Emotional Intelligence
INTRODUCTION
Emotional intelligence (EI) is the ability to perceive, understand, and regulate emotions in oneself and others. Introduced into formal scientific parlance in the 1990s,1 EI was popularized by the publication of Daniel Goleman’s best-selling book on the topic, entitled Emotional Intelligence: Why It Can Matter More Than IQ.2 As a construct, EI gained early traction in the field of business management, where it has been shown to predict job performance and leadership skills.2,3 EI has drawn subsequent attention from medical researchers interested in the relationships between emotion processing, medical training, and patient care.4–7
Neurosurgeons strive to deliver care that is clinically sound and emotionally responsive to the needs of their patients and families. In the process, a neurosurgeon routinely meets his or her own emotional obstacles in a professional context that is famous for its unrelenting pace, work–life imbalance, and constant intellectual rigor. In addition, the intuitive value of emotional connection must be weighed against the need for neurosurgeons to detach themselves from emotional suffering to accomplish the task at hand in the operating room. In light of this complexity, in this article we aim to introduce the general construct of EI and situate it within the scope of routine neurosurgical practice, resident training, and surgeon well-being.
WHAT IS EMOTIONAL INTELLIGENCE?
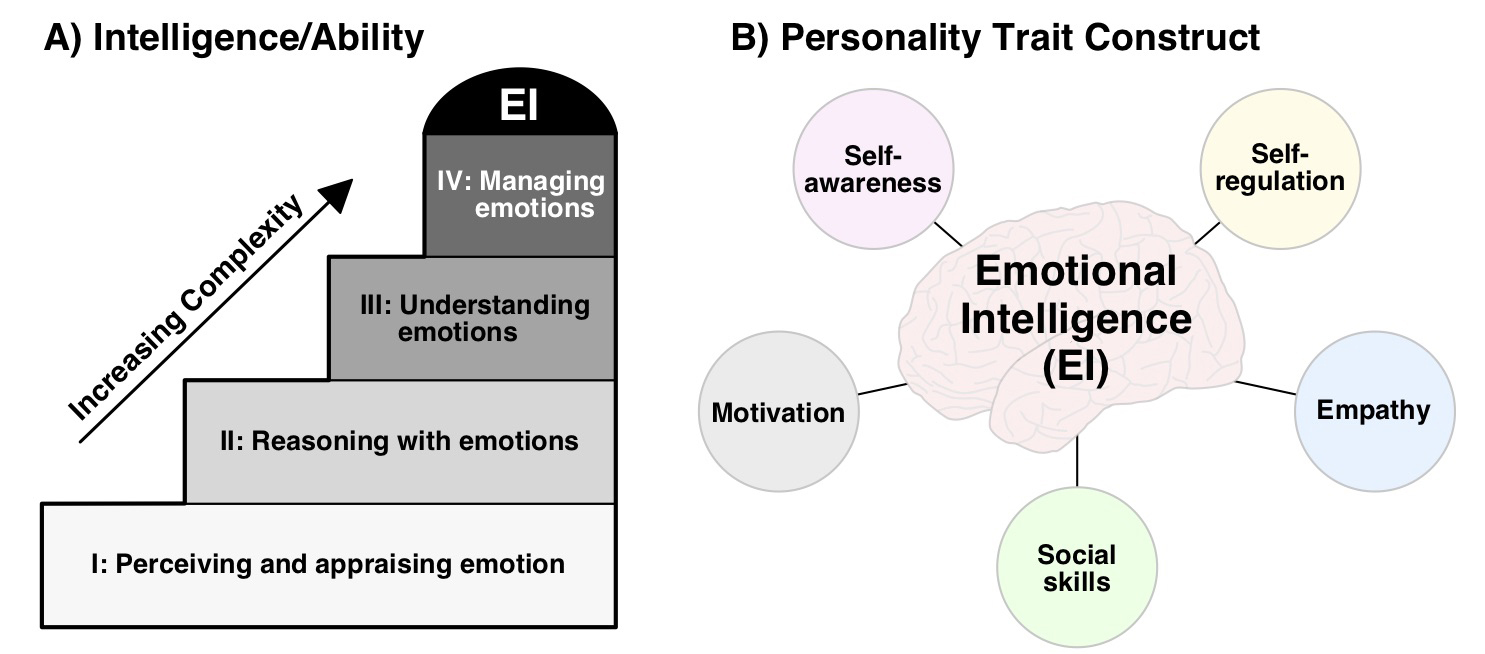
According to seminal work by Peter Salovey and John D. Mayer, both psychologists, EI is defined as an “ability to monitor one's own and others' feelings and emotions, to discriminate among them, and to use this information to guide one's thinking and actions.”8 This definition posits EI as a form of intelligence encompassing a set of interrelated abilities (or “competencies”) that can be learned and strengthened through training. According to Mayer and Salovey,9 the following 4 hierarchical branches constitute the theoretical foundation of EI (from least to most complex) (Fig 1A):
- Perceiving and appraising emotions in oneself and others
- Reasoning with emotions and using them to facilitate thinking
- Understanding emotions (including sources, fluctuations, link to behavior, etc.)
- Managing emotions to accomplish personal and interpersonal goals
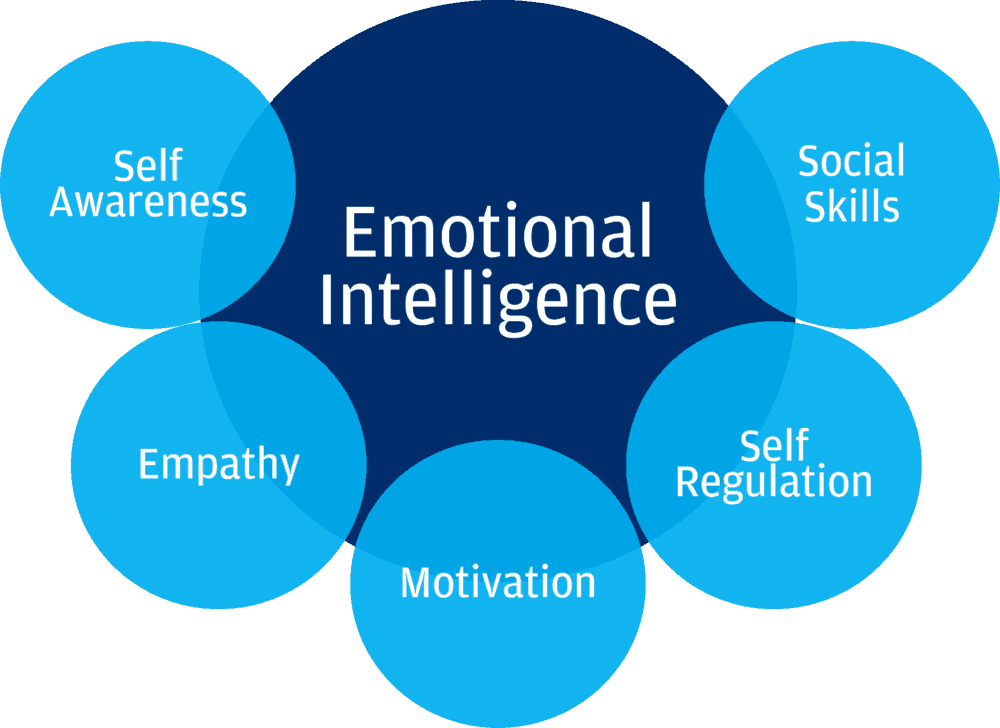
Daniel Goleman, a noted psychologist and New York Times writer, broadened this definition to include a set of personality traits and dispositions that underlie EI. His model included the following 5 core competencies10 (Fig 1B): (1) self-awareness, (2) self-regulation, (3) motivation, (4) empathy, and (5) social skills.
To frame our subsequent discussion, emotional skills, attitudes, and knowledge states that facilitate EI are presented in Table 1. Readers should note that the terms emotional intelligence (EI), emotion quotient, and emotional competence are each represented in the literature, and previous commentaries have criticized the unclear distinction between these entities, which are often used interchangeably.11
Figure 1. (A) The Mayer and Salovey 4-branch model of EI9 as a form of intelligence that encompasses a hierarchical set of 4 core abilities. (B) Five-component model of EI as a collection of personality traits.10
| Skills | |||
| Patient Directed | Self-Directed | Attitudes | Knowledge |
|
Reads facial expressions
Uses sympathetic tone
Reflects emotions back
De-escalates tension
Elicits patient concerns
Offers supportive gestures
Attends to nonverbal cues
Shares emotional observations
Makes empathic statements |
Practices positive self-talk
Recognizes self-emotion
Controls impulses
Cognitively reframes situations
Self-reflects
Self-forgives |
Open
Flexible
Nonjudgmental
Reflective
Altruistic
Accepting
Encouraging |
Recognizes sources of emotional state
Appreciates links between emotion, cognition, and behavior
Understands cultural beliefs that influence emotion
Develops strategies to identify and regulate emotional states |
*Adapted from reference 12.
EI AND MEDICINE
Compared with the literature on EI in the corporate world, relatively little has been published about the role of EI in medicine. Arora et al4 performed a systematic review of EI in the context of the 6 core Accreditation Council for Graduate Medical Education residency curriculum competencies (ie, patient care, medical knowledge, problem-based learning and improvement, interpersonal and communication skills, professionalism, and system-based practice). They examined 16 peer-reviewed articles (11 focused on residents, 4 on medical students, and 1 on medical school applicants) and found that EI was reported to correlate with improved teamwork and communication, doctor–patient relationships, empathy, and stress management. Satterfield and Hughes12 reviewed the literature on EI in undergraduate medical education and identified 5 randomized controlled trials that reported positive effects of emotional skills training on communication, empathy, and use of supportive patient-directed language.
Emerging evidence has linked EI with improved job satisfaction and well-being and decreased burnout rates among resident physicians,13–15 as well as increased patient satisfaction.16 The nascent literature exploring EI in surgical fields includes a study that documented low scores on an EI questionnaire among orthopedic surgery residents17 and a presidential address that discussed the role of EI in vascular surgery.18
EI AND NEUROSURGERY
Vignette
Dr V is a third-year neurosurgery resident starting a neuro-oncology rotation. His first appointment of the day is a follow-up visit with Mr J, a 53-year-old man who recently immigrated with his family to the area. Mr J presented to the hospital a few days ago after experiencing several weeks of progressive speech difficulty, minor headaches, and occasional memory lapses. He underwent outpatient magnetic resonance imaging (MRI) yesterday, and Dr V has just received the results.
Opening the radiology report, Dr V’s concerns are realized: “Large, heterogeneously enhancing lesion in the posterior left temporal lobe, concerning for malignant glioma.” As he prepares to discuss the results with Mr J, Dr V reflects on his own mother’s long battle with glioblastoma, having fought the disease until her death just last month. Briefly overcome by traumatic memories, Dr V takes a moment to collect his thoughts and calm his breathing.
Now composed, Dr V enters the room and greets Mr J, his wife, and his 2 school-aged sons. Dr V calls for a language interpreter to help facilitate conversation with Mr J’s wife, who speaks Spanish. Mr J sits anxiously as his wife tightly grips his hands. Mr J’s sons stand uneasily by the examination table. Dr V, feeling the weight in the room, flashes back to the day he sat with his mother as she received her diagnosis. He brings his focus back to Mr J and confirms his preference to discuss the results with his family by his side. He asks Mr J for permission to begin.
The following breakdown of the clinical vignette in reference to Goleman’s 5-component model of EI illustrates EI in neurosurgical practice:
- Self-awareness: Goleman defines self-awareness as “[k]nowing one’s emotions, strengths, weaknesses, drives, values, and goals—and their impact on others.”10 This domain encompasses the skills of emotional awareness, self-assessment, and self-confidence. Dr V enters the situation with a personal connection to this particular disease process, having experienced his own mother’s struggle with glioblastoma. These powerful emotions and memories should not be suppressed by Dr V but, rather, brought to the center of consciousness and acknowledged. Without self-awareness, Dr V could conjure the emotional trauma of his recent past and have an uncontrolled or unanticipated reaction while discussing the MRI results with Mr J. With preparation, however, Dr V can flag these emotions, anticipate feelings he might encounter, and prepare himself to be composed throughout the difficult conversation with Mr J and his family.
- Self-regulation: Self-regulation involves managing emotional responses and impulses, remaining composed, and staying focused under intense situations. In the vignette, Dr V has demonstrated several techniques for self-regulation. After the MRI report elicits traumatic memories from his mother’s battle with cancer, Dr V takes a moment to gather himself and bring his emotions under control. Dr V recognizes that Mr J and his family need a poised neurosurgeon to support them through this difficult conversation, and he regulates his own emotional state in response to that need. In the examining room, he again feels the rush of emotional memories, but by recentering his attention on the patient, he is able to stay focused and composed.
- Motivation: In reference to the self, motivation can arise from both external sources (eg, financial reward, professional advancement, etc.) and internal sources (eg, passion, life-long commitment). In this scenario, Dr V is motivated internally by his passion for medicine and his commitment to supporting patients with neurological disease. He also has the opportunity to motivate others in his surroundings, such as Mr J, to maintain his sense of agency and control over his medical care.
- Empathy. In the operating room or trauma bay, neurosurgeons need to occasionally distance themselves from the emotional circumstances at hand to function at peak performance. However, in the office setting, Dr V serves Mr J and his family by attending to the emotion in the room, noting their facial expressions and posture, and reflecting back his sympathy. Dr V has the difficult task of supporting the entire family unit through this conversation, and he must optimize the environment accordingly. For example, he confirms Mr J’s wishes to have his family present in the room (especially his children), and he ensures that a language interpreter is available to communicate most effectively with Mr J’s wife. He also asks permission to share the test results with Mr J, a simple acknowledgement of the patient’s agency that fosters trust and respect.
- Social skills: As is always the case, social savvy and interpersonal instincts are essential and likely dictate the quality of the patient–doctor relationship. Social skills refer to one’s ability to interact effectively with others and manage relationships in a manner that facilitates desired outcomes. In this scenario, Dr V aims to communicate his medical impressions and establish himself as an ally for Mr J in his forthcoming battle with disease. He therefore must be approachable, open, kind, and honest. Social nuances such as calibrating his greeting to the circumstances of the visit (eg, remaining cordial but not exuberant) contribute to the positive relationship.
EI AND LEADERSHIP
Beyond the immense knowledge base and technical skills that they must acquire, neurosurgeons need to function as an effective team leader (see Leadership Principles). EI is a fundamental skill that generalizes across a wide range of leadership positions, and neurosurgery would seem to be no exception. Having the ability to communicate effectively, inspire a team, and serve as a leader within the operating room during hours of high stress requires tremendous emotional skill. Neurosurgeons must be able to motivate colleagues around a shared vision of the treatment plan, procedural goals, and potential pitfalls.
Becoming an emotionally intelligent leader requires one to sense the mood of a colleague or group and adopt a communication style that suits that particular audience. EI is also required to navigate the everyday difficult conversations that arise between colleagues, patients, and families. As highlighted in the vignette, Dr V is the person in charge of setting the stage and creating an environment that is attentive to the emotional needs of the patient and his family. If colleagues are brought into the scenario (eg, language interpreter, member of the nursing team, etc.), Dr V assumes an interprofessional leadership role and must be able to orient the team to the emotional situation at hand.
EI AND PERSONAL COMPETENCE
Personal competence with regard to EI consists of self-awareness and self-regulation. The importance of self-awareness is familiar to most people, but the limitations of introspection and self-reflection are often overlooked. As a consequence, forming an accurate perception of one’s own mental and emotional states can be incredibly challenging. In particular, it is often difficult to recognize how our emotional state affects our behavior, and how our continuous stream of discursive thought influences our actions. Introspective techniques such as mindfulness and meditation can help overcome these “blind spots” by establishing a clear link between thoughts arising in consciousness and the emotional states that they elicit. The first step toward a more self-aware state of mind, therefore, is recognizing the connection between thoughts, emotions, and behaviors (see Situation Awareness).
Self-regulation is the second component of personal EI competence. Self-regulation offers immense benefit for neurosurgeons, especially given how emotionally draining the profession can be because of the high expectations placed on them by colleagues and patients. When practicing appropriate self-management, inner emotional conflicts are minimized and clarity in managing external situations evolves. This evolution optimizes efficiency and adaptability while promoting a more considerate approach toward one’s own emotions, which frees one’s senses and attunes them to the emotions of others. Self-regulation is also an important skill in conflict resolution and resident teaching, because losing control of one’s emotions can create an environment of distrust and contempt.
EI AND BURNOUT
Being a neurosurgeon results in an incredibly demanding lifestyle.19 Over the years, these demands can wear a person down. A 2015 study found that more than half of US physicians are experiencing professional burnout20 (for further details on burnout and how to avoid it, refer to Dealing with Burnout). Having EI is essential when demands become overwhelming, because it provides appropriate coping mechanisms. In fact, a study by Lin et al.14 found a direct correlation between EI and psychological well-being and an inverse relationship between EI and depression, emotional exhaustion, and depersonalization.
Within the framework offered by Goleman, EI can promote well-being and decrease burnout in several ways:
- Self-awareness helps the physician understand how he or she can function best.
- Self-regulation enables the physician to manage his or her own emotions under stressful conditions on the hospital floor and in the operating room.
- Motivation provides the physician an incentive to continue learning and improving despite being fatigued from the demands of the job.
- Empathy results in the compassion necessary for the physician when interacting with patients and families.
- Social skill enables the physician to accomplish his or her medical goals in a more efficient and patient-friendly manner.
CONCLUSION
We all should aim to enhance our EI. Some suggestions for attaining this goal, as Goleman outlined in his article, include the following:
- Seek constructive criticism from your colleagues
- Be cognizant of your actions and the effects they have on others
- Be a dynamic/active listener
- Be honest with yourself
Contributors: Samuel B. Tomlinson, BA, Karim Hafazalla, BS, and Benjamin Hendricks, MD
References
1. Brackett MA, Rivers SE, Salovey P. Emotional intelligence: implications for personal, social, academic, and workplace success. Soc Personal Psychol Compass 2011;5:88–103. doi.org/10.1111/j.1751-9004.2010.00334.x.
2. Goleman D. Emotional Intelligence: Why It Can Matter More Than IQ. Bloomsbury Publishing, London, England; 1995.
3. Van Rooy DL, Viswesvaran C. Emotional intelligence: a meta-analytic investigation of predictive validity and nomological net. J Vocat Behav 2004;65:71–95. doi.org/10.1016/S0001-8791(03)00076-9.
4. Arora S, Ashrafian H, Davis R, et al. Emotional intelligence in medicine: a systematic review through the context of the ACGME competencies. Med Educ 2010;44:749–764. doi.org/10.1111/j.1365-2923.2010.03709.x.
5. Grewal D, Davidson HA. Emotional intelligence and graduate medical education. JAMA 2008;300:1200–1202. doi.org/10.1001/jama.300.10.1200.
6. McKinley SK, Petrusa ER, Fiedeldey-Van Dijk C, et al. A multi-institutional study of the emotional intelligence of resident physicians. Am J Surg 2015;209:26–33. doi.org/10.1016/j.amjsurg.2014.09.015.
7. Mintz LJ, Stoller JK. A systematic review of physician leadership and emotional intelligence. J Grad Med Educ 2014;6:21–31. doi.org/10.4300/JGME-D-13-00012.1.
8. Salovey P, Mayer JD. Emotional intelligence. Imagin Cogn Pers1990;9:185–211.
9. Mayer JD, Salovey P. What is emotional intelligence? In: Salovey P, Sluyter D, eds. Emotional Development and Emotional Intelligence: Educational Implications. Basic Books, New York, NY; 1997: 3–31.
10. Goleman D. What makes a leader? Harv Bus Rev 1998;76:93–102.
11. Lewis NJ, Rees CE, Hudson JN, et al. Emotional intelligence in medical education: measuring the unmeasurable? Adv Health Sci Educ 2005;10:339–355. doi.org/10.1007/s10459-005-4861-0.
12. Satterfield JM, Hughes E. Emotion skills training for medical students: a systematic review. Med Educ 2007;41:935–941. doi.org/10.1111/j.1365-2923.2007.02835.x.
13. Hollis RH, Theiss LM, Gullick AA, et al. Emotional intelligence in surgery is associated with resident job satisfaction. J Surg Res 2017;209:178–183. doi.org/10.1016/j.jss.2016.10.015.
14. Lin DT, Liebert CA, Tran J, et al. Emotional intelligence as a predictor of resident well-being. J Am Coll Surg 2016;223:352–358. doi.org/10.1016/j.jamcollsurg.2016.04.044.
15. Lindeman B, Petrusa E, McKinley S, et al. Association of burnout with emotional intelligence and personality in surgical residents: can we predict who is most at risk? J Surg Educ 2017;74:e22–e30. doi.org/10.1016/j.jsurg.2017.11.001.
16. Weng HC, Steed JF, Yu SW, et al. The effect of surgeon empathy and emotional intelligence on patient satisfaction. Adv Health Sci Educ 2011;16:591–600. doi.org/10.1007/s10459-011-9278-3.
17. Chan K, Petrisor B, Bhandari M. Emotional intelligence in orthopedic surgery residents. Can J Surg 2014;57:89–93. doi.org/10.1503/cjs.022512.
18. Endean ED. Emotional intelligence and the vascular surgeon. J Vasc Surg 2018;68:317–324. doi.org/10.1016/j.jvs.2018.03.420.
19. Lynch G, Nieto K, Puthenveettil S, et al. Attrition rates in neurosurgery residency: analysis of 1361 consecutive residents matched from 1990 to 1999. J Neurosurg 2015;122:240–249. doi.org/10.3171/2014.10.JNS132436.
20. Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc 2015;90:1600–1613. doi.org/10.1016/j.mayocp.2015.08.023.
Please login to post a comment.