Abstract
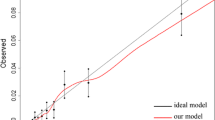
Small bowel obstruction (SBO) is one of the most frequent causes of general emergency surgery. The 30-day mortality rate post-surgery ranges widely from 2 to 30%, contingent upon the patient population, which renders risk assessment tools helpful. this study aimed to develop a 30-day point-scoring risk calculator designed for patients undergoing SBO surgery. Patients who underwent SBO surgery were identified in the ACS-NSQIP database from 2005 to 2021. Patients were randomly sampled into an experimental (2/3) and a validation (1/3) group. A weighted point scoring system was developed for the risk of 30-day mortality, utilizing multivariable regression on preoperative risk variables based on Sullivan’s method. The risk scores underwent both internal and external validation. Furthermore, the efficacy of the risk score was evaluated in 30-day major surgical complications. A total of 93,517 patients were identified, with 63,521 and 29,996 assigned to the experimental and validation groups, respectively. The risk calculator is structured to assign points based on age (> 85 years, 4 points; 75–85 years, 3 points; 65–75 years, 2 points; 55–65 years, 1 point), disseminated cancer (2 points), American Society of Anesthesiology (ASA) score of 4 or 5 (1 point), preoperative sepsis (1 point), hypoalbuminemia (1 point), and fully dependent functional status (1 point). The risk calculator showed strong discrimination (c-statistic = 0.825, 95% CI 0.818–0.831) and good calibration (Brier score = 0.043) in the experimental group. The point scoring system was successfully translated from individual preoperative variables (c-statistic = 0.840, 95% CI 0.834–0.847) and was externally validated in ACS-NSQIP (c-statistic = 0.827, 95% = CI 0.834–0.847, Brier score = 0.043). The SBO risk score can effectively discriminate major surgical complications including major adverse cardiovascular events (c-statistic = 0.734), cardiac complications (c-statistic = 0.732), stroke (c-statistic = 0.725), pulmonary complications (c-statistic = 0.727), renal complications (c-statistic = 0.692), bleeding (c-statistic 0.674), sepsis (c-statistic = 0.670), with high predictive accuracy (all Brier scores < 0.1). This study developed and validated a concise yet robust 10-point risk scoring system for patients undergoing SBO surgery. It can be informative to determine treatment plans and to prepare for potential perioperative complications in patients undergoing SBO surgery.


Similar content being viewed by others
Data availability
Not applicable.
References
Springer JE, Bailey JG, Davis PJB, Johnson PM (2014) Management and outcomes of small bowel obstruction in older adult patients: a prospective cohort study. Can J Surg 57:379–384. https://doi.org/10.1503/cjs.029513
Ozturk E, van Iersel M, Stommel MM et al (2018) Small bowel obstruction in the elderly: a plea for comprehensive acute geriatric care. World J Emerg Surg 13:48. https://doi.org/10.1186/s13017-018-0208-z
Jeppesen MH, Tolstrup M-B, Kehlet Watt S, Gögenur I (2016) Risk factors affecting morbidity and mortality following emergency laparotomy for small bowel obstruction: a retrospective cohort study. Int J Surg 28:63–68. https://doi.org/10.1016/j.ijsu.2016.02.059
Paul CJJ, Dohmen J, van Beekum CJ et al (2022) Surgical treatment of mechanical bowel obstruction: characteristics and outcomes of geriatric patients compared to a younger cohort. Int J Colorectal Dis 37:1281–1288. https://doi.org/10.1007/s00384-022-04152-4
Paulson EK, Thompson WM (2015) Review of small-bowel obstruction: the diagnosis and when to worry. Radiology 275:332–342. https://doi.org/10.1148/radiol.15131519
Margenthaler JA, Longo WE, Virgo KS et al (2006) Risk factors for adverse outcomes following surgery for small bowel obstruction. Ann Surg 243:456–464. https://doi.org/10.1097/01.sla.0000205668.58519.76
Bilimoria KY, Liu Y, Paruch JL et al (2013) Development and evaluation of the universal ACS NSQIP surgical risk calculator: a decision aid and informed consent tool for patients and surgeons. J Am Coll Surg 217:833. https://doi.org/10.1016/j.jamcollsurg.2013.07.385
Sullivan LM, Massaro JM, D’Agostino RB (2004) Presentation of multivariate data for clinical use: the Framingham Study risk score functions. Stat Med 23:1631–1660. https://doi.org/10.1002/sim.1742
van Walraven C, Austin PC, Jennings A et al (2009) A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care 47:626–633. https://doi.org/10.1097/MLR.0b013e31819432e5
DeLong ER, DeLong DM, Clarke-Pearson DL (1988) Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 44:837–845
Alba AC, Agoritsas T, Walsh M et al (2017) Discrimination and calibration of clinical prediction models: users’ guides to the medical literature. JAMA 318:1377–1384. https://doi.org/10.1001/jama.2017.12126
Bae S, Massie AB, Caffo BS et al (2020) Machine learning to predict transplant outcomes: helpful or hype? Transpl Int 33:1472–1480. https://doi.org/10.1111/tri.13695
Hackett NJ, De Oliveira GS, Jain UK, Kim JYS (2015) ASA class is a reliable independent predictor of medical complications and mortality following surgery. Int J Surg 18:184–190. https://doi.org/10.1016/j.ijsu.2015.04.079
Scarborough JE, Bennett KM, Englum BR et al (2015) The impact of functional dependency on outcomes after complex general and vascular surgery. Ann Surg 261:432–437. https://doi.org/10.1097/SLA.0000000000000767
Bateni SB, Meyers FJ, Bold RJ, Robert JC (2015) Current perioperative outcomes for patients with disseminated cancer. J Surg Res 197:118–125. https://doi.org/10.1016/j.jss.2015.03.063
Mullen MG, Michaels AD, Mehaffey JH et al (2017) Risk associated with complications and mortality after urgent surgery vs elective and emergency surgery: implications for defining “quality” and reporting outcomes for urgent surgery. JAMA Surg 152:768–774. https://doi.org/10.1001/jamasurg.2017.0918
Gibbs J, Cull W, Henderson W et al (1999) Preoperative serum albumin level as a predictor of operative mortality and morbidity: results from the national VA surgical risk study. Arch Surg 134:36–42. https://doi.org/10.1001/archsurg.134.1.36
Larsen PB, Liest S, Hannani D et al (2021) Preoperative hypoalbuminemia predicts early mortality following open abdominal surgery in patients above 60 years of age. Scand J Surg 110:29–36. https://doi.org/10.1177/1457496919888598
Hwang F, Crandall M, Smith A et al (2023) Small bowel obstruction in older patients: challenges in surgical management. Surg Endosc 37:638–644. https://doi.org/10.1007/s00464-022-09428-y
Almafreji I, Chinaka U, Hussain A et al (2020) Role of gastrografin in patients with small bowel obstruction. Cureus 12:e9695. https://doi.org/10.7759/cureus.9695
Acknowledgements
The authors acknowledge Dr. Richard Amdur, PhD, for giving statistical support for this project.
Funding
This research did not receive any funding from any agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Ethical approval
This study was exempt from the IRB approval by the George Washington University as it analyzed retrospective, deidentified ACS-NSQIP data.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, R. Development and validation of a 30-day point-scoring risk calculator for small bowel obstruction surgery. Updates Surg (2024). https://doi.org/10.1007/s13304-024-01875-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13304-024-01875-7