RESEARCH PAPER
Production of pro-inflammatory mediators stimulated by exposure of poultry house workers to airborne dust particulates
1
Central Institute for Labour Protection – National Research Institute (CIOP-PIB), Warsaw, Poland
2
Medical University, Gdańsk, Poland
Corresponding author
Rafał L. Górny
Central Institute for Labour Protection – National Research Institute (CIOP-PIB), ul. Czerniakowska 16, 00-701, Warszawa, Poland
Central Institute for Labour Protection – National Research Institute (CIOP-PIB), ul. Czerniakowska 16, 00-701, Warszawa, Poland
Ann Agric Environ Med. 2023;30(4):623-633
KEYWORDS
endotoxinsglucanssize distributionnasal lavagepoultry houseparticulate aerosolproinflammatory mediators
TOPICS
ABSTRACT
Introduction and objective:
Poultry house employees spend a significant part of their work shift being exposed to airborne particulate pollutants. The aim of this study was to assess their exposure at different stages of chicken production cycle, based on quantification of pro-inflammatory mediators (IL-1β, IL-6, IL-8, and TNFα) in nasal lavage (NAL) samples.
Material and methods:
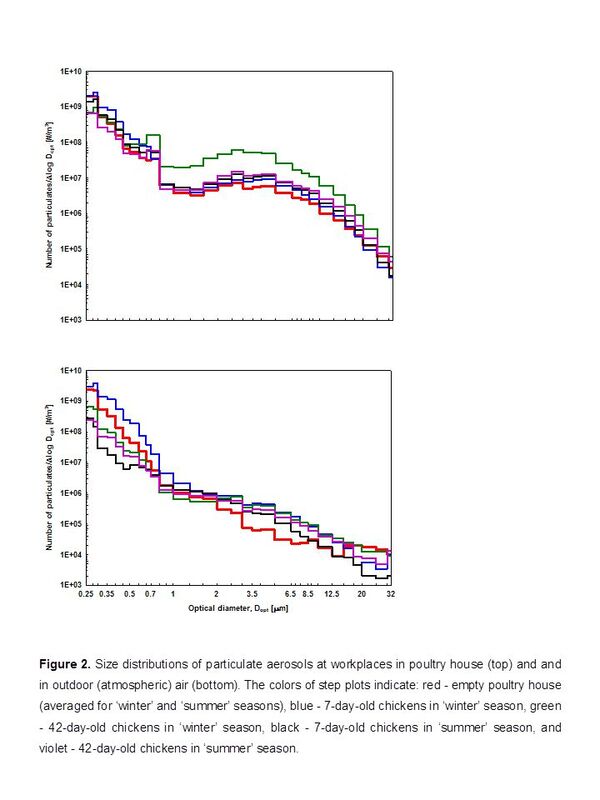
The concentrations of airborne dust at 3 different stages of the production cycle (i.e. empty poultry house, with 7- and 42-day-old chickens) were stationary measured using Grimm spectrometer, as well as CIS and Button samplers. The dust collected by the latter 2 samplers was analyzed for endotoxin and (1→3)-β-D-glucan content. NAL samples were collected from employees after their work shift to determine the pro-inflammatory mediator levels.
Results:
The maximum particulate aerosol, endotoxin, and (1→3)-β-D-glucan concentrations at workplaces reached the levels of 4.12 mg/m3, 45.21 ng/m3, and 56.54 ng/m3, respectively. The IL-1β, IL-6, and IL-8 concentrations in NAL samples ranged between 0.62–18.12 pg/mL, <0.70–25.37 pg/mL, and <3.50–259.5 pg/mL, respectively. All TNFα levels were below 4 pg/mL. There were no significant differences between these cytokine concentrations in NAL samples collected at different stages of chicken breeding in either ‘winter’ or ‘summer’ seasons.
Conclusions:
Inhalation stimulation with poultry dust containing endotoxins and (1→3)-β-D-glucans resulted in the production of pro-inflammatory mediators, which proves the course of immunological processes in the exposed employees that may lead to adverse effects. The use of nasal lavage fluid in the control of such exposure confirms that NAL analysis is a reliable laboratory tool for assessing the impact of poultry dust on exposed farm workers.
Poultry house employees spend a significant part of their work shift being exposed to airborne particulate pollutants. The aim of this study was to assess their exposure at different stages of chicken production cycle, based on quantification of pro-inflammatory mediators (IL-1β, IL-6, IL-8, and TNFα) in nasal lavage (NAL) samples.
Material and methods:
The concentrations of airborne dust at 3 different stages of the production cycle (i.e. empty poultry house, with 7- and 42-day-old chickens) were stationary measured using Grimm spectrometer, as well as CIS and Button samplers. The dust collected by the latter 2 samplers was analyzed for endotoxin and (1→3)-β-D-glucan content. NAL samples were collected from employees after their work shift to determine the pro-inflammatory mediator levels.
Results:
The maximum particulate aerosol, endotoxin, and (1→3)-β-D-glucan concentrations at workplaces reached the levels of 4.12 mg/m3, 45.21 ng/m3, and 56.54 ng/m3, respectively. The IL-1β, IL-6, and IL-8 concentrations in NAL samples ranged between 0.62–18.12 pg/mL, <0.70–25.37 pg/mL, and <3.50–259.5 pg/mL, respectively. All TNFα levels were below 4 pg/mL. There were no significant differences between these cytokine concentrations in NAL samples collected at different stages of chicken breeding in either ‘winter’ or ‘summer’ seasons.
Conclusions:
Inhalation stimulation with poultry dust containing endotoxins and (1→3)-β-D-glucans resulted in the production of pro-inflammatory mediators, which proves the course of immunological processes in the exposed employees that may lead to adverse effects. The use of nasal lavage fluid in the control of such exposure confirms that NAL analysis is a reliable laboratory tool for assessing the impact of poultry dust on exposed farm workers.
ACKNOWLEDGEMENTS
The study was funded by the National Science Centre, Kraków,
Poland (Contract No. 2019/35/B/NZ7/04394, Intensive
rearing of poultry – identification of changes occurring in
the environment and their impact on human health).
REFERENCES (122)
1.
Owczarek D. Artificial intelligence in poultry industry. What are the latest innovations in poultry farming? Nexocode 2022. https://nexocode.com/blog/post... (access: 2023.06.30).
2.
Gowda RNS. Modern innovations in poultry farming. SR Publications 2023. https://www.srpublication.com/... (access: 2023.06.30).
3.
Just N, Duchaine C, Singh B. An aerobiological perspective of dust in cage-housed and floor-housed poultry operations. J Occup Med Toxicol. 2009;4:13. https://doi.org/10.1186/1745-6....
4.
HSE – Statement of evidence: Respiratory hazards of poultry dust. Sudbury: Health and Safety Executive; 2009. www.hse.gov.uk/pubns/web40.pdf (access: 2023.06.30).
5.
May S, Romberger DJ, Poole JA. Respiratory health effects of large farming environments. J Toxicol Environ Health B Crit Rev. 2012;15(8):524-541. https://doi.org/10.1080/109374....
6.
Viegas S, Caetano LA, Korkalainen M, et al. Cytotoxic and inflammatory potential of air samples from occupational settings with exposure to organic dust. Toxics. 2017;5(1):8. https://doi.org/10.3390/toxics....
7.
Gerber PF, Gould N, McGahan E. Potential contaminants and hazards in alternative chicken bedding materials and proposed guidance levels: a review. Poult Sci. 2020;99:6664–6684. https:/doi.org/10.1016/j.psj.2020.09.047.
8.
Zuskin E, Mustajbegovic J, Schachter EN, et al. Respiratory function in poultry workers and pharmacological characterization of poultry dust extract. Environ Res. 1995;70(1):11–19. https://doi.org/10.1006/enrs.1....
9.
Castranova V, Robinson VA, Frazer DG. Pulmonary reactions to organic dust exposures: development of an animal model. Environ Health Perspect. 1996;104(Suppl. 1):41–53.
10.
Skórska C, Mackiewicz B, Golec M, et al. Health effects of exposure to organic dust in workers of a modern hatchery. Ann Agric Environ Med. 2007;14:341–345.
11.
Oppliger A, Charriere N, Droz P, et al. Exposure to bioaerosols in poultry houses at different stages of fattening; use of real-time PCR for airborne bacterial quantification. Ann Occup Hyg. 2008;52(5):405–412. https://doi.org/10.1093/annhyg....
12.
McClendon CJ, Gerald CL, Waterman JT. Farm animal models of organic dust exposure and toxicity: insights and implications for respiratory health. Curr Opin Allergy Clin Immunol. 2015;15(2):137–144. https://doi.org/10.1097/ACI.00....
13.
Hamid A, Ahmad AS, Khan N. Respiratory and other health risks among poultry-farm workers and evaluation of management practices in poultry farms. Braz J Poult Sci. 2018;20(1):111–118. https://doi.org/10.1590/1806-9....
14.
Taluja MK, Gupta V, Sharma G, et al. Respiratory hazards to occupational exposure of poultry dust in poultry farm workers in Northern India. Indian J Physiol Pharmacol. 2019;63(3):223–230.
15.
Viegas S, Faísca VM, Dias H, et al. Occupational exposure to poultry dust and effects on the respiratory system in workers. J Toxicol Environ Health, Part A. 2013;76(4-5):230–239. https://doi.org/10.1080/152873....
16.
Dos Anjos Magri C, Garófallo Garcia R, Binotto E, et al. Occupational risk factors in health of broiler-farm workers: A systematic review. Arch Environ Occup Health. 2021;76(8):482–493. https://doi.org/10.1080/193382....
17.
Brain JD. Environmental lung disease: exposures and mechanisms. Chest. 1996;109(3Suppl):74S–78S.
18.
Mack SM, Madl AK, Pinkerton KE. Respiratory health effects of exposure to ambient particulate matter and bioaerosols. Compr Physiol. 2019;10(1):1–20. https://doi.org/10.1002/cphy.c....
19.
Vaali K, Tuomela M, Mannerström M, et al. Toxic indoor air is a potential risk of causing immuno suppression and morbidity—a pilot study. J Fungi. 2022;8:104. https://doi.org/10.3390/jof802....
20.
Morakinyo OM, Mokgobu MI, Mukhola MS, et al. Health outcomes of exposure to biological and chemical components of inhalable and respirable particulate matter. Int J Environ Public Health. 2016;13:592. https://doi.org/10.3390/ijerph....
21.
Mbareche H, Morawska L, Duchaine C. On the interpretation of bioaerosol exposure measurements and impacts on health. J Air Waste Manag Assoc. 2019;69(7):789–804. https://doi.org/10.1080/109622....
22.
Roy CJ, Reed DS, Hutt JA. Aerobiology and inhalation exposure to biological select agents and toxins. Vet Pathol. 2010;47(5):779–789. https://doi.org/10.177/0300985....
23.
Steerenberg PA, Fisher PH, Gmelig-Meyling F, et al. Nasal lavage as tool for health effect assessment of photochemical air pollution. Hum Exp Toxicol. 1996;15:111–119. https://doi.org/10.1177/096032....
24.
Wang Z, Larsson K, Palmberg L, et al. Inhalation of swine dust induces cytokine release in the upper and lower airways. Eur Respir J. 1997;10:381–387. https://doi.org/10.1183/090319....
25.
Hellgren UM, Leino M, Aarnisalo AA, et al. Low tumor necrosis factor alpha levels and neutrophil counts in nasal lavage after mold exposure. Ann Allergy Asthma Immunol. 2009;102:210–215. https://doi.org/10.1016/S1081-....
26.
Górny RL, Gołofit-Szymczak M, Cyprowski M, et al. Nasal lavage as analytical tool in assessment of exposure to particulate and microbial aerosols in wood pellet production facilities. Sci Total Environ. 2019;697:134018. https://doi.org/10.1016/j.scit....
27.
Phillips VR, Holden MR, Sneath RW, et al. The development of robust methods for measuring concentrations and emission rates of gaseous and particulate air pollutants in livestock buildings. J Agric Engng Res. 1998;70(1):11–24. https://doi.org/10.1006/jaer.1....
28.
Greiff L, Pipkorn U, Alkner U, et al. The ‘nasal pool’ device applies controlled concentrations of solutes on human nasal airway mucosa and samples its surface exudations/secretions. Clin Exp Allergy. 1990;20:253–259. https://doi.org/10.1111/j.1365....
29.
Ordinance of the Minister of Family, Labor and Social Policy of June 12, 2018 on the maximum admissible concentrations and intensities for agents harmful to health in the working environment. Journal of Laws 2018, item 1286 as amended Journal of Laws 2020, item 61.
30.
Górny RL. Harmful biological agents. In: Pośniak M, Skowroń J, editors. Harmful agents in working environment – admissible values. 13th edition. Warszawa: Wydawnictwo Centralnego Instytutu Ochrony Pracy–PIB; 2022. p. 161–173.
31.
Balty I, Bertrand N, David C, et al. Valeurs guides endotoxines – interprétation des résultats de étrologie des bioaérosols. Hygiène et sécurité du travail. 2015;239:46–50.
32.
Donham KJ, Cumro D, Reynolds SJ, et al. Dose-response relationships between occupational aerosol exposures and cross-shift declines of lung function in poultry workers: Recommendations for exposure limits. J Occup Environ Med. 2000;42(3):260–269. http://www.jstor.org/stable/44....
33.
Haglind P, Rylander R. Exposure to cotton dust in an experimental cardroom. Brit J Ind Med. 1984;41(3):340–345. https://doi.org/10.1136/oem.41....
34.
Clark S. Health effects of organic dusts in the farm environment. Report on prevention and control. Am J Ind Med. 1986;10(3):267–273. https://doi.org/10.1002/ajim.4....
35.
Rylander R. The role of endotoxin for reactions after exposure to cotton dust. Am J Ind Med. 1987;12(6):687–697. https://doi.org/10.1002/ajim.4....
36.
Malmros P, Sigsgaard T, Bach B. Occupational health problems due to garbage sorting. Waste Manage Res. 1992;10(3):227–234. https://doi.org/10.1177/073424....
37.
Castellan RM, Olenchock SA, Kinsley KB, et al. Inhaled endotoxin and decreased spirometric values. An exposure-response relation for cotton dust. N Engl J Med. 1987;317(10):605–610. https://doi.org/10.1056/NEJM19....
38.
Farokhi A, Heederik D, Smit LAM. Respiratory health effects of exposure to low levels of airborne endotoxin - a systematic review. Environ Health. 2018;17(1):14. https://doi.org/10.1186/s12940....
39.
Laitinen S, Kangas J, Husman K, et al. Evaluation of exposure to airborne bacterial endotoxins and peptidoglycans in selected work environments. Ann Agric Environ Med. 2001;8(2):213–219.
40.
Palchak RB, Cohen R, Ainslie M, et al. Airborne endotoxin associated with industrial-scale production of protein products in gram-negative bacteria. Am Ind Hyg Assoc J. 1988;49(8):420–421. https://doi.org/10.1080/152986....
41.
Parker JA, Boles C, Buerger AN, et al. Derivation of an occupational exposure limit for β-glucans. Regul Toxicol Pharmacol. 2021;123:104959. https://doi.org/10.1016/j.yrtp....
42.
Ellen JJ, Bottcher RW, von Wachenfelt E, et al. Dust levels and control methods in poultry houses. J Agric Saf Health. 2000;6(4):275–282. https://doi.org/10.13031/2013.....
43.
Younis F, Salem E, Salem E. Respiratory health disorders associated with occupational exposure to bioaerosols among workers in poultry breeding farms. Environ Sci Pollut Res. 2020;27:19869–19876. https://doi.org/10.1007/s11356....
44.
Matuka DO, Ngajilo FD, Baatjies R, et al. Occupational bioaerosol exposures associated with poultry farming. J Agromed. 2023. https://doi.org/10.1080/105992....
45.
Radon K, Danuser B, Iversen M, et al. Air contaminants in different European farming environments. Ann Agric Environ Med. 2002;9:1–48.
46.
Spaan S, Wouters IM, Oosting I, et al. Exposure to inhalable dust and endotoxins in agricultural industries. J Environ Monit. 2006;8(1):63–72. https://doi.org/10.1039/b50983....
47.
Vučemilo M, Matković K, Vinković B. The effect of animal age on air pollutant concentration in a broiler house. Czech J Anim Sci. 2007;52(6):170–174. https://doi.org/10.17221/2318-....
48.
Clark S, Rylander R, Larsson L. Airborne bacteria, endotoxin and fungi in dust in poultry and swine confinement buildings. Am Ind Hyg Assoc J. 1983;44(7):537–541. https://doi.org/10.1080/152986....
49.
Olenchock SA, Lenhart SW, Mull JC. Occupational exposure to airborne endotoxins during poultry processing. J Toxicol Environ Health. 1982;9(2):339–349. https://doi.org/10.1080/152873....
50.
Jones W, Morring K, Olenchock SA, et al. Environmental study of poultry confinement buildings. Am Ind Hyg Assoc J. 1984;45(11):760–766.
51.
Yang X, Wang X, Zhang Y, et al. Monitoring total endotoxin and (1 --> 3)-beta-D-glucan at the air exhaust of concentrated animal feeding operations. J Air Waste Manag Assoc. 2013;63(10):1190–1198. https://doi.org/10.1080/109622....
52.
Jerez SB, Cheng Y, Bray J. Exposure of workers to dust and bioaerosol on a poultry farm. J Appl Poult Res. 2014;23:7–14. https://dx.doi.org/10.3382/jap....
53.
Guo L, Zhao B, Jia Y, et al. Mitigation strategies of air pollutants for mechanical ventilated livestock and poultry housing—a review. Atmosphere. 2022:13:452. https://doi.org/10.3390/atmos1....
54.
Kim Y-H, Suh H-J, Kim J-M, et al. Evaluation of environmental circumstance within swine and chicken houses in South Korea for the production of safe and hygienic animal food products. Korean J Food Sci Anim Resour. 2008;28:623–628. https://doi.org/10.5851/KOSFA.....
55.
Roque K, Shin K-M, Jo J-H, et al. Relationship between chicken cellular immunity and endotoxin levels in dust from chicken housing environments. J Vet Sci. 2015;16(2):173–177. https://dx.doi.org/10.4142/jvs....
56.
Gautam R, Heo Y, Lim G, et al. Altered immune responses in broiler chicken husbandry workers and their association with endotoxin exposure. Ind Health. 2018;56(1):10–19. https://doi.org/10.2486/indhea....
57.
Golbabaei F, Islami F. Evaluation of workers' exposure to dust, ammonia and endotoxin in poultry industries at the province of Isfahan, Iran. Ind Health. 2000;38(1):41–46. https://doi.org/10.2486/indhea....
58.
Almuhanna EA. Effect of natural and mechanical ventilation systems on air contaminants of poultry housing in Al-Ahsa (Estern Province), Saudi Arabia. J Soil Sci Agric Eng. 2011;2(3):295–314. https://doi.org/10.21608/jssae....
59.
Ławniczek-Wałczyk A, Górny RL, Golofit-Szymczak M, et al. Occupational exposure to airborne microorganisms, endotoxins and β-glucans in poultry houses at different stages of the production cycle. Ann Agric Environ Med. 2013;20(2):259–267.
60.
Lenhart SW, Morris PD, Akin RE, et al. Organic dust, endotoxin, and ammonia exposures in the North Carolina poultry processing industry. Appl Occup Environ Hyg. 1990;5:611–618. https://doi.org/10.1080/104732....
61.
Yang W, Guo M, Liu G, et al. Detection and analysis of fine particulate matter and microbial aerosol in chicken houses in Shandong Province, China. Poult Sci. 2018;97:995–1005. https://doi.org/10.3382/ps/pex....
62.
Douwes J, Thorne P, Pearce N, et al. Bioaerosol health effects and exposure assessment: progress and prospects. Ann Occup Hyg. 2003;47:187–200. https://doi.org/10.1093/annhyg....
63.
Young RS, Jones AM, Nicholls PJ. Something in the air: endotoxins and glucans as environmental troublemakers. J Pharm Pharmacol. 1998;50:11–17. https://doi.org/10.1111/j.2042....
64.
Rylander R. Endotoxin in the environment – exposure and effects. J Endotoxin Res. 2002;8(4):241–252. https://doi.org/10.1179/096805....
65.
Huneau-Salaün A, Le Bouquin S, Bex-Capelle V, et al. Endotoxin concentration in poultry houses for laying hens kept in cages or in alternative housing systems. Br Poult Sci. 2011;52(5):523–530. https://doi.org/10.1080/000716....
66.
Zock JP, Hollander A, Heederik D, et al. Acute lung function changes and low endotoxin exposures in the potato processing industry. Am J Ind Med. 1998;33(4):384–391. https://doi.org/10.1002/(sici)...<384::aid-ajim9>3.0.co;2-u.
67.
Rylander R, Carvalheiro MF. Airways inflammation among workers in poultry houses. Int Arch Occup Environ Health. 2006;79:487–490. https://doi.org/10.1007/s00420....
68.
Seedorf J, Hartung J, Schroder M, et al. Concentrations and emissions of airborne endotoxins and microorganisms in livestock buildings in Northern Europe. J Agric Eng Res. 1998;70:97–109. https://doi.org/10.1006/jaer.1....
69.
Gladding TL, Rolph CA, Gwyther CL, et al. Concentration and composition of bioaerosol emissions from intensive farms: Pig and poultry livestock. J Environ Manage. 2020;272:111052. https://doi.org/10.1016/j.jenv....
70.
Schierl R, Heise A, Egger U, et al. Endotoxin concentration in modern animal houses in Southern Bavaria. Ann Agric Environ Med. 2007;14:129–136.
71.
Kim EY, Han J, Lee Y-K, et al. Bioaerosol exposure by farm type in Korea. Ann Agric Environ Med. 2022;29(1):38–43. https://doi.org/10.26444/aaem/....
72.
Millner PD. Bioaerosols associated with animal production operations. Bioresour Technol. 2009;100(22):5379–5385. https://doi.org/10.1016/j.bior....
73.
Devlin RB, Ghio AJ, Costa DL. Responses of inflammatory cells. In: Gehr P, Heyder J, editors. Particle–lung interactions. New York: Marcel Dekker, Inc.; 2000. p. 437–472.
74.
Sigsgaard T, Bonefeld-Jørgensen EC, Kjaergaard SK, et al. Cytokine release from the nasal mucosa and whole blood after experimental exposures to organic dusts. Eur Respir J. 2000;16(1):140–145. https://doi.org/10.1034/j.1399....
75.
Douwes J, Wouters I, Dubbeld H, et al. Upper airway inflammation assessed by nasal lavage in compost workers: a relation with bio-aerosol exposure. Am J Ind Med. 2000;37:459–468. https://doi.org/10.1002/(SICI)....
76.
Douwes J. (1-->3)-Beta-D-glucans and respiratory health: a review of the scientific evidence. Indoor Air. 2005;15(3):160–169. https://doi.org/10.1111/j.1600....
77.
Sander I, Fleischer C, Borowitzki G, et al. Development of a two-site enzyme immunoassay based on monoclonal antibodies to measure airborne exposure to (1-->3)-beta-D-glucan. J Immunol Methods. 2008;337(1):55–62. https://doi.org/10.1016/j.jim.....
78.
Górny RL, Dutkiewicz J. Evaluation of microorganisms and endotoxin levels of indoor air in living rooms occupied by cigarette smokers and non-smokers in Sosnowiec, Upper Silesia, Poland. Aerobiologia. 1998;14:235–239. https://doi.org/10.1007/BF0269....
79.
Madsen AM, Schlunssen V, Olsen T, et al. Airborne fungal and bacterial components in PM1 dust from biofuel plants. Ann Occup Hyg. 2009;53(7):749–757. https://doi.org/10.1093/annhyg....
80.
Kirychuk SP, Reynolds SJ, Koehncke NK, et al. Endotoxin and dust at respirable and nonrespirable particle sizes are not consistent between cage- and floor-housed poultry operations. Ann Occup Hyg. 2010;54(7):824–832. https://doi.org/10.1093/annhyg....
81.
Madsen AM, Nielsen SH. Airborne endotoxins associated with particles of different sizes and affected by water content in handled straw. Int J Hyg Environ Health. 2010;213(4):278–284. https://doi.org/10.1016/j.ijhe....
82.
Fogelmark B, Sjöstrand M, Rylander R. Pulmonary inflammation induced by repeated inhalations of β(1,3)-D-glucan and endotoxin. Int J Exp Pathol. 1994;75(2):85–90.
83.
Fogelmark B, Thorn J, Rylander R. Inhalation of (1-->3)-beta-D-glucan causes airway eosinophilia. Mediators Inflamm. 2001;10(1):13–19. https://doi.org/10.1080/096293....
84.
Douwes J, Eduard W, Thorne PS. Bioaerosols. In: Quah SR, Cockerham W, editors. International encyclopedia of public health. 2nd edition. Volume 1. Waltham: Academic Press; 2017. p. 210–218. https://dx.doi.org/10.1016/B97....
85.
Nordgren TM, Bailey KL, Heires AJ, et al. Effects of Agricultural Organic Dusts on Human Lung-Resident Mesenchymal Stem (Stromal) Cell Function. Toxicol Sci. 2018;162(2):635–644. https://doi.org/10.1093/toxsci....
86.
Morris PD, Lenhart SW, Service WS. Respiratory symptoms and pulmonary function in chicken catchers in poultry confinement units. Am J Ind Med. 1991;19(2):195–204. https://doi.org/10.1002/ajim.4....
87.
Yasmeen R, Ali Z, Tyrrel S, et al. Assessment of respiratory problems in workers associated with intensive poultry facilities in Pakistan. Saf Health Work. 2020;11:118–124. https://doi.org/10.1016/j.shaw....
88.
Neghab M, Ebrahimi A, Soleimani E. Respiratory symptoms and lung functional impairments associated with occupational exposure to poultry house pollutants. Int J Occup Saf Ergon. 2021;27(3):867–873. https://doi.org/10.1080/108035....
89.
Sherwood RL. Biological agents. In: Cohen MD, Zelikoff JT, Schlesinger RB, editors. Pulmonary toxicology. Dordrecht: Kluwer Academic Publishers Group; 2000. p. 183–197.
90.
Quie PG. Lung defense against infection. J Pediatr. 1986;108(5 Pt 2):813–816. https://doi.org/10.1016/s0022-....
92.
Sherman JG, Peake JL, Wong VJ, et al. Air pollutants, epithelial surfaces, and lung disease. In: Foster WM, Costa DL, editors. Air pollutants and the respiratory tract. London: Informa Healthcare; 2011. p. 157–193.
93.
Roponen M, Seuri M, Nevalainen A, et al. Nasal lavage method in the monitoring of upper airway inflammation: seasonal and individual variation. Inhal Toxicol. 2003;15:649–661. https://doi.org/10.1080/089583....
94.
Stark H. Inflammatory airway responses caused by Aspergillus fumigatus and PVC challenges. (PhD Dissertation). Kuopio: University of Kuopio; 2007. http://epublications.uef.fi/pu... (access: 2023.06.30).
95.
Hoffmann H J, Iversen M, Sigsgaard T, et al. A single exposure to organic dust of non-naïve non-exposed volunteers induces long-lasting symptoms of endotoxin tolerance. Int Arch Allergy Immunol. 2005;138(2):121–126. https://doi.org/10.1159/000088....
96.
Mueller-Anneling LJ, O'Neill ME, Thorne PS. Biomonitoring for assessment of organic dust-induced lung inflammation. Eur Respir J. 2006;27:1096–1102; https://doi.org/10.1183/090319....
97.
Bønløkke JH, Veillette M, Mériaux A, et al. Work-related health effects in swine building workers after respiratory protection use. J Occup Environ Med. 2012;54(9):1126–1132. https://doi.org/10.1097/JOM.0b....
98.
Huijskens EG, Smit LA, Rossen JW, et al. Evaluation of patients with community-acquired pneumonia caused by zoonotic pathogens in an area with a high density of animal farms. Zoonoses Public Health. 2016;63(2):160–166. https://doi.org/10.1111/zph.12....
99.
Redente EF, Massengale RD. A systematic analysis of the effect of corn, wheat, and poultry dusts on interleukin-8 production by human respiratory epithelial cells. J Immunotoxicol. 2006;3(1):31–37. https://doi.org/10.1080/154769....
100.
Natarajan K, Meganathan V, Mitchell C, et al. Organic dust induces inflammatory gene expression in lung epithelial cells via ROS-dependent STAT-3 activation. Am J Physiol Lung Cell Mol Physiol. 2019;317(1):L127–L140. https://doi.org/10.1152/ajplun....
101.
Lopez-Castejon G, Brough D. Understanding the mechanism of IL-1β secretion. Cytokine Growth Factor Rev. 2011;22(4):189–195. https://doi.org/10.1016/j.cyto....
102.
Kaneko N, Kurata M, Yamamoto T, et al. The role of interleukin-1 in general pathology. Inflamm Regener. 2019;39:12. https://doi.org/10.1186/s41232....
103.
Thorne PS. Environmental endotoxin exposure and asthma. J Allergy Clin Immunol. 2021;148(1):61–63. https://doi.org/10.1016/j.jaci....
104.
Kaur G, Sethi RS. Multiple exposures to poultry barn air and lipopolysaccharide synergistically increase the pulmonary expression of TLR-4 and IL-1β. J Occup Health. 2020;62(1):e12094. https://doi.org/10.1002/1348-9....
105.
Fuster JJ, Walsh K. The good, the bad, and the ugly of interleukin-6 signaling. EMBO J. 2014;33(13):1425–1427. https://doi.org/10.15252/embj.....
106.
McLoughlin RM, Jenkins BJ, Grail D, et al. IL-6 trans-signaling via STAT3 directs T cell infiltration in acute inflammation. Proc Natl Acad Sci USA. 2005;102:9589–9594. https://doi.org/10.1073/pnas.0....
107.
Inoue KI, Sagawa T, Takano H. Role of IL-6 in severe inflammation. Am J Respir Crit Care Med. 2021;203(1):140–141. https://doi.org/10.1164/rccm.2....
108.
Larsson KA, Eklund AG, Hansson LO, et al. Swine dust causes intense airways inflammation in healthy subjects. Am J Respir Crit Care Med. 1994;150(4):973–977. doi: 10.1164/ajrccm.150.4.7921472.
109.
Larsson BM, Larsson K, Malmberg P, et al. Airway responses in naive subjects to exposure in poultry houses: comparison between cage rearing system and alternative rearing system for laying hens. Am J Ind Med. 1999;35(2):142–149. https://doi.org/10.1002/(sici)...<142::aid-ajim6>3.0.co;2-9.
110.
Von Essen S, Fryzek J, Nowakowski B, et al. Respiratory symptoms and farming practices in farmers associated with an acute febrile illness after organic dust exposure. Chest. 1999;116(5):1452–1458. https://doi.org/10.1378/chest.....
111.
Strieter RM. Interleukin-8: a very important chemokine of the human airway epithelium. Am J Physiol Lung Cell Mol Physiol. 2002;283(4):L688–689. https://doi.org/10.1152/ajplun....
112.
Gołąb J, Jakóbisiak M, Lasek M, et al. Immunologia. Wyd 7. Warszawa: Wydawnictwo Naukowe PWN; 2017.
113.
Poole JA, Wyatt TA, Von Essen SG, et al. Repeat organic dust exposure-induced monocyte inflammation is associated with protein kinase C activity. J Allergy Clin Immunol. 2007;120(2):366–373. https://doi.org/10.1016/j.jaci....
114.
Burge HA. Biological airborne pollutants. In: Foster WM, Costa DL, editors. Air pollutants and the respiratory tract. London: Informa Healthcare; 2011. p. 329–355.
115.
Von Essen S, Donham K. Illness and injury in animal confinement workers. Occup Med. 1999;14(2):337–350.
116.
Senthilselvan A, Dosman JA, Chénard L, et al. Toll-like receptor 4 variants reduce airway response in human subjects at high endotoxin levels in a swine facility. J Allergy Clin Immunol. 2009;123(5):1034-1040, 1040.e1-2. https://doi.org/10.1016/j.jaci....
117.
Delves PJ, Martin SJ, Burton DR, et al. Roitt's essential immunology. 13th edition. Oxford: Wiley-Blackwell; 2017.
118.
Albensi BC. What is nuclear factor kappa B (NF-κB) doing in and to the mitochondrion? Front Cell Dev Biol. 2019;7:154. https://doi.org/10.3389/fcell.....
119.
Brown DM, Donaldson K. Wool and grain dusts stimulate TNF secretion by alveolar macrophages in vitro. Occup Environ Med. 1996;53(6):387–393. https://doi.org/10.1136/oem.53....
120.
Wunschel J, Poole JA. Occupational agriculture organic dust exposure and its relationship to asthma and airway inflammation in adults. J Asthma. 2016;53(5):471–477. https://doi.org/10.3109/027709....
121.
Biswas SK, Lopez-Collazo E. Endotoxin tolerance: new mechanisms, molecules and clinical significance. Trends Immunol. 2009;30(10):475–487. https://doi.org/10.1016/j.it.2....
122.
López-Collazo E, del Fresno C. Pathophysiology of endotoxin tolerance: mechanisms and clinical consequences. Crit Care. 2013;17(6):242. https://doi.org/10.1186/cc1311....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.