Abstract
Background
Small bowel obstruction (SBO) is a common disease affecting all segments of the population, including the frail elderly. Recent retrospective data suggest that earlier operative intervention may decrease morbidity. However, management decisions are influenced by surgical outcomes. Our goal was to determine the current surgical management of SBO in older patients with particular attention to frailty and the timing of surgery.
Study design
A retrospective review of patients over the age of 65 with a diagnosis of bowel obstruction (ICD-10 K56*) using the 2016 National Inpatient Sample (NIS). Demographics included age, race, insurance status, medical comorbidities, and median household income by zip code. Elixhauser comorbidities were used to derive a previously published frailty score using the NIS dataset. Outcomes included time to operation, mortality, discharge disposition, and hospital length of stay. Associations between demographics, frailty, timing of surgery, and outcomes were determined.
Results
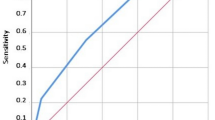
264,670 patients were included. Nine percent of the cohort was frail; overall mortality was 5.7%. Frail had 1.82 increased odds of mortality (95% CI 1.64–2.03). Hospital LOS was 1.6 times as long for frail patients; a quarter of the frail were discharged home. Frail patients waited longer for surgery (3.58 days vs 2.44 days; p < 0.001). Patients transferred from another facility had increased mortality (aOR 1.58; 95% CI 1.36–1.83). There was an increasing mortality associated with a delay in surgery.
Conclusion
Patients with frailty and SBO have higher mortality, more frequent discharge to dependent living, longer hospital length of stay, and longer wait to operative intervention. Mortality is also associated with male gender, black race, transfer status from another facility, self-pay status, and low household income. Every day in delay in surgical intervention for those who underwent operations led to higher mortality. If meeting operative indications, older patients with bowel obstruction have a higher chance of survival if they undergo surgery earlier.

Similar content being viewed by others
References
Taylor MR, Lalani N (2013) Adult small bowel obstruction. Acad Emerg Med 20(6):528–544
Irvine TT (1989) Abdominal pain: a surgical audit of 1190 emergency admission. Br J Surg 76(11):1121–1125
Robinson TN, Wu DS, Pointer LP, Dunn CL, Cleveland JC, Moss M (2013) Simple frailty score predicts post-operative complications across surgical specialties. Am J Surg 206(4):544–550
Zattoni D, Montroni I, Saur NM, Garutti A, Reggiani MLB, Galetti C, Calogero P, Tonini V (2019) J Am Geriatr Soc 67(2):309–316
Biondo S, Pares D, Mora L, Rague JM, Kreisler E, Jaurrieta E (2003) Randomized clinical study of Gastrografin administration in patients with adhesive small bowel obstruction. Br J Surg 90(5):542–546
Joseph B, Pandit V, Sadoun M, Zangbar B, Fain MJ, Friese RS, Rhee P (2014) Frailty in surgery. J Trauma Acute Care Surg 76(4):1151–1156
Springer JE, Bailey JG, Davis PJ, Johnson PM (2014) Management and outcomes of small bowel obstruction in older adult patients: a prospective cohort study. Can J Surg 57(6):379–384
Pandit V, Khan M, Martinez C, Jehan F, Zeeshan M, Koblinski J, Hamidi M, Omesieta P, Osuchukwu O, Nfonsam V (2018) A modified frailty index predicts adverse outcomes among patients with colon cancer undergoing surgical intervention. Am J Surg 216(6):1090–1094
Lin H, Watts JN, Peel NM, Hubbard RE (2016) Frailty and post-operative outcomes in older surgical patients: a systematic review. BMC Geriatr 16(1):157
Lim SC, Koh AJH (2017) Nutrition and the elderly surgical patients. MOJ Surg 4(5):114–120
Ho JWC, Wu AHW, Lee MWK, Lau S, Lam P, Lau W, Kwok SSS, Kwan RYH, Lam C, Tam C, Lee S (2015) Malnutrition risk predicts surgical outcomes in patients undergoing gastrointestinal operations: results of a prospective study. Clin Nutr 34(4):679–684
Mosquera C, Koutlas NJ, Edwards KC, Strickland A, Vohra NA, Zervos EE, Fitzgerald TL (2016) Impact of malnutrition on gastrointestinal surgical patients. J Surg Res 205(1):95–101
Reames BN, Birkmeyer NJO, Dimick JB, Ghaferi AA (2014) Socioeconomic disparities in mortality after cancer surgery: failure to rescue. JAMA Surg 149(5):475–481
Birkmeyer NJO, Gu N, Baser O, Morris AM, Birkmeyer JD (2008) Socioeconomic status and surgical mortality in the elderly. Med Care 46(9):893–899
Sukumar S, Ravi P, Sood A, Gervais M, Su JC, Kim SP, Menon M, Roghmann F, Sammon JD, Sun M, Trinh VQ, Trinh QD (2015) Racial disparities in operative outcomes after major cancer surgery in the United States. World J Surg 39(3):634–643
McIsaac DI, Moloo H, Bryson GL, van Walraven C (2017) The association of frailty with outcomes and resource use after emergency general surgery: a population-based cohort study. Anesth Analg 124(5):1653–1661
Zogg CK, Olufajo OA, Jiang W, Bystricky A, Scott JW, Shafi S, Havens JM, Salim A, Schoenfeld AJ, Haider AH (2017) The need to consider longer-term outcomes of care: racial/ethnic disparities among adult and older adult emergency general surgery patients at 30, 90, and 180 days. Ann Surg 266(1):66–75
Khubchandani JA, Shen C, Ayturk D, Kiefe CI, Santry HP (2018) Disparities in access to emergency general surgery care in the United States. Surgery 163(2):243–250
Makary MA, Segev DL, Pronovost PJ, Syin D, Bandeen-Roche K, Patel P, Takenaga R, Devgan L, Holzmueller CG, Tian J, Fried LP (2010) Frailty as a predictor of surgical outcomse in older patients. J Am Coll Surg 210(6):901–908
Joseph B, Zangbar B, Pandit V, Fain M, Mohler MJ, Kulvatunyou N, Jokar TO, O’Keefe T, Friese RS, Rhee P (2016) Emergency general surgery in the elderly: too old or too frail? J Am Coll Surg 222(5):805–813
Acknowledgements
The authors would like to acknowledge the American Association for the Surgery of Trauma Patient Assessment Committee for its contribution to study concept.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Franchesca Hwang, Marie Crandall, Alan Smith, Neil Parry, and Amy Liepert have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor hold exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hwang, F., Crandall, M., Smith, A. et al. Small bowel obstruction in older patients: challenges in surgical management. Surg Endosc 37, 638–644 (2023). https://doi.org/10.1007/s00464-022-09428-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09428-y