General dental practitioners’ perceptions on Team-based learning pedagogy for continuing dental education
Submitted: 14 April 2021
Accepted: 24 June 2021
Published online: 4 January, TAPS 2022, 7(1), 98-101
https://doi.org/10.29060/TAPS.2022-7-1/SC2517
Lean Heong Foo & Marianne Meng Ann Ong
Department of Restorative Dentistry, National Dental Centre Singapore, Singapore
Abstract
Introduction: Team-based learning (TBL) pedagogy is a structured, flipped classroom approach to promote active learning. In April 2019, we designed a TBL workshop to introduce the New Classification of Periodontal Diseases 2017 to a group of general dental practitioners (GDPs). We aimed to investigate GDPs feedback on learning this new classification using TBL pedagogy.
Methods: Two articles related to the 2017 classification were sent to 22 GDPs 2 weeks prior to a 3-hour workshop. During the face-to-face session, they were randomly assigned to five groups. They participated in individual and group readiness assurance tests. Subsequently, the GDPs had inter- and intragroup facilitated discussions on three simulated clinical cases. They then provided feedback using a pen-to-paper survey. Based on a 5-point Likert scale (1-strongly disagree to 5-strongly agree), they indicated their level of agreement on items related to the workshop and their learning experience.
Results: Majority (94.7%, 18 out of 19 GDPs) agreed the session improved their understanding of the new classification and they preferred this TBL pedagogy compared to a conventional lecture. All learners agreed they can apply the knowledge to their work and there was a high degree of participation and involvement during the session. They found the group discussion and the simulated clinical cases useful.
Conclusion: A TBL workshop is suitable for clinical teaching of the New Classification of Periodontal Diseases 2017 for GDPs. Its structure promotes interaction among learners with the opportunity to provide feedback and reflection during the group discussions. This model might be a good pedagogy for continuing dental education.
Keywords: Team-based Learning, General Dental Practitioners, New Classification of Periodontal Diseases
I. INTRODUCTION
Team-based learning (TBL) is a flipped classroom, structured learning pedagogy that was introduced by Larry Michaelsen and has gained popularity among healthcare educators recently. TBL is learner-centric and dialectic based, and practices logical discussion used for determining the truth of a theory or opinion (Michaelsen et al., 2008). It provides the opportunity for peer-teaching by group members and can assist weaker students in understanding course materials.
Several dental educators have utilised TBL in undergraduate dentistry programmes and observed higher engagement among learners, less student contact time and faculty time, and higher course grades (Haj-Ali & Al Quran, 2013). General dental practitioners (GDPs), unlike undergraduate dental students, juggle between busy dental practice and family life. Hence, GDPs might seek active learning with direct knowledge application to manage their continuing dental education needs efficiently. The World Workshop of Periodontology recently revamped the diagnosis of periodontal diseases and proposed a new classification of staging (Stage I-IV; based on severity of disease) and grading (Grade A-C; based on disease progression) for periodontitis (Tonetti et al., 2018). We aimed to investigate GDP feedback on learning this new classification using TBL pedagogy.
II. METHODS
This is a descriptive study on GDPs’ feedback on learning the New Classification of Periodontal Diseases 2017 using a TBL approach. 22 GDPs attended the TBL workshop in April 2019.
Two articles related to the new classification were sent to the GDPs 2 weeks prior to the 3-hour workshop. Five multiple-choice questions were crafted from the two articles (Individual Readiness Assurance Test, IRAT) to assess learners’ basic understanding of the new classification. Learners were divided into five groups to discuss IRAT and provide answers using the immediate feedback assessment technique card (Group Readiness Assurance Test, GRAT). Faculty then highlighted key elements of the new classification. Three clinical periodontal cases crafted based on the 4S framework principles i.e. same problem, significant problem, specific choice, and simultaneous reporting, were used in the application process (Michaelsen et al., 2008). The key question was to diagnose the periodontal condition based on the staging and grading criteria. Lastly, learners provided implied consent by answering an anonymous pen-to-paper survey voluntarily. They answered based on their level of agreement on a 5-point Likert scale (5 indicating strongly agree, 1 indicating strongly disagree). The survey comprising 13 education-related statements: two statements related to programme content, two to presentation, six to learning experience, and three about the workshop. Three qualitative questions in the survey were: “What do you like most about the workshop?”, “What aspects of the session could be improved?” and “Other comments and feedback”.
III. RESULTS
Nineteen out of the 22 GDPs who attended the TBL workshop responded to the survey (response rate 86.4%). Results are summarised in Figure 1. We conducted a reliability analysis on the perceived task values scale comprising two subscales (learning experience and workshop) with at least three items.
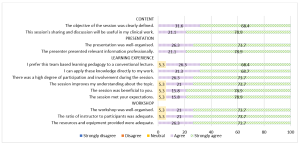
Figure 1. Learners’ feedback about the workshop
A. Content (Two items)
During the workshop, we highlighted the staging and grading criteria for the new classification. Learners provided a mean score of 4.74 (standard deviation, SD, 0.446; median 5) in two statements related to content. In general, 68.4% of them strongly agreed and 31.6% agreed the objective of the workshop was clearly defined. There were 78.9% and 21.1% of learners who strongly agreed and agreed respectively that the sharing and discussion during the workshop was useful to their clinical work.
B. Presentation (Two items)
Learners gave a mean score of 4.76 for presentation (SD 0.431; median 5). There were 73.7% learners who strongly agreed and 26.3% who agreed that the presentation was well-organised. In addition, 78.9% and 21.1% of the learners strongly agreed and agreed respectively that the presenter presented relevant information professionally.
C. Learning Experience (Six items)
Cronbach’s alpha for the learning experience subscale reached acceptable reliability at α = 0.81. The mean score for learning experience was 4.70 (SD 0.531; median 5). There were 68.4% learners who strongly agreed and 26.3% who agreed that they prefer TBL pedagogy to a conventional lecture. Also, 68.7% of the learners strongly agreed and 31.3% agreed they could apply the knowledge directly to their work. All learners agreed that there was a high degree of participation and involvement during the session. 18 learners (94.7%) agreed that the session met their expectations and improved their understanding about the topic.
D. Workshop (Three items)
The mean score for learners’ feedback on the workshop was 4.71 (SD 0.533; median 5). 18 learners (94.7%) agreed that the workshop was well organised with an adequate ratio of instructor to participants (2:22). There were 73.7% learners who strongly agreed and 26.3% who agreed that resources and equipment provided were adequate. Cronbach’s alpha for the workshop subscale reached acceptable reliability at α = 0.75.
E. Qualitative Feedback
The learners cited the following themes as their favourite component of the workshop: “group interaction and discussion” (4), “clinical case discussion” (3), “useful and relevant clinical cases” (1), “interesting readiness assurance test” (1), and “pre-reading material” (1). They also cited “active learning” (1), “correct wrong understanding” (1), “discussion improves my understanding” (1), and “great information and lecturer” (1) as positive learning experiences. Three different learners provided feedback of “best workshop ever attended”, “well done”, and “very good” respectively. One learner commented that the air-conditioning in the room was cold. One learner commented on small font size in dental charting and another learner suggested “less tests at the start”.
IV. DISCUSSION
The flipped classroom concept in TBL was suitable for GDPs to study the pre-reading articles at their own pace. The structured workshop enabled them to correct any misconception immediately and deepen their understanding about the new classification. This observation concurs with the finding that all GDPs agreed they could apply the knowledge to their work and preferred this pedagogy over a traditional lecture. This active learning process differs from a conventional didactic lecture, which is faculty-centric with less feedback and interaction. Hence, this pedagogy can be applied for some continuing dental education programmes by improving the delivery and application of new concepts. The 4S framework in the application cases are key elements to promote productive and logical discussion similar to a debate facilitated by faculty. The problem-solving aspect of TBL, along with the scaffolding and guidance by faculty, can enhance the metacognition process among learners (Hrynchak & Batty, 2012). Almost all learners agreed there was an adequate ratio of faculty to participants, emphasising the benefit of using TBL workshops to teach a large group of learners with less faculty. However, faculty needs to work more in planning and preparing the teaching materials, executing, and facilitating the session following the TBL structure and process. In addition, hurdles in conducting TBL include acceptance from faculty and learners, difficulty in supervising a large group, the customisation of the course content, and adequate training and expertise to conduct TBL effectively.
The learners also cited “group interaction and discussion” as their favourite component of the workshop. The learning theory underpinning TBL is the constructivist learning theory where the faculty exposes knowledge inconsistency during group discussion, subsequently allowing a new mental framework to be built upon the new understanding (Hrynchak & Batty, 2012). TBL is useful in healthcare education since it can promote good critical thinking and teamwork. In addition, the intra- and intergroup formal discussion provides the opportunity to reflect, give feedback, and enable peer-teaching. Self-reflection enables learners to make a judgement when modifying their existing knowledge. Peer-to-peer teaching in TBL enhances learning and aids weaker learners to understand the course material (Park et al., 2014).
Some limitations of our study were that the sample size was small, reporting participants’ self-perception on how they felt after attending the workshop and the lack of longitudinal follow-up on retention of knowledge. In addition, we did not have a separate didactic lecture on the new classification as a control group to truly compare the two different modes of teaching. Future recommendation includes having two groups of GDPs to collate their perceptions as well as include a pre and post assessment to investigate the difference in improvement and in knowledge retention comparing TBL workshop and traditional didactic lecture, and include peer evaluation in TBL to increase accountability among learners. Besides, ethnographic research method can be explored to provide insight to researchers to understand the essence of how dental professionals learn during TBL. It would be meaningful to follow up this group of GDPs to assess the accuracy of their periodontal diagnoses based on the new classification to investigate the effectiveness of the TBL workshop. Of note, TBL workshops can be adapted into an online format; this is particularly useful during the current COVID-19 pandemic to engage learners and promote active learning in an online setting.
V. CONCLUSION
In conclusion, TBL pedagogy may be another mode of teaching for GDPs in continuing dental education where participants are actively engaged, and direct application of knowledge gained can be made. During this pandemic, where face-to-face sessions are minimised, educators can consider adopting TBL pedagogy on an online platform to improve learning experience and engagement of their learners.
Notes on Contributors
Dr Lean Heong Foo is a Consultant Periodontist in Department of Restorative Dentistry and Head to the Dental Surgery Assistant Certification Programme in National Dental Centre Singapore. FLH reviewed the literature, contributed to study conception, data acquisition, data analysis, drafted and critically revised the manuscript.
Dr Marianne M. A. Ong is a Senior Consultant Periodontist & Director of Education in National Dental Centre Singapore. MO contributed to study conception, data acquisition and critically revised the manuscript. All authors gave their final approval and agreed to be accountable for all aspects of the work.
Ethical Approval
This study was exempted from formal Centralised Institutional Review Broad review by SingHealth Institutional Review Board (CIRB Ref: 2021/2133).
Data Availability
Data is deposited at Figshare. https://doi.org/10.6084/m9.figshare.14411858
Acknowledgement
The authors would like to thank Ms Safiyya Mohamed Ali for providing editorial support.
Funding
There was no funding involved in the preparation of the manuscript.
Declaration of Interest
The authors declare no conflict of interest.
References
Haj-Ali, R., & Al Quran, F. (2013). Team-based learning in a preclinical removable denture prosthesis module in a United Arab Emirates dental school. Journal of Dental Education, 77(3), 351–357.
Hrynchak, P., & Batty, H. (2012). The educational theory basis of team-based learning. Medical Teacher, 34(10), 796–801.https://doi.org/10.3109/0142159X.2012.687120
Michaelsen, L. K., Parmelee, D. X., McMahon, K. K., & Levine, R. E. (2008). Team-based learning for health professions education: A guide to using small groups to improving learning. Stylus.
Park, S. E., Kim, J., & Anderson, N. K. (2014). Evaluating a team-based learning method for detecting dental caries in dental students. Journal of Curriculum and Teaching, 3(2), 100-105. https://doi.org/10.5430/jct.v3n2p100
Tonetti, M. S., Greenwell, H., & Kornman, K. S. (2018). Staging and grading of periodontitis: Framework and proposal of a new classification and case definition. Journal of Periodontology, 89(Suppl 1), S159–S172. https://doi.org/10.1002/JPER.18-0006
*Foo Lean Heong
National Dental Centre Singapore,
5, Second Hospital Avenue,
168938 Singapore
Email: foo.lean.heong@singhealth.com
Announcements
- Fourth Thematic Issue: Call for Submissions
The Asia Pacific Scholar is now calling for submissions for its Fourth Thematic Publication on “Developing a Holistic Healthcare Practitioner for a Sustainable Future”!
The Guest Editors for this Thematic Issue are A/Prof Marcus Henning and Adj A/Prof Mabel Yap. For more information on paper submissions, check out here! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Volume 9 Number 1 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors. - Volume 8 Number 3 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2021
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2021.
Refer here for the list of recipients. - Most Accessed Article 2021
The Most Accessed Article of 2021 goes to Professional identity formation-oriented mentoring technique as a method to improve self-regulated learning: A mixed-method study.
Congratulations, Assoc/Prof Matsuyama and co-authors. - Best Reviewer Awards 2020
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2020.
Refer here for the list of recipients. - Most Accessed Article 2020
The Most Accessed Article of 2020 goes to Inter-related issues that impact motivation in biomedical sciences graduate education. Congratulations, Dr Chen Zhi Xiong and co-authors.









