emulate senior colleagues as they engaged in clinical reasoning with authentic patient presentations, followed by the application of the newly acquired skills, significantly influenced the development of their clinical reasoning skills. This highlights the continued relevance of apprenticeship as a pedagogical tool today (Dornan, 2005), facilitating the ongoing development of clinical reasoning skills among junior doctors. It also provides a unique opportunity to witness firsthand the decision-making processes of junior doctors operating independently in clinical practice, aligning with the highest level of clinical skills assessment in Miller’s pyramid (Miller, 1990). This presents a potential opening for formative assessment of clinical reasoning, whether conducted formally or informally, as part of junior doctor training.
Junior doctors also constructed knowledge through interpersonal interactions in the workplace by engaging in an iterative process of learning, application, and consolidation of knowledge with each experience contributing to the refinement of their clinical reasoning skills. Learning from these experiences required them to reflect on these experiences and arrive at new understandings by integrating and building on previous knowledge. This is aligned with the principles of experiential learning theory (Morris, 2020; Yardley et al., 2012) and the constructivism learning theory (Olusegun, 2015). This highlights the importance of encouraging reflection by proactively including junior doctors in all pertinent patient-related discussions. Also, the value of implementing a reflective portfolio to acknowledge junior doctors’ learning needs at the outset of the internship, with formative assessments conducted midway and at its conclusion by clinical supervisors. This could also introduce a learning orientation to the already service-focused internship placement.
Junior doctors found collaborative learning, including referrals to other specialties and engaging in those discussions or working in partnerships with peers, beneficial for developing clinical reasoning (Laal & Laal, 2012; Tolsgaard et al., 2016). This highlights the value of involving junior doctors in collaborative work within or across disciplines. Simulation-based training (Khan et al., 2011) offers similar opportunities for collaborative learning within a safe environment, without compromising patient safety. Integrating simulation-based training for junior doctors immediately after graduation or before the internship can equip them with reasoning skills for authentic practice, addressing challenges during their transition to the workplace.
The caring and compassionate attitudes instilled in junior doctors by their seniors and further nurtured through close patient interactions, served as indirect motivators for learning clinical reasoning skills. This is an area not widely discussed in literature. While there is acknowledgment of the potential influence of clinicians’ emotions on clinical reasoning (Kozlowski et al., 2017), the specific impact of emotional closeness in patient care, and whether it aligns with the conventions of a more objective, rule-based healthcare delivery system, remains an area that merits more comprehensive investigation (Dreyfus, 2004). However, the study findings support that the more emotionally closer the junior doctors are to their patients, the more they are invested in learning clinical reasoning to ensure healthier outcomes for their patients. Clinical teachers could nurture such attitudes through role modeling as noted in this study.
The interrupted supervisory relationships due to work rotations of the senior staff challenged learning clinical reasoning. Such system-related factors deprived junior doctors of learning by emulating senior practice. It also hampered their ability to appreciate the continuity of patient care due to individual variations of reasoning among senior staff and prevented developing closer relationships with seniors, which could have been more emotionally satisfying (Ryan & Deci, 2000). This underlines the need to take necessary steps to prevent any adverse effects of staff working patterns on trainee doctors, while simultaneously ensuring extended periods of supervision within a consistent healthcare team.
The collective findings of this study not only confirm but also add valuable insights to the clinical reasoning pathway for teaching clinical reasoning skills (Linn et al., 2012). According to this framework, the teaching of clinical reasoning occurs in three stages through three consultations. Stage 1- Demonstration and deconstruction, Stage 2- Comprehension, and Stage 3- Performance. The transition in focus from the teacher’s approach to the student’s performance occurs in the last stage. In junior doctor training, this framework is ideally applied within a team context during daily clinical ward rounds focusing on selected patient presentations as afforded by the time constraints. The three stages of the framework can be combined, and the reasoning discussions can be brief and can take place within the ward round after the selected presentations with increasing junior doctors’ involvement as they gain experience. This could allow junior doctors to learn from verbalised reasoning from the team, reflect and actively contribute to the discussion, and feel valued as team members. They can apply newly acquired reasoning skills in subsequent patient consultations independently, in addition to the opportunity to demonstrate these during the ward rounds. Based on the study findings, additional considerations for analysing patient presentations could be proposed as enhancements to the clinical reasoning pathway (Linn et al., 2012). These aspects are detailed within the overall structure of this framework in Figure 2.
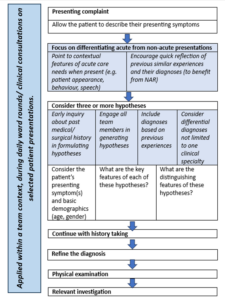
Figure 2. Proposed additions to the deconstructed consultation according to the clinical reasoning pathway (Linn et al., 2012) for teaching clinical reasoning to junior doctors as part of daily clinical ward rounds
Additions are presented in italics and highlighted. (NAR- non-analytic reasoning)
V. CONCLUSION
The ‘practice-oriented clinical skills development framework’ has brought together factors that act as ‘enhancers’ and ‘silencers’ of learning clinical reasoning specific to this period of transition from medical graduates to junior doctors. These findings offer practical insights that can prove invaluable for clinical educators in their teaching practices to facilitate the development of clinical reasoning skills.
This research also offers insights into the responsibilities of clinical teachers in supporting the development of clinical reasoning skills among junior doctors during their internship. It provides suggestions for teaching these skills in practice and highlights potential system-related changes needed to facilitate this process.
A. Limitations of the Study
The reader needs to determine the applicability of the findings to their context to overcome the limitations of qualitative research. To facilitate this process, the methodology and the data analysis are appropriately detailed.
The study focused on immediate medical graduates, and therefore, it did not delve into the clinical reasoning experiences of junior doctors at different levels of seniority and training, although this could have added to our understanding. This lack of comparative analysis is another limitation of this study.
Notes on Contributors
Dr WCD Karunaratne conceptualised the study, prepared the study proposal, conducted all interviews, analysed them and developed the manuscript for this submission.
Professor Madawa Chandratilake was a supervisor of this study and he contributed to the study design, guided initial interviews, and analysed selected transcripts to finalise the final coding framework for the study. He also reviewed and provided feedback on different versions of the manuscript.
Professor Kosala Marambe was also a supervisor of the study. She contributed to the study design and analysis of selected transcripts to finalise the final coding framework for the study and provided feedback on different versions of the manuscript.
Ethical Approval
Ethical clearance (P/11/01/16) was obtained from the Faculty of Medicine, University of Kelaniya, Sri Lanka.
Data Availability
Institutional ethical clearance was given to maintain the data in the secure storage of the principal investigator of the study. However, additional supportive quotations are deposited in the repository (Karunaratne et al., 2023) and are available from this URL – https://doi.org/10.6084/m9.figshare.23536548.v2.
Readers may contact the principal researcher for additional data and details if required.
Acknowledgement
We would like to acknowledge Dr Pavithra Godamunne (Faculty of Medicine, University of Kelaniya, Sri Lanka) who applied and secured funding for the project and Dr Paul Crampton (Hull York Medical School, UK) who reviewed the manuscript and provided constructive comments.
Funding
University of Kelaniya, Sri Lanka funded this research study (No. RP/03/04/17/01/16).
Declaration of Interest
The authors have no conflicts of interest to disclose.
References
Ajjawi, R., & Higgs, J. (2007). Using hermeneutic phenomenology to investigate how experienced practitioners learn to communicate clinical reasoning. The Qualitative Report, 12(4), 612–638. https://doi.org/10.46743/2160-3715/2007.1616
Ajjawi, R., & Higgs, J. (2008). Learning to reason: A journey of professional socialisation. Advances in Health Sciences Education, 13, 133–150. https://doi.org/10.1007/s10459-006-9032-4
Braun, V., & Clarke, V. (2012). Thematic Analysis. In APA Handbook of Research Methods in Psychology, 2, 57-71. https://doi.org/10.1037/13620-004
Brennan, N., Corrigan, O., Allard, J., Archer, J., Barnes, R., Bleakley, A., Collett, T., & De Bere, S. R. (2010). The transition from medical student to junior doctor: Today’s experiences of tomorrow’s doctors. Medical Education, 44(5), 449–458. https://doi.org/10.1111/j.1365-2923.2009.03604.x
Cameron, A., Millar, J., Szmidt, N., Hanlon, K., & Cleland, J. (2014). Can new doctors be prepared for practice? A review. Clinical Teacher, 11(3), 188–192. https://doi.org/10.1111/tct.12127
Cave, J., Woolf, K., Jones, A., & Dacre, J. (2009). Easing the transition from student to doctor: How can medical schools help prepare their graduates for starting work? Medical Teacher, 31(5), 403–408. https://doi.org/10.1080/01421590802348127
Charlin, B., Boshuizen, H. P. A., Custers, E. J., & Feltovich, P. J. (2007). Scripts and clinical reasoning. Medical Education, 41(12), 1178–1184. https://doi.org/10.1111/j.1365-2923.2007.02924.x
Charlin, B., Tardif, J., & Boshuizen, H. P. A. (2000). Scripts and medical diagnostic knowledge: Theory and applications for clinical reasoning instruction and research. Academic Medicine, 75(2), 182–190. https://doi.org/10.1097/00001888-200002000-00020
Cohen, L., Manion, L., & Morrison, K. (2017). Research methods in education (8th ed.). Routledge. https://doi.org/10.4324/9781315456539
Croskerry, P. (2009). A universal model of diagnostic reasoning. Academic Medicine, 84(8), 1022–1028. https://doi.org/10.1097/ACM.0b013e3181ace703
Crotty, M. (1998). Foundations of social research: Meaning and perspective in the research process (1st ed.). Routledge. https://doi.org/10.4324/9781003115700
Dornan, T. (2005). Osler, Flexner, apprenticeship and “the new medical education.” Journal of the Royal Society of Medicine, 98(3), 91–95. https://doi.org/10.1177/014107680509800302
Dreyfus, S. E. (2004). The five-stage model of adult skill acquisition. Bulletin of Science, Technology and Society, 24(3), 177–181. https://doi.org/10.1177/0270467604264992
Durning, S., Artino, A. R., Jr., Pangaro, L., van der Vleuten, C. P. M., & Schuwirth, L. (2011). Context and clinical reasoning: Understanding the perspective of the expert’s voice. Medical Education, 45(9), 927–938. https://doi.org/10.1111/j.1365-2923.2011.04053.x
Durning, S. J., & Artino, A. R. (2011). Situativity theory: A perspective on how participants and the environment can interact: AMEE guide no. 52. Medical Teacher, 33(3), 188-199. https://doi.org/10.3109/0142159x.2011.550965
Durning, S. J., Artino, A. R., Jr., Schuwirth, L., & van der Vleuten, C. (2013). Clarifying assumptions to enhance our understanding and assessment of clinical reasoning. Academic Medicine, 88(4), 442-448. https://doi.org/10.1097/acm.0b013e3182851b5b
Ericsson, K. A. (2004). Deliberate practice and the acquisition and maintenance of expert performance in medicine and related domains. Academic Medicine, 79(10 Suppl), S70–S81. https://doi.org/10.1097/00001888-200410001-00022
Eva, K., Neville, J., & Norman, G. (1998). Exploring the etiology of content specificity: Factors influencing analogic transfer and problem solving. Academic medicine, 73(10), S1-S5. https://doi.org/10.1097/00001888-199810000-00028
Eva, K. W. (2004). What every teacher needs to know about clinical reasoning. Medical Education, 39(1), 98–106. https://doi.org/10.1111/j.1365-2929.2004.01972.x
Goldacre, M. J., Davidson, J. M., & Lambert, T. W. (2003). Doctors’ views of their first year of medical work and postgraduate training in the UK: Questionnaire surveys. Medical Education, 37(9), 802–808. https://doi.org/10.1046/j.1365-2923.2003.01611.x
Graber, M. L., Franklin, N., & Gordon, R. (2005). Diagnostic error in internal medicine. Archives of Internal Medicine, 165(13), 1493–1499. https://doi.org/10.1001/archinte.165.13.1493
Groves, M. (2012). Understanding clinical reasoning: The next step in working out how it really works. Medical Education, 46(5), 444–446. https://doi.org/10.1111/j.1365-2923.2012.04244.x
Gruppetta, M., & Mallia, M. (2020). Clinical reasoning: Exploring its characteristics and enhancing its learning. British Journal of Hospital Medicine, 81(10), 1–9. https://doi.org/10.12968/hmed.2020.0227
Hattie, J., & Timperley, H. (2007). The power of feedback. Review of Educational Research, 77(1), 81–112. https://doi.org/10.3102/003465430298487
Health Services Safety Investigation Body. (2022). Investigation report: Clinical decision making- diagnosis and treatment of pulmonary embolism in emergency departments. Retrieved from https://www.hssib.org.uk/patient-safety-investigations/clinical-decision-making-diagnosis-of-pulmonary-embolism-in-emergency-departments/investigation-report/
Huckman, R. S., & Barro, J. R. (2005). NBER working paper series cohort turnover and productivity: The July phenomenon in teaching hospitals. Retrieved from http://www.nber.org/papers/ w11182
Jen, M. H., Bottle, A., Majeed, A., Bell, D., & Aylin, P. (2009). Early in-hospital mortality following trainee doctors’ first day at work. PLoS ONE, 4(9), Article e7103. https://doi.org/10.1371/jo urnal.pone.0007103
Kafle, N. P. (2011). Hermeneutic phenomenological research method simplified. Bodhi: An Interdisciplinary Journal, 5(1), 181–200. https://doi.org/10.3126/bodhi.v5i1.8053
Karunaratne, D., Chandratilake, M., & Marambe, K. (2023). Annexure-1 Additional supportive quotations (Version 2). [Data set]. Figshare. https://doi.org/10.6084/m9.figshare.23536548.v2
Khan, K., Pattison, T., & Sherwood, M. (2011). Simulation in medical education. Medical Teacher 33(1), 1-3. https://doi.org/10.3109/0142159X.2010.519412
Koufidis, C., Manninen, K., Nieminen, J., Wohlin, M., & Silén, C. (2020). Grounding judgement in context: A conceptual learning model of clinical reasoning. Medical Education, 54(11), 1019–1028. https://doi.org/10.1111/medu.14222
Kozlowski, D., Hutchinson, M., Hurley, J., Rowley, J., & Sutherland, J. (2017). The role of emotion in clinical decision making: An integrative literature review. BMC Medical Education, 17(1), Article 255. https://doi.org/10.1186/s12909-017-1089-7
Laal, M., & Laal, M. (2012). Collaborative learning: What is it? Procedia Social and Behavioral Sciences, 31, 491–495. https://doi.org/10.1016/j.sbspro.2011.12.092
Langridge, N., Roberts, L., & Pope, C. (2015). The clinical reasoning processes of extended scope physiotherapists assessing patients with low back pain. Manual Therapy, 20(6), 745-750. https://doi.org/10.1016/j.math.2015.01.005
Lave, J. (1991). Situating learning in communities of practice. In L. B. Resnick, J. M. Levine, & S. D. Teasley (Eds.), Perspectives on socially shared cognition (pp. 63–82). American Psychological Association. https://doi.org/10.1037/10096-003
Laverty, S. M. (2003). Hermeneutic phenomenology and phenomenology: A comparison of historical and methodological considerations. International Journal of Qualitative Methods, 2(3), 21–35. https://doi.org/10.1177/160940690300200303
Lee, C. Y., Jenq, C. C., Chandratilake, M., Chen, J., Chen, M. M., Nishigori, H., Wajid, G., Yang, P. H., Yusoff, M. S. B., & Monrouxe, L. (2021). A scoping review of clinical reasoning research with Asian healthcare professionals. Advances in Health Sciences Education, 26(5), 1555–1579. https://doi.org/10.1007/s10459-021-10060-z
Lempp, H., Seabrook, M., Cochrane, M., & Rees, J. (2005). The transition from medical student to doctor: Perceptions of final year students and preregistration house officers related to expected learning outcomes. International Journal of Clinical Practice, 59(3), 324–329. https://doi.org/10.1111/j.1742-1241.2005.00 438. x
Linn, A., Khaw, C., Kildea, H., & Tonkin, A. (2012). Clinical reasoning: A guide to improving teaching and practice. Australian Family Physician, 41(1), 18–20. https://search.informit.org/doi/10. 3316/informit.875577247352301
Malterud, K., Siersma, V. D., & Guassora, A. D. (2016). Sample size in qualitative interview studies: Guided by information power. Qualitative Health Research, 26(13), 1753-1760. https://doi.org/10.1177/1049732315617444
Mamede, S., Schmidt, H. G., & Penaforte, J. C. (2008). Effects of reflective practice on the accuracy of medical diagnoses. Medical Education, 42(5), 468–475. https://doi.org/10.1111/j.1365-2923. 2008.03030.x
Mamede, S., van Gog, T., Moura, A. S., de Faria, R. M. D., Peixoto, J. M., Rikers, R. M. J. P., & Schmidt, H. G. (2012). Reflection as a strategy to foster medical students’ acquisition of diagnostic competence. Medical Education, 46(5), 464–472. https://doi.org/10.1111/j.1365-2923.2012.04217.x
Miller, G. (1990). The assessment of clinical skills/competence/performance. Academic Medicine, 65(9), S63–S67. https://doi.org/10.1097/00001888-199009000-00045
Monrouxe, L. V., Grundy, L., Mann, M., John, Z., Panagoulas, E., Bullock, A., & Mattick, K. (2017). How prepared are UK medical graduates for practice? A rapid review of the literature 2009-2014. British Medical Journal Open, 7, Article e013656. https://doi.org/10.1136/bmjopen-2016-013656
Morris, T. H. (2020). Experiential learning – A systematic review and revision of Kolb’s model. Interactive Learning Environments, 28(8), 1064–1077. https://doi.org/10.1080/10494820.2019.15702 79
Muylaert, C. J., Sarubbi, V., Jr., Gallo, P. R., Neto, M. L. R., & Reis, A. O. A. (2014). Narrative interviews: An important resource in qualitative research. Revista Da Escola de Enfermagem Da USP, 48, 184–189. https://doi.org/10.1590/s0080-623420140000800027
Norman, G. (2005). Research in clinical reasoning: Past history and current trends. Medical Education, 39(4), 418–427. https://doi.org/10.1111/j.1365-2929.2005.02127.x
Norman, G., Young, M., & Brooks, L. (2007). Non-analytical models of clinical reasoning: The role of experience. Medical Education, 41(12), 1140–1145. https://doi.org/10.1111/j.1365-292 3.2007.02914.x
O’Brien, B. C., & Battista, A. (2020). Situated learning theory in health professions education research: A scoping review. Advances in Health Sciences Education, 25(2), 483–509. https://doi.org/10.1007/s10459-019-09900-w
Olusegun, S. (2015). Constructivism learning theory: A paradigm for teaching and learning. IOSR Journal of Research & Medical Edication, 5(6), 66–70.
Pelaccia, T., Tardif, J., Triby, E., & Charlin, B. (2011). An analysis of clinical reasoning through a recent and comprehensive approach: The dual-process theory. Medical Education Online, 16(1), Article 5890. https://doi.org/10.3402/meo.v16i0.5890
Prince, K. J. A. H., Van de Wiel, M. W. J., Scherpbier, A. J. J. A., Van der Vleuten, C. P. M., & Boshuizen, H. P. A. (2000). A qualitative analysis of the transition from theory to practice in undergraduate training in a PBL-medical school. Advances in Health Sciences Education, 5, 105–116. https://doi.org/10.1023/a:1009873003677
Prince, K. J. A. H., Van de Wiel, M. W. J., Van der Vleuten, C. P. M., Boshuizen, H. P. A., & Scherpbier, A. J. J. A. (2004). Junior doctors’ opinions about the transition from medical school to clinical practice: A change of environment. Education for Health, 17(3), 323–331. https://doi.org/10.1080/13576280400002510
Robertson, D. (2012). Critical thinking and clinical reasoning in new graduate Occupational therapists: A phenomenological study. [Doctoral Dissertation, Robert Gordan University]. OpenAIR@RGU. http://hdl.handle.net/10059/792
Ryan, R. M., & Deci, E. L. (2000). Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. American Psychologist, 55(1), 68–78. https://doi.org/10.1037/0003-066X.55.1.68
Schmidt, H., & Rikers, R. (2007). How expertise develops in medicine: Knowledge encapsulation and illness script formation. Medical Education, 41(12), 1133–1139. https://doi.org/10.1111/j. 1365-2923.2007.02915.x
Schmidt, H. G., & Boshuizen, H. P. A. (1993). On acquiring expertise in medicine. Educational Psychology Review, 5(3), 205–221. https://doi.org/10.1007/BF01323044
Tallentire, V. R., Smith, S. E., Facey, A. D., & Rotstein, L. (2017). Exploring newly qualified doctors’ workplace stressors: An interview study from Australia. British Medical Journal Open, 7, e015890. https://doi.org/10.1136/bmjopen-2017-015890
Tallentire, V. R., Smith, S. E., Skinner, J., & Cameron, H. S. (2011). Understanding the behaviour of newly qualified doctors in acute care contexts. Medical Education, 45(10), 995–1005. https://doi.org/10.1111/j.1365-2923.2011.04024.x
Taylor, D. C. M., & Hamdy, H. (2013). Adult learning theories: Implications for learning and teaching in medical education: AMEE Guide No. 83. Medical Teacher, 35(11), e1561–e1572. https://doi.org/10.3109/0142159X.2013.828153
Teunissen, P. W., & Westerman, M. (2011). Opportunity or threat: The ambiguity of the consequences of transitions in medical education. Medical Education, 45(1), 51–59. https://doi.org/10.1111/j.1365-2923.2010.03755.x
Tolsgaard, M. G., Kulasegaram, K. M., & Ringsted, C. V. (2016). Collaborative learning of clinical skills in health professions education: The why, how, when and for whom. Medical Education, 50(1), 69–78. https://doi.org/10.1111/medu.12814
Varpio, L., Ajjawi, R., Monrouxe, L. V., O’Brien, B. C., & Rees, C. E. (2017). Shedding the cobra effect: Problematising thematic emergence, triangulation, saturation and member checking. Medical Education, 51, 40–50. https://doi.org/10.1111/medu.13124
Woods, N. N. (2007). Science is fundamental: The role of biomedical knowledge in clinical reasoning. Medical Education, 41(12), 1173–1177. https://doi.org/10.1111/j.1365-2923.2007.029 11.x
Yardley, S., Teunissen, P. W., & Dornan, T. (2012). Experiential learning: AMEE Guide No. 63. Medical Teacher, 34(2), e102–e115. https://doi.org/10.3109/0142159X.2012.650741
*WCD Karunaratne
Centre for Medical Education,
University of Dundee
Scotland, DD2 4BF
+44 7594 504928
Email: dilminikarunaratne@gmail.com / Wkarunaratne001@dundee.ac.uk
Announcements
- Fourth Thematic Issue: Call for Submissions
The Asia Pacific Scholar is now calling for submissions for its Fourth Thematic Publication on “Developing a Holistic Healthcare Practitioner for a Sustainable Future”!
The Guest Editors for this Thematic Issue are A/Prof Marcus Henning and Adj A/Prof Mabel Yap. For more information on paper submissions, check out here! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Volume 9 Number 1 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors. - Volume 8 Number 3 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2021
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2021.
Refer here for the list of recipients. - Most Accessed Article 2021
The Most Accessed Article of 2021 goes to Professional identity formation-oriented mentoring technique as a method to improve self-regulated learning: A mixed-method study.
Congratulations, Assoc/Prof Matsuyama and co-authors. - Best Reviewer Awards 2020
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2020.
Refer here for the list of recipients. - Most Accessed Article 2020
The Most Accessed Article of 2020 goes to Inter-related issues that impact motivation in biomedical sciences graduate education. Congratulations, Dr Chen Zhi Xiong and co-authors.









