Abstract
Background
Anterior Cruciate Ligament Aplasia (ACLA) is a rare condition which can sometimes remain asymptomatic into adult life. Although the quoted incidence is 1.7 per 100,000 live births, it is higher due to these silent cases and can be encountered by the arthroscopy surgeon doing reconstructive procedure for the ACL. The aim of this study is to get information on clinical presentation, imaging, arthroscopy findings and management of the knee in patients with ACL aplasia through a systematic review relevant to the arthroscopy surgeon in making a decision when they encounter such a case.
Methods
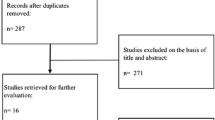
We performed a systematic review of the literature to get information on this condition that may be relevant to the arthroscopy surgeon from PubMed, Ovid full text, Embase and Ovid Medline databases. After exclusions and inclusions, we found 31 articles relevant to the search which included 101 knees.
Results
Most of the publications were case reports due to the rarity of this condition. ACLA is commonly associated with Fibular Hemimelia, Congenital Dislocation of the Knee and Proximal Focal Femoral Deficiency (PFFD). Clinical findings, imaging appearances, other associated findings with ACLA have been listed and management options listed and discussed.
Conclusions
Patients with ACLA are often asymptomatic and arthroscopic reconstruction of the ACL appears to be a viable option in selected symptomatic cases only. The arthroscopic surgeon should be aware of the clinical picture and intraarticular findings of ACLA to recognize the condition and make a decision on the optimal management. Further studies are required to report on long-term outcomes of the condition in terms of secondary osteoarthritis development as well as the procedures performed. We recommend forming a global registry to study and further understand the aspects of this condition.
Level of Evidence
4




Similar content being viewed by others
Availability of Data and Materials
The data sets during and/or analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
- AC:
-
Articular cartilage
- ACLA:
-
Anterior cruciate ligament aplasia
- ACLR:
-
Anterior cruciate ligament reconstruction
- AL:
-
Anterolateral
- BPTB:
-
Bone patellar tendon bone
- CKD:
-
Congenital knee dislocation
- CORA:
-
Centre of angulation of rotation
- FH:
-
Fibular hemimelia
- ICN:
-
Intercondylar notch
- LCL:
-
Lateral collateral ligament
- LFC:
-
Lateral femoral condyle
- LLD:
-
Limb length discrepancy
- LM:
-
Lateral meniscus
- MFC:
-
Medial femoral condyle
- MFL:
-
Menisco femoral ligament
- MM:
-
Medial meniscus
- MPFL:
-
Medial patello femoral ligament
- PCLA:
-
Posterior cruciate ligament aplasia
- PCLR:
-
Posterior cruciate ligament reconstruction
- PFFD:
-
Proximal focal femoral deficiency
- PFJ:
-
Patello-femoral joint
- PLC:
-
Postero lateral corner
- STG:
-
Semitendinosis gracilis
References
Johannson, E., & Aparisi, T. (1982). Congenital absence of the cruciate ligaments. A case report and review of the literature. Clinical Orthopaedics and Related Research, 162, 108–111.
Manner, H., Radler, C., Ganger, R., & Grill, F. (2006). Dysplasia of the cruciate ligaments: Radiographic assessment and classification. Journal of Bone and Joint Surgery. American Volume, 88(1), 130–137. https://doi.org/10.2106/JBJS.E.00146
Berruto, M., Gala, L., Usellini, E., Duci, D., & Marelli, B. (2012). Congenital absence of the cruciate ligaments. Knee Surgery, Sports Traumatology, Arthroscopy, 20(8), 1622–1625. https://doi.org/10.1007/s00167-011-1816-2
Critical-appraisal-tools—Critical Appraisal Tools | Joanna Briggs Institute. Retrieved from https://jbi.global/critical-appraisal-tools. 23 June 2021.
Thomas, N. P., Jackson, A. M., & Aichroth, P. M. (1985). Congenital absence of the anterior cruciate ligament. A common component of knee dysplasia. Journal of Bone and Joint Surgery. British Volume, 67(4), 572–575. https://doi.org/10.1302/0301-620X.67B4.4030852
Kaelin, A., Hulin, P. H., & Carlioz, H. (1986). Congenital aplasia of the cruciate ligaments. A report of six cases. Journal of Bone and Joint Surgery, 68(5), 827–828. https://doi.org/10.1302/0301-620X.68B5.3782255
Roux, M., & Carlioz, H. (1999). Clinical examination and investigation of the cruciate ligaments in children with fibular hemimelia. Journal of Pediatric Orthopedics, 19(2), 247–251. https://doi.org/10.1097/00004694-199903000-0002
Gabos, P. G., El Rassi, G., & Pahys, J. (2005). Knee reconstruction in syndromes with congenital absence of the anterior cruciate ligament. Journal of Pediatric Orthopedics, 25(2), 210–214. https://doi.org/10.1097/01.bpo.0000153874.74819.29
Chomiak, J., Podskubka, A., Dungl, P., Ost’Adal, M., & Frydrychova, M. (2012). Cruciate ligaments in proximal femoral focal deficiency: Arthroscopic assessment. Journal of Pediatric Orthopaedics, 32(1), 21–28. https://doi.org/10.1097/BPO.0b013e31823d34db
Sachleben, B., Nasreddine, A., Nepple, J., et al. (2019). Reconstruction of symptomatic congenital anterior cruciate ligament insufficiency. Journal of Pediatric Orthopedics, 39(2), 59–64. https://doi.org/10.1097/BPO.0000000000000940
Andersson, A. P., & Ellitsgaard, N. (1992). Aplasia of the anterior cruciate ligament with a compensating posterior cruciate ligament. Acta Orthopaedica Belgica, 58(2), 240–242.
Balke, M., Mueller-Huebenthal, J., Shafizadeh, S., Liem, D., & Hoeher, J. (2010). Unilateral aplasia of both cruciate ligaments. Journal of Orthopaedic Surgery and Research, 5(1), 11. https://doi.org/10.1186/1749-799X-5-11
Benassi, A. B., Guerreiro, J. P. F., de Oliveira Queiroz, A., Gasparelli, R. G., & Danieli, M. V. (2018). Anterior and posterior cruciate ligament agenesis. Journal of Surgical Case Reports. https://doi.org/10.1093/jscr/rjy216
Chahla, J., Pascual-Garrido, C., & Rodeo, S. A. (2015). Ligament reconstruction in congenital absence of the anterior cruciate ligament: A report of two cases. HSS Journal, 11(2), 177–181. https://doi.org/10.1007/s11420-015-9448-6
Davanzo, D., Fornaciari, P., Barbier, G., Maniglio, M., & Petek, D. (2017). Review and long-term outcomes of cruciate ligament reconstruction versus conservative treatment in siblings with congenital anterior cruciate ligament aplasia. Case Reports in Orthopedics, 2017, 1636578.
De Ponti, A., Sansone, V., & de Gama, M. M. (2001). Bilateral absence of the anterior cruciate ligament. Arthroscopy, 17(6), E26. https://doi.org/10.1053/jars.2001.22411
Degnan, A. J., Kietz, D. A., Grudziak, J. S., & Shah, A. (2018). Bilateral absence of the cruciate ligaments with meniscal dysplasia: Unexpected diagnosis in a child with juvenile idiopathic arthritis. Clinical Imaging, 49, 193–197. https://doi.org/10.1016/j.clinimag.2018.03.015
Figueroa, D., Calvo, R., Villalón, I. E., Schmidt-Hebbel, A., Figueroa, F., & Baar, A. (2012). Single time angular deformity correction and treatment of knee instability in congenital fibular hemimelia. A case report. The Knee, 19(4), 504–507. https://doi.org/10.1016/j.knee.2011.07.009
Hejgaard, N., & Kjaerulff, H. (1987). Congenital aplasia of the anterior cruciate ligament. Report of a case in a seven-year-old girl. International Orthopaedics, 11(3), 223–225. https://doi.org/10.1007/BF00271452
Kambhampati, S. B. (2019). Bucket handle horizontal cleavage tear of medial meniscus with congenital deformity—A case report. Journal of Arthroscopy and Joint Surgery, 6(3), 146–148. https://doi.org/10.1016/j.jajs.2019.05.005
Kaplan, D., Jazrawi, T., Capo, J., & Strauss, E. (2017). multiple ligament reconstruction for absent cruciate and a congenital short femur case report and review of the literature. Bulletin of the Hospital for Joint Disease, 75(2), 143–147.
Kwan, K., & Ross, K. (2009). Arthrogryposis and congenital absence of the anterior cruciate ligament: A case report. The Knee, 16(1), 81–82. https://doi.org/10.1016/j.knee.2008.08.004
Lee, J. J., Oh, W. T., Shin, K. Y., Ko, M. S., & Choi, C. H. (2011). Ligament reconstruction in congenital absence of the anterior cruciate ligament: A case report. Knee Surgery & Related Research, 23(4), 240–243. https://doi.org/10.5792/ksrr.2011.23.4.240
Lu, R., Zhu, D. P., Chen, N., Sun, H., Li, Z. H., & Cao, X. W. (2019). How should congenital absence of cruciate ligaments be treated? A case report and literature review. World Journal of Clinical Cases, 7(19), 3082–3089. https://doi.org/10.12998/wjcc.v7.i19.3082
Mascarenhas, R., Simon, D., Forsythe, B., & Harner, C. D. (2014). ACL reconstruction in a teenage athlete with fibular hemimelia. The Knee, 21(2), 613–616. https://doi.org/10.1016/j.knee.2013.10.011
Murali, J., Monchik, K., & Fadale, P. (2015). congenital absence of the anterior cruciate ligament. American Journal of Orthopedics, 44(8), E283–E285.
Park, I.-S., & Kim, S.-J. (2013). Agenesis of the posterolateral bundle of anterior cruciate ligament. Knee Surgery, Sports Traumatology, Arthroscopy, 21(3), 596–598. https://doi.org/10.1007/s00167-012-1962-1
Patwardhan, S., Sodhai, V., Sancheti, P., & Shyam, A. (2020). Extra-articular tenodesis using autogenous iliotibial band for symptomatic congenital absence of anterior cruciate ligament: A report of 2 cases. JBJS Case Connector, 10(2), e0240. https://doi.org/10.2106/JBJS.CC.19.00240
Rayar, M., Bouillis, J., Fraisse, B., Marleix, S., Chapuis, M., & Violas, P. (2011). Discoid meniscus associated with agenesis of the anterior cruciate ligament in an 8-year-old child. Orthopaedics & Traumatology, Surgery & Research, 97(8), 874–876. https://doi.org/10.1016/j.otsr.2011.04.011
Razi, M., Mazoochy, H., Ziabari, E. Z., Dadgostar, H., Askari, A., & Arasteh, P. (2020). Anterolateral meniscofemoral ligament associated with ring-shaped lateral meniscus and congenital absence of anterior cruciate ligament, managed with ligament reconstruction. Archives of Bone and Joint Surgery, 8(1), 112–116. https://doi.org/10.22038/abjs.2019.14128
Silva, A., & Sampaio, R. (2011). Anterior lateral meniscofemoral ligament with congenital absence of the ACL. Knee Surgery, Sports Traumatology, Arthroscopy, 19(2), 192–195. https://doi.org/10.1007/s00167-010-1199-9
Sonn, K. A., & Caltoum, C. B. (2014). Congenital absence of the anterior cruciate ligament in monozygotic twins. International Journal of Sports Medicine, 35(13), 1130–1133. https://doi.org/10.1055/s-0034-1370923
Katz, M. P., Grogono, B. J., & Soper, K. C. (1967). The etiology and treatment of congenital dislocation of the knee. Journal of Bone and Joint Surgery. British Volume, 49(1), 112–120. https://doi.org/10.1302/0301-620X.49B1.112
Bedoya, M. A., McGraw, M. H., Wells, L., & Jaramillo, D. (2014). Bilateral agenesis of the anterior cruciate ligament: MRI evaluation. Pediatric Radiology, 44(9), 1179–1183. https://doi.org/10.1007/s00247-014-2947-7
Dejour, H., Neyret, P., Eberhard, P., & Walch, G. (1990). Bilateral congenital absence of the anterior cruciate ligament and the internal menisci of the knee. A case report. Revue de Chirurgie Orthopédique et Réparatrice de l’Appareil Moteur, 76(5), 329–332.
Knorr, J., Accadbled, F., Cassard, X., Ayel, J. E., & Sales de Gauzy, J. (2006). Isolated congenital aplasia of the anterior cruciate ligament treated by reconstruction in a 5-year-old boy. Revue de Chirurgie Orthopédique et Réparatrice de l’Appareil Moteur, 92(8), 803–808. https://doi.org/10.1016/s0035-1040(06)75949-9
Steckel, H., Klinger, H. M., Baums, M. H., & Schultz, W. (2005). Cruciate ligament reconstruction in knees with congenital cruciate ligament aplasia. Sportverletzung-Sportschaden, 19(3), 130–133. https://doi.org/10.1055/s-2005-858474
Tolo, V. T. (1981). Congenital absence of the menisci and cruciate ligaments of the knee. A case report. Journal of Bone & Joint Surgery, 63(6), 1022–1024.
Crawford, D., Tompkins, B., Baird, G., & Caskey, P. (2012). The long-term function of the knee in patients with fibular hemimelia and anterior cruciate ligament deficiency. The Journal of Bone and Joint Surgery. British Volume, 94-B(3), 328–333. https://doi.org/10.1302/0301-620X.94B3.27997
Walker, J., Milbrandt, T., Iwinski, H., & Talwalkar, V. (2019). Classification of cruciate ligament dysplasia and the severity of congenital fibular deficiency. Journal of Pediatric Orthopaedics, 39(3), 136–140. https://doi.org/10.1097/BPO.0000000000000910
Giorgi, B. (1956). Morphologic variations of the intercondylar eminence of the knee. Clinical Orthopaedics, 8, 209–217.
Hamdy, R., Makhdom, A., et al. (2014). Congenital fibular deficiency. Journal of the American Academy of Orthopaedic Surgeons, 22(4), 246–255. https://doi.org/10.5435/JAAOS-22-04-246
Cuervo, M., Albiñana, J., Cebrian, J., & Juarez, C. (1996). Congenital hypoplasia of the fibula: Clinical manifestations. Journal of Pediatric Orthopedics. Part B, 5(1), 35–38.
Paley, D., & Standard, S. C. (2010). Treatment of congenital femoral deficiency. In S. W. Wiesel (Ed.), Operative techniques in orthopaedic surgery (pp. 1202–1223). Philadelphia: Lippincott Williams & Wilkins.
Mindler, G. T., Radler, C., & Ganger, R. (2016). The unstable knee in congenital limb deficiency. Journal of Children’s Orthopaedics, 10(6), 521–528. https://doi.org/10.1007/s11832-016-0784-y
World Population Prospects-Population Division-United Nations. Retrieved from https://population.un.org/wpp/Graphs/DemographicProfiles/Line/900. 2 Sept 2021.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
SBSK: conceptualized, designed the study, searched the literature, data collection, Risk of bias assessments, data analysis, derivation of results, manuscript writing, revising and final approval. KV: data collection, risk of bias assessments, data analysis, derivation of results, manuscript writing, revising, final approval. NV: data collection, data analysis, manuscript writing, final approval. APSK: data analysis, manuscript writing, final approval. BA: data analysis, manuscript writing, final approval. DM: data analysis, derivation of results, manuscript writing, revising, final approval.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no competing interests.
Ethics Approval
Not applicable. As this is a literature search study, ethics committee approval was deemed not required.
Consent to Participate
Not applicable. As this is a literature search study, ethics committee approval was deemed not required.
Consent for Publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kambhampati, S.B.S., Vishwanathan, K., Vasudeva, N. et al. Management of Anterior Cruciate Ligament Aplasia for the Arthroscopy Surgeons: A Systematic Review. JOIO 56, 1123–1138 (2022). https://doi.org/10.1007/s43465-022-00651-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43465-022-00651-2