LEARNING OBJECTIVES
After reading this article you will be able to:
• understand the terms agonist, antagonist, partial agonist and inverse agonist, and how these interact with receptors
• visualise a model of dopamine receptors and be able to differentiate five subtypes
• conceptualise the dopamine hypothesis and the mechanisms of action of antipsychotics, including receptor occupancy.
Aripiprazole, brexpiprazole and cariprazine are partial agonists at dopamine (and serotonin) receptors in the brain. Used in the treatment of psychosis and depression, they have complex effects that are not easily predictable but offer both opportunities and risks for clinicians. In this article we outline the theory underlying the mechanism of action of such drugs. In our second article (Cookson Reference Cookson and Pimm2021) we will discuss their specific pharmacology and clinical use.
Receptor theory and mechanisms
Understanding the actions of partial agonists involves ‘receptor theory’, which was developed by pharmacologists in the early 20th century. Receptors are molecules on or in cells to which a drug attaches to produce its effects. The drug is said to ‘occupy’ a site on the receptor. Neurotransmitters work by attaching to their own particular type of receptor. Many drugs work by interacting with these same receptors.
A drug that activates a receptor is called an agonist and causes a response (for instance, a biochemical or electrical change in cells, contraction of smooth muscle, or secretion). Agonists act like and include the natural transmitter. Increasing concentrations of an agonist produce greater activation of receptors, up to a maximum response. This can be plotted graphically as a concentration–response curve (Fig. 1). All full agonists produce the same maximum response. (This does not mean that all the receptors are occupied by the agonist; there may be ‘spare receptors’, meaning that only a fraction needs to be occupied by an agonist to produce a full response.)

FIG 1 Sigmoidal concentration–response curves for an agonist, partial agonist and inverse agonist; a neutral antagonist produces no change in basal response. The drug concentration is plotted on a base 10 logarithmic scale (graph based on ‘Dose response curves of a full agonist, partial agonist, neutral antagonist, and inverse agonist’, Boghog, 2014; © CC BY-SA 4.0).
A competitive antagonist is a drug that attaches to the same receptor without activating it, and blocks the receptor, preventing an agonist attaching to it.
The interaction between drugs (D) and receptors (R) follows the Law of Mass action applying to chemical reactions: drug (D) and receptor (R) combine to form a drug-receptor (DR) complex and the DR complex then dissociates in the reverse reaction into D and R separately, obeying the Law of Mass Action represented thus D + R → DR and DR → D + R. An agonist and a competitive antagonist compete for binding to the receptor over a wide range of concentrations. Thus, the presence of an antagonist reduces the response produced by the agonist; this competitive interaction depends on the strength of the attraction of the antagonist to the receptor, known as the ‘affinity’. An antagonist with a high affinity will be able to block the majority of receptors at a low concentration.
A drug is described as a partial agonist if it activates the receptors but is unable to produce the same maximum response as a full agonist, however high its concentration (Fig. 1). The second important feature of a partial agonist is that, at high concentrations, it will attach to nearly all the receptors and thereby block the action of another drug which is a full agonist.
Some receptors are ‘constitutively active’; that is, they are partly activated even in the absence of the transmitter. This allows some drugs to reduce their basal activity: these are called inverse agonists (Fig. 1).
Dopamine and its receptors
Dopamine is a neurotransmitter with five identified receptor subtypes: D1-like (D1 and D5) and D2-like (D2, D3 and D4).
All the receptors are metabotropic (causing biochemical changes in cells). They are single peptides structured with seven-transmembrane domains (7TMD) arranged like a barrel with amine (NH2) and carboxyl terminals (COOH) (Fig. 2). They are G-protein coupled (GPC) receptors (GPCRs), involving second messenger systems, with different targets, including membrane channel permeability changes, intracellular signalling such as changes in cyclic adenosine monophosphate (cAMP), and affecting other enzymes.
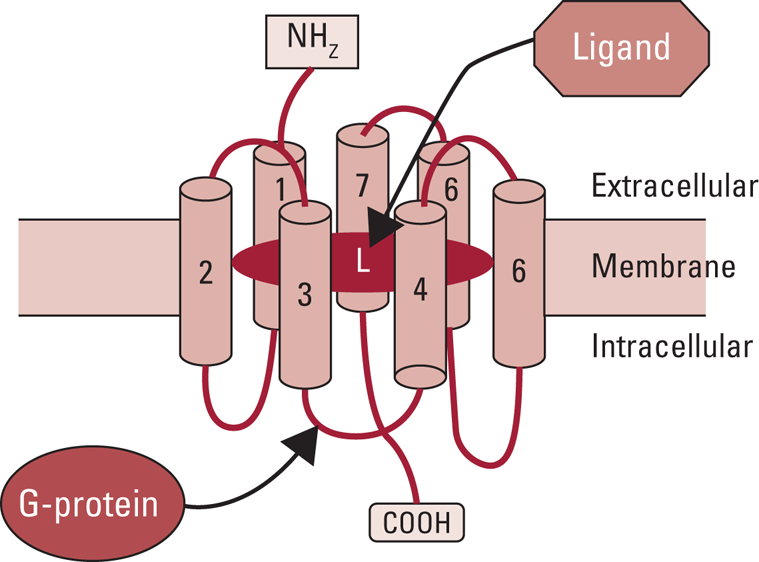
FIG 2 The seven-transmembrane domains (7TMD) architecture of the G-protein coupled dopamine receptor. L, ligand.
Dopamine binding in the extracellular side of the transmembrane ‘barrel’ causes a conformational change extending to the inner (cytoplasmic) part of the barrel, activating a guanine nucleotide exchange factor (GEF) domain and leading to the release of a G-protein (Fig. 2). The G-protein activates or inhibits adenylyl cyclase to increase cAMP (D1-like) or to decrease it (D2-like).
The receptors are subject to activation by the transmitter (dopamine) or by other ‘agonistic’ drugs (dopamine agonists) and to blockade by drugs that are antagonists of the transmitter. Most antipsychotics are regarded as reversible antagonists of dopamine receptors (‘neutral antagonists’).
The current understanding of partial agonism at GPCRs is that it arises because the drug produces a smaller conformational change in the receptor than a full agonist (Warne Reference Warne, Edwards and Dore2019). This might then produce a smaller release of G-protein.
Current antipsychotic drugs owe their efficacy to blockade of D2-like receptors. Most drugs that bind to D2 receptors bind also to D3 and D4. However, drugs have been discovered that selectively block either D3 or D4 receptors. The D3 receptors have a slightly different distribution in the brain – being richer in more ventral areas of the striatum concerned with reward – rather than D2, which are richer in the dorsal striatum and concerned with habit formation.
Characterising agonists, antagonists and partial agonists
Agonists are defined by their selectivity in eliciting a response at particular receptors, for example a D2 receptor agonist.
Antagonists are characterised by their ‘affinity’ (Ki), corresponding to their potency in occupying the receptor and blocking the response. Their affinity is measured by their ‘dissociation constant’ (Kd), the concentration at which they occupy 50% of the receptors, and this can be measured with accuracy.
Partial agonists are defined in part by their affinity (their dissociation constant) for particular receptors, but also by their ‘intrinsic activity’.
Intrinsic activity is the fraction of the maximum response the drug can achieve. This varies with different types of response (for example, in different cell types) and appears less when there are fewer receptors or no ‘spare’ receptors (Kenakin Reference Kenakin, Barrett, Page and Michel2019). It is therefore more difficult to measure.
The interactions between agonists, antagonists and partial agonists are usually competitive and reach an equilibrium that follows the law of mass action.
Combining a partial agonist with a full agonist
If a partial agonist has 20% intrinsic activity, the maximal response it can achieve (in the absence of a full agonist) is 20%.
High concentrations of a full agonist produce 100% response. When increasing concentrations of the partial agonist are added, the response is reduced, ultimately to 20% at high concentrations of the partial agonist.
The partial agonist can be described as ‘stabilising’ the stimulant action of a transmitter (agonist), whether the transmitter has a high or low concentration – in this example at 20%. This gives rise to the name ‘system stabiliser’, which is sometimes used.
In treating psychosis, the combination of a partial agonist – such as aripiprazole – with a full antagonist – such as haloperidol – is a complex situation that is beyond the scope of this paper.
Dopamine hypotheses of psychosis and receptor occupancy
Both schizophrenia and mania are hypothesised to arise from excessive activity of dopamine at specific sites in the brain, and antipsychotic/antimanic drugs improve symptoms by antagonising this excess, primarily by competitive blockade of receptors.
Dopamine and schizophrenia
Positron emission tomography (PET) scans in schizophrenia have indicated that the degree of D2-like receptor occupancy required to treat an acute relapse of schizophrenia is in the range of 70 to 80% in most cases. However, antipsychotics tend to produce Parkinsonian side-effects, which are increasingly likely with occupancy above 80% (Farde Reference Farde, Nordstrom and Wiesel1992).
As explained above, in theory a partial agonist could reduce the effect of excessive dopamine by occupying receptors but not totally blocking them at high doses. An ideal partial agonist for an acute relapse would occupy almost all receptors at the full dose, but exert an antagonistic action equivalent to only 80% antagonist occupancy; the remaining action – equivalent to almost 20% occupancy – would act like the pure agonist dopamine, thus avoiding Parkinsonism. In the example above, high doses of partial agonist result in 20% of the maximum response, whatever the concentration of the agonist (dopamine).
However, a partial agonist with higher intrinsic activity would only be able to antagonise a smaller excess of dopamine, for example where the dopamine excess requires only 65% occupancy to control the condition. This corresponds to the levels of occupancy observed in some patients in the long-term maintenance phase of schizophrenia (Ozawa Reference Ozawa, Bies and Pillai2019) and in people with a first episode (Kapur Reference Kapur, Zipursky and Jones2000).
Dopamine and mania
People with mild manic states require lower doses (for example, 1–2 mg haloperidol or risperidone, occupying 50–60% of D2 and/or D3 receptors) than those with severe mania, who may require doses up to 25 mg/day (Chou Reference Chou, Czobor and Charles1999), which are calculated to occupy more than 95% of receptors.
Dopamine and serotonin in depression
Antipsychotics are useful adjuncts to antidepressants in treating depression. The rationale is unclear, but dopamine has an important role in reward pathways and a suspected role in unipolar (Peciña Reference Peciña, Sikora and Avery2017) and bipolar depression (Belujon Reference Belujon and Grace2017). Theories of antidepressant mechanisms include D2 and/or D3 stimulation, but also serotonin mechanisms such as 5-HT1A stimulation and 5-HT2A (Gawliński Reference Gawliński, Smaga and Zaniewska2019) and 5-HT7 blockade (Yohn Reference Yohn, Gergues and Samuels2017). The partial agonists have been investigated as adjuncts or monotherapy for unipolar and bipolar depression.
Conclusions
This article introduces the mechanisms of action of aripiprazole, brexpiprazole and cariprazine, which are partial agonists at dopamine D2-like receptors and share activity as partial agonists at 5-HT1A receptors. They vary in their activities and clinical effects and this is discussed in our second article (Cookson Reference Cookson and Pimm2021).
Author contributions
J.C. drafted the text and J.P. provided advice and assistance on revisions.
Funding
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Declaration of interest
J.C. is a member of the BJPsych Advances editorial board and did not take part in the review or decision-making process for this article.
MCQs
Select the single best option for each question stem
1 D3 dopamine receptors:
a are ligand-gated ion channels
b have five transmembrane subunits
c increase the formation of cAMP
d are constitutively active
e are more common in ventral areas of the striatum.
2 Competitive antagonists:
a are selective for one particular subtype of receptor
b interact with a single neurotransmitter
c cause a parallel shift in the log–dose response curve to an agonist
d increase the effect of an inverse agonist
e prevent receptors being occupied by partial agonists.
3 Partial agonists:
a fully stimulate a proportion of receptors
b reduce the binding of full antagonists
c can occupy only a small fraction of the receptors
d occupy a subtype of the receptors that are blocked by an antagonist
e have intrinsic activity on one type of receptor.
4 The degree of D2 and D3 antagonist occupancy required for efficacy in a first episode of schizophrenia is:
a 90%
b 80%
c 70%
d 60%
e 50%.
5 If a partial agonist has 40% intrinsic activity, what occupancy is equivalent to the highest degree of antagonism it can exert?
a 20%
b 40%
c 60%
d 80%
e 100%.
MCQ answers
1 e 2 c 3 b 4 d 5 c








eLetters
No eLetters have been published for this article.