Abstract
Breast cancer is increasingly common among young women in Ghana. BCa is heterogeneous with unique traits that impact causes, prognostic, and predictive outcomes of patients before and after menopause. However, limited evidence exists on differences between young premenopausal (YPM) and postmenopausal cases in Ghana. This study compared breast tumour characteristics between YPM women (under 35 years) and postmenopausal women. We conducted a prospective cross-sectional study involving 140 BCa-diagnosed women at the Breast Care Clinic of Komfo Anokye Teaching Hospital (KATH), Kumasi from November 2019 to June 2021. Thirty-one (22.1%) of participants were YPM and 109 (77.9%) were postmenopausal. The median ages for YPM and postmenopausal were 32.0 (range: 25.0–35.0) and 57.0 (48.0–86.0) respectively. Invasive carcinoma was the most common histological type (97.1%). Left tumour location was the most frequent in both groups (51.6% for YPM and 51.8% for postmenopausal). Lumps detected were frequently in the outer upper quadrant in both groups (61.3% and 56.0%). The majority of the YPM women (80.7%) and postmenopausal women (87.0%) had stage III and IV diseases. Most YPM (64.5%) and postmenopausal women (64.4%) exhibited triple-negative breast cancer (TNBC). Both YPM 13 (56.6%) and postmenopausal participants 40 (56.3%) exhibited a predominantly partial response to neo-adjuvant chemotherapy but YPM women (21.7%) experienced disease progression than the postmenopausal women (12.7%). The study highlights consistent tumour characteristics and advanced clinical stages at diagnosis in both groups with a higher prevalence of TNBC. TNBC and HER2+ subtypes respond better to Anthracycline-based neoadjuvant chemotherapy. Establishing Breast Care Clinics in district and regional hospitals for early detection is crucial and further studies are warranted to understand the higher TNBC prevalence in black Africans and re-evaluate breast education programs to address the persistently late presentations.
Similar content being viewed by others
Introduction
Breast cancer (BCa) is the most prevalent global malignancy among women, with projections, indicating over 2 million new cases annually by 20301,2. This global trend is mirrored in sub-Saharan Africa, particularly in countries like Ghana and Nigeria, where BCa is the most frequently diagnosed cancer in females3,4. However, this surge in incidence in Sub-Saharan Africa is paralleled by poor prognosis, leading to an exponential rise in BCa mortality rates5,6. In contrast, developed countries have seen a steady decline in death rates since the 1990s due to early detection programs and improved treatment options7. A striking feature is that the majority of African women seek treatment when the disease is advanced with over 70% of cases in Ghana, Kenya, and Nigeria being diagnosed at advanced stages, often involving aggressive subtypes8,9,10.
Globally, there is an increasing incidence of BCa in younger women. These younger women exhibit distinct tumour characteristics compared to older women, such as more aggressive tumours with larger sizes, higher disease grades, positive lymph nodes, and hormone receptor negativity11,12. They also tend to have higher proportions of triple-negative breast cancer (TNBC) molecular subtype followed by human epidermal growth factor receptor 2 (HER2) which is linked with unfavourable prognoses12. Anastasiadi et al. reported young women with non-metastatic breast cancer have a higher 5-year risk of developing metastatic breast cancer when compared to their older counterparts13. The disparities in tumour characteristics between young and older women may be attributed to variations in risk factors such as race or ethnicity, body size, and reproductive history13,14. Tumour characteristics and biological markers play a crucial role in predicting outcomes in different age groups14,15.
Breast cancers in women under 35 years are classified with a category of malignancies referred to as “younger pre-menopausal women's cancers”16,17,18,19. The available literature is limited due to the scarcity of comprehensive studies and variations in the definition of "young” which may encompass ages such as 30 years, < 35 years, < 40 years, or all pre-menopausal patients. Nevertheless, the majority of studies in global literature concur that a woman under the age of 35 is generally considered “young”16,17,18,19. Findings emerging from various studies in Ghana at Komfo Anokye Teaching Hospital (KATH)20 and Korle-Bu Teaching Hospital21 as well as other regions in Ghana22, demonstrate that majority of breast cancer cases occurred in premenopausal and perimenopausal women, concomitant with advanced disease and unfavourable prognostic features.
The Breast Care Clinic at KATH registers on average 200 new cases of BCa annually. In 2019, 216 cases of tissue diagnosed BCa were recorded Breast cancer registry at KATH. Approximately, 13% of these cases affected YPM women (35 years and below), while 50% impacted women aged 49 and older23. Currently, no published study has compared tumour characteristics between these age groups in Ghana. Additionally, there is a lack of epidemiological data on BCa tumour characteristics at KATH. The study seeks to examine and assess the trend in these characteristics in the above age groups and provide valuable epidemiological information for BCa management in KATH potentially influencing treatment guidelines and enhancing outcomes in these patients.
Methodology
Study design and setting
This hospital-based prospective cross-sectional study was conducted at the Breast Care Clinic (BCC) and the Oncology Department within Komfo Anokye Teaching Hospital (KATH) from November 2019 to June 2021. KATH, the second-largest hospital in Ghana, is located in the Ashanti region, Kumasi, with a thousand-bed capacity. KATH houses skilled medical professionals including doctors, nurses, anaesthetists, and specialized departments like surgery, internal medicine, obstetrics, gynaecology, paediatrics, oncology, family medicine, and emergency care. It is strategically located, providing excellent accessibility for patients from the Ashanti Region and beyond. The BCC at KATH is discreetly positioned opposite the Human resource directorate of KATH. The BCC at KATH was established in July 2004 to take care of all patients with breast complaints. The clinic offers an autonomous daily service exclusively focused on breast diseases. The clinic days are handled by five surgical specialists. The clinic has a staff strength of ten (10): five registered nurses, two enrolled nurses, a health care assistant, and a community health nurse, led by a deputy chief nursing officer. All patients presented at the BCC undergo thorough evaluation including detailed medical history and complete clinical breast examinations. All breast lumps are assessed by a combination of clinical examination, and breast imaging (breast ultrasound and or mammography).
Study population and subject selection
The study enrolled all young pre-menopausal (YPM) women, defined as women aged 35 years and below and postmenopausal women with a histological confirmed BCa diagnosis presenting at Breast Care Clinic, KATH. The choice of the 35-year age threshold was made by harmonizing the global literature variations of different age cut-offs, such as < 30 years, < 35 years, < 40 years or all pre-menopausal used to define “young” patients with the majority considering under 35 as “young”11,17,18,19. Postmenopausal status was defined as a woman at least 48 years old with 12 consecutive months without menstruation. Patient selection was done using a convenience sampling approach and it took place in the consulting room every day of the week, starting from 8 a.m. to 2 p.m. during the study period.
Data collection and tools
Data collection involved face-to-face interviews using a structured questionnaire with women diagnosed with BCa at the BCC. The questionnaire covered demographics, BCa risk factors, breast examination findings, histological features, and staging investigations. The principal investigator and trained assistant conducted the interviews. The questionnaire was written in English but was carefully translated into the local language to ensure clarity. It was developed with information from literature and guidance from supervising consultants and pretested with 12 BCa patients at the BCC. Problems identified from the pretesting phase were corrected and the final draft was prepared for collection of data. The interviewer administered the questionnaires during the study period.
Inclusion and exclusion criteria
All women in the above age group presenting at the breast clinic with histologically proven diagnoses of breast adenocarcinoma received adriamycin and cyclophosphamide chemotherapeutic agents and consented to the study. Excluded from the study were patients with non-epithelial BCa, individuals with recurrent BCa, those prior incomplete breast mass removal, women unsuitable for chemotherapy (e.g., due to cardiac issues or early pregnancy with BCa), surgically induced menopause, cases of bilateral BCa, those undergone hysterectomy, experienced ovarian issues, lack specified menopausal status and those who decline consent.
Study sample size
In 2019, among 216 cases of breast carcinoma diagnosed in women at BCC at KATH, 28 occurred in women under 35, and 108 occurred in those aged 49 years and above. The sample size for the study was determined using the Yamane formula which is suitable when the entire population (N) is known. In this instance, the required sample size was derived from a total of 216 cases resulting in a calculated sample size of 133. To account for a 5% attrition rate and increase statistical power, the sample size was adjusted to include 140 women.
Laboratory estimation of immunohistochemistry
Specimens for histological diagnosis included core, excision, and incisional biopsies. All tissue specimens were kept in a 10% neutral buffered formalin solution within 48 h to 72 h. All biopsies were initially evaluated by routine hematoxylin and eosin-stained slides. Immunohistochemistry analysis was performed for all cases as part of routine assessment before initiation of chemotherapy. The measurement of tumour sizes before and after chemotherapy treatment was performed as part of the study. Histological grading was performed using the Scarff-Bloom-Richardson classification as modified by Elston-Ellis24. Tumors were staged according to the TNM system and regrouped using the American Joint Committee on Cancer Stages (AJCC 2010)25. Immunohistochemistry analysis for ER, PR, and HER2/neu expression was performed on the Ventana BenchMark GX autostainer. Both ER and PR were Rabbit monoclonal antibodies, ER clone SP1 and PR 1E2. The HER2 antibody used in the analysis was the Rabbit monoclonal antibody, 4B5. ER/PR positivity was defined as 1% nuclear staining following CAP/ASCO, 2020 recommendation. HER2/neu expression was categorized as per Fitzgibbons et al.’s recommendation26. Any specimen scored as 0 or 1+ was classified as HER2/neu negative, and specimens scored as 3+ were classified as positive. Cases with a score of 2+ were classified as equivocal, and reflex fluorescent in situ hybridization was used to assess the HER2/neu gene amplification. Fluorescent in situ hybridization for HER2/neu gene amplification was interpreted in compliance with ASCO/College of American Pathologists guidelines, and cases were reclassified as gene amplified or negative. Breast lump sizes were measured using a caliper and the longest diameter was recorded in centimeters. To assess tumour response to neoadjuvant chemotherapy, a follow-up measurement of any residual lump was taken a caliper (in centimeters), approximately two weeks after the completion of the fourth cycle of chemotherapy, following RECIST Criteria27.
Ethical consideration
The study was approved by the Human Research, Publication, and Ethics (CHRPE/AP/68/19) of the School of Medicine and Dentistry (SMD), Kwame Nkrumah University of Science and Technology (KNUST) and the Research and Development (R&D) unit of KATH. Prospective participants, including those with no educational background, had their legally authorized representatives or literate guardians provide informed consent for their participation. The purpose of the study was explained to all participants, and written consent was obtained. The study adhered to the core principles outlined in the Declaration of Helsinki.
Statistical analysis
Data was collected using a structured data entry form after which it was entered into Microsoft Excel software. Statistical analyses were performed on R language for statistical computing28. The principal variables analysed included immunohistochemistry (intrinsic subtypes,) and tumour characteristics (such as BCa histological type, tumor size, staging investigations, tumour location, site of lump, skin involvement, and type of skin involvement). Additionally, socio-demographic characteristics (age, marital status, educational background, occupational status, and ethnicity) were considered, along with risk factors (menarche, age at full-term pregnancy, family history of BCa, and the use of combined oral contraceptive pills). Menarche was further categorised into early (12 years and below) and late (more than 12 years). Descriptive statistics were used to examine the distribution of the study variables. Data for continuous variables between two groups were presented as means ± standard deviation (SD). Categorical variables were presented as frequencies (n) and percentages (%). Fisher’s exact test was performed to test the association of various reproductive and clinicopathological factors with pre and postmenopausal groups. A P-value of less than 0.05 was considered statistically significant.
Results
Sociodemographic characteristics of the study participants
A total of 336 patients received BCa core biopsy diagnoses between November 2019 and June 2021. Of these, 46 (13.7%) were YPM and 165 (49%) were postmenopausal and 125 (38%) were premenopausal aged 36–49 years. Fifteen YPM and 55 of the postmenopausal women did not meet inclusion criteria. Consequently, 141 eligible YPM women recruited for the study. However, the analysis included data from 140 patients, with one patient (0.07%) excluded due to inadequate data.
Table 1 shows the sociodemographic characteristics of the study participants. Among the participants, thirty-one (22.1%) were aged below 35 years, while 109 participants (77.9%) were identified in the post-menopausal phase. The majority of the participants were married (52.9%), engaged in informal occupations (62.2%) attained a basic education level (37.9%), and belonged to the Akan ethnic group. Similar trends in terms of frequencies of the results were observed between those under 35 years and postmenopausal, except for differences in educational category. While 12 (38.7%) of participants under 35 years had received tertiary education, a majority of postmenopausal participants 44 (40.4%) had completed only basic education level.
Age distribution of below 35 years and postmenopausal participants
As shown in Fig. 1, the median age of all participants was 55.0 years (range: 25.0–86.0). The median ages for those below 35 years and postmenopausal were 32.0 (range:25.0–35.0) and 57.0 (48.0–86.0) respectively. A considerable proportion of the study’s participants fell between 31 and 35 years (74.1%) among those under 35 years, while post-menopausal participants were predominantly distributed between 56 and 65 years (48.6%). A few of the participants (3.2%) within the pre-menopausal group were 25 years and below.
Association of breast-cancer-related risk factors with postmenopausal status
The majority of the under-35 participants (15, 48.4%) and postmenopausal women (46, 42.24%) experienced full-term pregnancy within 19–29 years. The absence of a family history of BCa was prevalent in both groups, with 27 (87.1%) among those under 35 and 95 (87.2%) among postmenopausal women. Similarly, no usage history of oestrogen-containing contraceptive/hormone replacement therapy was found in both groups: 27 (87.1%) and 100 (91.7%). The majority of the participants under 35 years 15 (48.4%) experienced late menarche, while a majority of post-menopausal participants 53 (48.6%) were unsure. Fisher’s exact test revealed no significant correlation between BCa-related risk factors and menopausal status (P > 0.05) (Table 2).
Association of tumour characteristics with postmenopausal women
A greater 107 (98.2%) of the post-menopausal participants had invasive carcinoma. Mean tumour size was significantly higher in those under 35 compared to postmenopausal individuals (8.76 cm ± 6.08 vs. 6.2 cm ± 3.34, P = 0.026). Both groups commonly had Left tumour locations: 51.6% (under 35) and 51.4% (post-menopausal). The upper outer quadrant was the most prevalent tumour site for both groups: 62% of those under 35 years had upper outer quadrant tumor location with 52% in the post-menopausal group. Tumour-related skin involvement was present in 45.2% of patients under 35, all displaying Peau d’orange.) Fisher’s exact test revealed no significant correlation between tumour characteristics and menopausal status (P > 0.05) (Table 3).
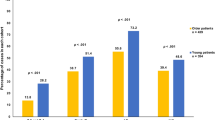
Distribution and association of clinical stage and cancer subtype with postmenopausal status
The majority of the under-35 had stage IV cancer 13 (41.9%) and for postmenopausal individuals, it was 50.4%. None of the participants under 35 had stage I BCa. TNBC subtype was the most expressed subtype 20 (64.52%) followed by HER2+ 5 (16.1%) for under-35 participants. Similarly, for post-menopausal participants, TNBC subtype was the most common subtype 70 (64.3%) followed by luminal A 19 (17.4%). There was no statistically significant association between tumour stages (P = 0.456) and tumour subtypes (P = 0.380) with postmenopausal (Fig. 2).
Distribution of RECIST response criteria among under 35-year-old and postmenopausal participants
Among those under-35, 3 (13.0%) showed complete clinical response, 13 (56.6%) had partial response, 5 (21.7%) had progressive disease and 2 (8.7%) had stable disease. Postmenopausal women exhibited predominantly partial response 40 (56.3%), with 7 (9.9%) achieved complete clinical response and 9 (12.7%) developed disease progression. Stable disease was present in 15 (21.1%) patients (Fig. 3).
Discussion
BCa accounts for around 16% of all cancer cases in Ghana and is the most common cancer among women29. Early-onset BCa may differ in etiologies, clinical features, and outcomes compared with BCa in older women. To gain further insight, we prospectively collected and compared demographic, clinico-pathological features, and outcomes of BCa in women under 35 years and those who have reached menopause at a Ghanaian teaching hospital.
The highest incidence of BCa in Ghana is typically observed between the ages of 40 to 49 years. New cases of BCa in women under 35 years at KATH constitute 13% annually as documented in the Breast Cancer Registry book of 2020. In contrast, the United States had considerably lower figures, with less than 3% for women under 35 and 7% for those under 4030. Among 336 women diagnosed with BCa during the study, 13.7% were YPM women, 49.1% were postmenopausal, and 37.2% were premenopausal. Similar patterns were observed in a study in Ghana by Clegg-Lamptey et al., showing 8% for YPM, 52% between ages 35–48 years, and 40% above 50 years21. Moreover, other regions have reported a higher proportion of BCa cases among women under 35 years, Togo, and Senegal, for instance, have reported 38.3% and 22.6%, respectively16,17. Ntekim et al. found 30.6% of BCa cases in women aged 15 to 39 years in Nigeria31 while Ntirenganya et al. also reported a proportional rate of 45.9% of BCa cases in women below 40 years in Rwanda32. The incidence of BCa in YPM women is higher in Africa as compared to other parts of the world. Hwang et al. found 4.4% of women under 35 years in South Korea33, Eiriz et al. recorded 2.5% of women under 35 in Portugal11, and Jmor et al. reported 2.0% for women under 35 in Edinburg34, The disparities may in part be explained by the population age structures and the prevalence of younger populations in African countries.
Among young premenopausal in this study, a significant portion were married, and none were divorced or widowed. Among postmenopausal, 49.5% were married, approximately half were either single or divorced, with a small fraction widowed (5%). Similar marital status distributions were reported in an Accra-based study by Iddrisu et al. for pre- and postmenopausal women with BCa in Ghana35. A study by Hinyard et al. marital status and BCa-related outcomes suggested that younger unmarried BCa women may benefit from additional counseling at the time of diagnosis36. While marriage reduces BCa and metastasis risk, it can present psychosocial challenges for young married couples37,38.
Reproductive history has been consistently associated with BCa risk39,40. Age at menarche, age at first full-term pregnancy, and nulliparity are well-established risk factors40,41,42. However, their specific impact on pre- and postmenopausal BCA risk varies across studies43. This study found that the majority of under-35 and postmenopausal women had full-term pregnancies between 19 and 29 years, and many under-35 participants had late menarche. The findings indicated there were no differences in the distribution of reproductive risk factors for BCa in both groups in this study. Both groups also had a high prevalence of no family history of BCa, consistent with reports from the literature, as most BCa patients lack a family history44. Experts caution against overemphasizing hereditary factors to avoid false security in some women45.
In this study, the commonest pathological type of BCa among YPM and postmenopausal women was invasive carcinoma at 91.67% and 98.17% respectively. These results are consistent with earlier Ghanaian studies which documented comparable findings ranging from 82 to 86%20,21,22. Moreover, these findings also mirror reports from a retrospective study by Eiriz et al.11 where in situ disease accounted for 6.45% of YPM women and 1.03% of postmenopausal women. The average tumor size at diagnosis indicated an advanced-stage disease measuring 8.76 cm (T3) for YPM women and 6.20 cm (T3) for postmenopausal women. Clegg-Lamptey et al. found an average tumour size of 6 × 7 cm in southern Ghana21 while another study in Tanzania reported an average tumour size of 6 cm46.
Most breast cancer lumps for both age groups were located in the upper outer quadrant followed by involvement in multiple quadrants. This result is consistent with reports from previous studies in Ghana20,21,22. The increased prevalence in the upper outer quadrant may be attributed to the amount of target epithelial tissue in that region, but other studies have suggested that causative factors may play a role47. The study revealed a minimal predilection for the left breast with a left breast/right breast ratio of 1.07 in both groups similar to results from the USA, Europe, and other African countries. Attributable reasons so far are inconclusive48.
Both YPM and the postmenopausal group showed concerning rates of advanced stage BCa with 80.65% and 87.1% presented at stages III and IV, respectively. The clinical stage at presentation did not differ between the two groups. Similar trends have been observed in previous studies in Ghana20,21,22 and many other sub-Saharan African countries49,50, indicating a persistent problem of late-stage diagnosis. Efforts to improve breast cancer awareness and education have not led to better early diagnosis rates. Asoogo et al. conducted a study in BCa presenting at KATH and identified key factors contributing to the late presentation including insufficient disease knowledge fear of mastectomy and cancer treatment, poverty, and destructive cultural beliefs51.
TNBC is more prominent in premenopausal African American and African women compared to women of European descent52,53. In this study, 64.5% of the YPM had TNBC while 16.3% had the HER2 + subtype. Postmenopausal women showed similar proportions 64.2% for TNBC and 11.9% for HER2 subtype and no statistical difference between the two groups. These findings concord with results from a retrospective study done by Mensal et al. in Ghana which high TNBC prevalence (66.38%) and 9.5% for the HER2+ subtype54. A comparative study by Jiagge et al. found that in patients under 50 years, TNBC was most prevalent in (50.8%) and African Americans (34.3%) compared with White Americans (16.0%) and Ethiopians (16.0%)55. Follow-up population-based studies supported the link between WA ancestry, increased TNBC rates, and more unfavourable disease outcomes55. Additionally, different studies from Nigeria (25.0%) and Kenya (20.3%) have also reported a high prevalence of TNBC56,57. Biologic and environmental factors may contribute to racial disparities in TNBC52. Tumour grade among young premenopausal women was either 48.39% for grade 2 or 51.61% for grade 3. 96.77% had no lymphovascular invasion. Among postmenopausal patients, tumour grade 2 was 55.96% and grade 3 was 36.70% and 98.17 had no lymphovascular invasion. Similar findings have been reported in different studies in sub-Saharan Africa56,58.
In this study, 13.0% of YPM women achieved complete clinical response, with 56.6% showing a partial response, but 21.7% progressed, and 8.7% remained stable. These findings are comparable to reports study by Egwuonwu et al.59, where the premenopausal response revealed 12.9% complete clinical response, 61.3% partial response, and 25.8% non-response. In postmenopausal women, 56.3% showed partial response, and 9.9% demonstrated a complete clinical response. However, 12.7% experienced disease progression and 21.1% showed stable disease. These findings highlight the aggressive nature and high progression of BCa in the younger population. Furthermore, among YPM who had either complete or partial response to anthracycline-based neoadjuvant chemotherapy, 80.95% had TNBC or HER2 subtypes, while 19.1% had luminal breast cancer For postmenopausal women with either complete clinical response or partial response, 77.42% had TNBC or HER2+ subtype and 22.6% Luminal A and B These results are consistent with reports from a study done by Carey et al. indicating that Basal-like and HER- molecular subtypes are more sensitive to anthracycline-based neoadjuvant chemotherapy than luminal breast cancers60.
The study had some limitations, including its single-centre design and small sample size. The reported numbers likely represent gross underestimate of the true prevalence of BCa among YPM and postmenopausal women in Ghana, given that a majority of patients never make it to the hospital for diagnosis. Moreover, the limited sample size undermines the suitability of robust statistical testing. The study did not evaluate loss of androgen-reception expression which has been shown to be associated with aggressive BCa in women of African descent, nor did it examine immune markers of exhaustion. Nevertheless, our findings are congruent with previous reports and highlight some significant demographic and clinical characteristics of BCa in YPM and postmenopausal women.
Conclusion
The study highlights consistent tumour characteristics in both YPM and postmenopausal women with a higher prevalence of TNBC in both groups. Advanced clinical stages at diagnosis were common. Anthracycline-based neoadjuvant chemotherapy was effective for TNBC and HER2+ subtypes. YPM women often experience more disease progression. Establishing Breast Care Clinics in district and regional hospitals for early detection is crucial. Further studies are warranted to understand the higher prevalence of TNBC in black Africans and re-evaluate breast education programs to address persistently late presentations.
Data availability
The data used to support the findings of this study will be made available upon request to the corresponding author.
References
Ferlay, J. et al. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int. J. Cancer https://doi.org/10.1002/ijc.25516 (2010).
Igene, H. Global health inequalities and breast cancer: An impending public health problem for developing countries. Breast J. https://doi.org/10.1111/j.1524-4741.2008.00618.x (2008).
Nyaaba, G. N., Stronks, K., de-Graft Aikins, A., Kengne, A. P. & Agyemang, C. Tracing Africa’s progress towards implementing the Non-Communicable Diseases Global action plan 2013–2020: A synthesis of WHO country profile reports. BMC Public Health https://doi.org/10.1186/s12889-017-4199-6 (2017).
Anyigba, C. A., Awandare, G. A. & Paemka, L. Breast cancer in sub-Saharan Africa: The current state and uncertain future. Exp. Biol. Med. https://doi.org/10.1177/15353702211006047 (2021).
Youlden, D. R. et al. The descriptive epidemiology of female breast cancer: An international comparison of screening, incidence, survival and mortality. Cancer Epidemiol. https://doi.org/10.1016/j.canep.2012.02.007 (2012).
Sharma, R. et al. Mapping cancer in Africa: A comprehensive and comparable characterization of 34 cancer types using estimates from GLOBOCAN 2020. Front. Public Health https://doi.org/10.3389/fpubh.2022.839835 (2022).
Bray, F. et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. https://doi.org/10.3322/caac.21492 (2018).
Thomas, A. S. et al. Breast cancer in Ghana: Demonstrating the need for population-based cancer registries in low-and middle-income countries. J. Glob. Oncol. https://doi.org/10.1200/JGO.2016.006098 (2017).
Azubuike, S. O. & Celestina, U. O. Breast cancer: The perspective of Northern Nigerian women. Int. J. Prev. Med. https://doi.org/10.4103/2008-7802.172803 (2015).
Makoni, M. Pilot cancer programmes in Côte d’Ivoire, Kenya, and Zimbabwe. Lancet Oncol. https://doi.org/10.1016/s1470-2045(23)00519-3 (2023).
Eiriz, I. et al. Breast cancer in young women: A multi-center 10-year experience. Ann. Oncol. https://doi.org/10.1093/annonc/mdz096.015 (2019).
Chollet-Hinton, L. et al. Breast cancer biologic and etiologic heterogeneity by young age and menopausal status in the Carolina Breast Cancer Study: A case-control study. Breast Cancer Res. https://doi.org/10.1186/s13058-016-0736-y (2016).
Anastasiadi, Z., Lianos, G. D., Ignatiadou, E., Harissis, H. V. & Mitsis, M. Breast cancer in young women: An overview. Updates Surg. https://doi.org/10.1007/s13304-017-0424-1 (2017).
Tjokrowidjaja, A., Lee, C., Houssami, N. & Lord, S. Metastatic breast cancer in young women: A population-based cohort study to describe risk and prognosis. Intern. Med. J. https://doi.org/10.1111/imj.12481 (2014).
Fredholm, H. et al. Breast cancer in young women: Poor survival despite intensive treatment. PLoS ONE 4, e7695 (2009).
Darré, T. et al. Breast cancer cases of female patients under 35 years of age in Togo: A series of 158 cases. Mol. Clin. Oncol. https://doi.org/10.3892/mco.2017.1461 (2017).
Das, U. et al. Breast cancer in women of younger than 35 years: A single center study. J. Mol. Biomark. Diagn. https://doi.org/10.4172/2155-9929.1000261 (2015).
Makanjuola, D. et al. Breast cancer in women younger than 30 years: Prevalence rate and imaging findings in a symptomatic population. Pan Afr. Med. J. https://doi.org/10.11604/pamj.2014.19.35.2849 (2014).
Gueye, M. et al. Breast cancer in women younger than 35 years: Features and outcomes in the breast unit at Aristide le Dantec Teaching Hospital, Dakar. Médecine et Santé Tropicales https://doi.org/10.1684/mst.2016.0637 (2016).
Adjei, E. Breast cancer in Kumasi, Ghana. Ghana Med. J. 46, 8–13 (2012).
Clegg-Lamptey, J. & Hodasi, W. A study of breast cancer in Korle Bu Teaching Hospital: Assessing the impact of health education. Ghana Med. J. https://doi.org/10.4314/gmj.v41i2.55305 (2007).
NakuGhartey, F. Jr., Anyanful, A., Eliason, S., Mohammed Adamu, S. & Debrah, S. Pattern of breast cancer distribution in Ghana: A survey to enhance early detection, diagnosis, and treatment. Int. J. Breast Cancer https://doi.org/10.1155/2016/3645308 (2016).
KATH. Breast Cancer Registry Notebook (Komfo Anokye Teaching Hospital, 2019).
Elston, C. W. & Ellis, I. O. Pathological prognostic factors in breast cancer. I. The value of histological grade in breast cancer: Experience from a large study with long-term follow-up. Histopathology https://doi.org/10.1111/j.1365-2559.1991.tb00229.x (1991).
Edge, S. B. & Compton, C. C. The American Joint Committee on Cancer: The 7th edition of the AJCC cancer staging manual and the future of TNM. Ann. Surg. Oncol. https://doi.org/10.1245/s10434-010-0985-4 (2010).
Allison, K. H. et al. Estrogen and progesterone receptor testing in breast cancer: ASCO/CAP guideline update. J. Clin. Oncol. https://doi.org/10.1200/jco.19.02309 (2020).
Schwartz, L. H. et al. RECIST 1.1—Update and clarification: From the RECIST committee. Eur. J. Cancer https://doi.org/10.1016/j.ejca.2016.03.081 (2016).
Cohen, Y. & Cohen, J. Y. Statistics and Data with R: An Applied Approach Through examples (Wiley, 2008).
Torre, L. A. et al. Global cancer statistics, 2012. CA Cancer J. Clin. https://doi.org/10.3322/caac.21262 (2015).
Anders, C. K., Johnson, R., Litton, J., Phillips, M. & Bleyer, A. In Seminars in Oncology. 237–249 (Elsevier).
Ntekim, A., Oluwasanu, M. & Odukoya, O. Breast cancer in adolescents and young adults less than 40 years of age in Nigeria: A retrospective analysis. Int. J. Breast Cancer https://doi.org/10.1155/2022/9943247 (2022).
Ntirenganya, F., Twagirumukiza, J. D., Bucyibaruta, G., Rugwizangoga, B. & Rulisa, S. Premenopausal breast cancer risk factors and associations with molecular subtypes: A case-control study. Int. J. Breast Cancer https://doi.org/10.1155/2021/5560559 (2021).
Hwang, T. S. et al. A comparative study of the clinical characteristics of breast cancer patients less than 35 years old and older patients. Korean J. Clin. Oncol. https://doi.org/10.14216/kjco.18001 (2018).
Jmor, S. et al. Breast cancer in women aged 35 and under: Prognosis and survival. J. R. Coll. Surg. Edinb. 47, 693–699 (2002).
Iddrisu, M., Aziato, L. & Dedey, F. A qualitative study on coping strategies of young women living with breast cancer in Ghana. Int. J. Afr. Nurs. Sci. https://doi.org/10.1016/j.ijans.2019.100173 (2019).
Hinyard, L., Wirth, L. S., Clancy, J. M. & Schwartz, T. The effect of marital status on breast cancer-related outcomes in women under 65: A SEER database analysis. Breast https://doi.org/10.1016/j.breast.2016.12.008 (2017).
Aizer, A. A. et al. Marital status and survival in patients with cancer. J. Clin. Oncol. https://doi.org/10.1200/JCO.2013.49.6489 (2013).
Baucom, D. H., Porter, L. S., Kirby, J. S., Gremore, T. M. & Keefe, F. J. Psychosocial issues confronting young women with breast cancer. Breast Dis. https://doi.org/10.3233/BD-2006-23114 (2006).
Mao, X. et al. Association of reproductive risk factors and breast cancer molecular subtypes: A systematic review and meta-analysis. BMC Cancer https://doi.org/10.1186/s12885-023-11049-0 (2023).
Lambertini, M. et al. Reproductive behaviors and risk of developing breast cancer according to tumor subtype: A systematic review and meta-analysis of epidemiological studies. Cancer Treat. Rev. https://doi.org/10.1016/j.ctrv.2016.07.006 (2016).
Khalis, M. et al. Menstrual and reproductive factors and risk of breast cancer: A case-control study in the Fez region, Morocco. PLoS ONE https://doi.org/10.1371/journal.pone.0191333 (2018).
Cancer, C. G. o. H. F. i. B. Menarche, menopause, and breast cancer risk: Individual participant meta-analysis, including 118 964 women with breast cancer from 117 epidemiological studies. Lancet Oncol. https://doi.org/10.1016/S1470-2045(12)70425-4 (2012).
Li, C. et al. Parity and risk of developing breast cancer according to tumor subtype: A systematic review and meta-analysis. Cancer Epidemiol. 75, 102050 (2021).
C. G. o. H. F. i. B. Familial breast cancer: Collaborative reanalysis of individual data from 52 epidemiological studies including 58 209 women with breast cancer and 101 986 women without the disease. Lancet 358, 1389–1399 (2001).
Admoun, C. & Mayrovitz, H. N. The etiology of breast cancer. Exon Publ. https://doi.org/10.36255/exon-publications-breast-cancer-etiology (2022).
Mremi, A. et al. Breast cancer in Tanzanian, black American, and white American women: An assessment of prognostic and predictive features, including tumor infiltrating lymphocytes. PLoS ONE https://doi.org/10.1371/journal.pone.0224760 (2019).
Darbre, P. D. Recorded quadrant incidence of female breast cancer in Great Britain suggests a disproportionate increase in the upper outer quadrant of the breast. Anticancer Res. 25, 2543–2550 (2005).
Wilting, J. & Hagedorn, M. Left-right asymmetry in embryonic development and breast cancer: Common molecular determinants?. Curr. Med. Chem. https://doi.org/10.2174/092986711798347252 (2011).
Agodirin, O. et al. Determinants of delayed presentation and advanced-stage diagnosis of breast cancer in Africa: A systematic review and meta-analysis. Asian Pac. J. Cancer Prev. https://doi.org/10.31557/APJCP.2021.22.4.1007 (2021).
Jedy-Agba, E., McCormack, V., Adebamowo, C. & dos-Santos-Silva, I. Stage at diagnosis of breast cancer in sub-Saharan Africa: A systematic review and meta-analysis. Lancet Glob. Health https://doi.org/10.1016/S2214-109X(16)30259-5 (2016).
Asoogo, C. & Duma, S. E. Factors contributing to late breast cancer presentation for health care amongst women in Kumasi, Ghana. Curationis, https://hdl.handle.net/10520/EJC177948 (2015).
Dietze, E. C., Sistrunk, C., Miranda-Carboni, G., O’regan, R. & Seewaldt, V. L. Triple-negative breast cancer in African-American women: Disparities versus biology. Nat. Rev. Cancer https://doi.org/10.1038/nrc3896 (2015).
Jiagge, E. et al. Breast cancer and African ancestry: Lessons learned at the 10-year anniversary of the Ghana-Michigan Research Partnership and International Breast Registry. J. Glob. Oncol. https://doi.org/10.1200/JGO.2015.002881 (2016).
Mensah, A. C. Survival outcomes of breast cancer in Ghana: An analysis of clinicopathological features https://doi.org/10.1245/s10434-016-5420-z (2016).
Jiagge, E. et al. Comparative analysis of breast cancer phenotypes in African American, white American, and west versus east African patients: Correlation between African ancestry and triple-negative breast cancer. Ann. Surg. Oncol. https://doi.org/10.1245/s10434-016-5420-z (2016).
Gukas, I. et al. Clinicopathological features and molecular markers of breast cancer in Jos, Nigeria. West Afr. J. Med. 24, 209–213 (2005).
Nyagol, J. et al. Routine assessment of hormonal receptor and HER-2/neu status underscores the need for more therapeutic targets in Kenyan women with breast cancer. Anal. Quant. Cytol. Histol. 28, 97–103 (2006).
Mbondel, M. P. et al. Characterisation of benign lesions and carcinomas of the female breast in a sub-Saharan African population. Pathol.-Res. Pract. https://doi.org/10.1016/S0344-0338(98)80097-6 (1998).
Egwuonwu, O. A., Anyanwu, S. N. & Nwofor, A. M. Efficacy of neoadjuvant chemotherapy in down staging locally advanced pre-menopausal breast cancer in Eastern Nigeria: Is four courses adequate?. J. Cancer Res. Ther. https://doi.org/10.4103/0973-1482.126463 (2013).
Carey, L. A. et al. The triple negative paradox: Primary tumor chemosensitivity of breast cancer subtypes. Clin. Cancer Res. https://doi.org/10.1158/1078-0432.CCR-06-1109 (2007).
Author information
Authors and Affiliations
Contributions
K.B., J.Y., T.B., S.B. and E.A. were involved in the conceptualization of the study. K.B., J.Y., M.Y., C.O. and T.B. designed the study. K.B., S.K.A., I.K., M.O.A. and D.Y. administered the project and collected data. T.B., E.A., M.N., C.O. wrote and reviewed the literature and methodology. E.A., T.B., M.N. and K.B. cleaned and analysed the data. All authors read and approved the submitted version and agree to be accountable for the accuracy of this work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bosompem, K., Yorke, J., Buckman, T.A. et al. Comparative analysis of breast cancer characteristics in young premenopausal and postmenopausal women in Ghana. Sci Rep 14, 2704 (2024). https://doi.org/10.1038/s41598-024-52129-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-52129-w
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.