Abstract
Purpose of Review
The purpose of this review is to discuss the evolving techniques and approaches for pericardiectomy, with a focus on the use of cardiopulmonary bypass (CPB) and the extent of radical pericardial resection. The review aims to highlight the benefits and considerations associated with these modifications in radical pericardiectomy.
Recent Findings
Recent studies have demonstrated that the use of CPB during pericardiectomy does not increase procedural risk or negatively impact survival. In fact, it has been shown to contribute to a more radical resection and improve postoperative outcomes, which is associated with less recurrence and better survival.
Summary
The review emphasizes the importance of radical pericardiectomy and the use of CPB in achieving successful outcomes. Radical resection of the pericardium, facilitated by CPB, helps minimize the risk of recurrent constrictions and the need for reinterventions. The findings highlight the correlation between postoperative outcomes and survival, further supporting the use of CPB.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Adler Y, Charron P, Imazio M, Badano L, Barón-Esquivias G, Bogaert J, et al. 2015 ESC Guidelines for the diagnosis and management of pericardial diseases: the Task Force for the Diagnosis and Management of Pericardial Diseases of the European Society of Cardiology (ESC) endorsed by: the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2015;36(42):2921–64.
• Chiabrando JG, Bonaventura A, Vecchié A, Wohlford GF, Mauro AG, Jordan JH, et al. Management of acute and recurrent pericarditis: JACC state-of-the-art review. J Am Coll Cardiol. 2020;75(1):76–92. This article provides an up-to-date overview of the current management of acute and recurrent pericarditis, outlining the various available medical treatment options, as well as considerations for when to choose surgical management.
•• Unai S, Johnston DR. Radical pericardiectomy for pericardial diseases. Curr Cardiol Rep. 2019;21(2):6. This article provides a clear and specific description of the surgical approach that is currently being performed most frequently.
Johnston DR. Surgical management of pericardial diseases. Prog Cardiovasc Dis. 2017;59(4):407–16.
Rodriguez ER, Tan CD. Structure and anatomy of the human pericardium. Prog Cardiovasc Dis. 2017;59(4):327–40.
Hoit BD. Anatomy and physiology of the pericardium. Cardiol Clin. 2017;35(4):481–90.
Syed FF, Schaff HV, Oh JK. Constrictive pericarditis—a curable diastolic heart failure. Nat Rev Cardiol. 2014;11(9):530–44.
• Oh NA, Hennecken C, Van den Eynde J, Doulamis IP, Avgerinos DV, Kampaktsis PN. Pericardiectomy and Pericardial window for the treatment of pericardial disease in the contemporary era. Curr Cardiol Rep. 2022;24(11):1619–31. This article summarizes contemporary practices in pericardial diseases. It emphasizes the diagnostic approach and current management of constrictive pericarditis, while also highlighting various studies that confirm the benefits of CPB in pericardiectomy.
Cremer PC, Kumar A, Kontzias A, Tan CD, Rodriguez ER, Imazio M, et al. Complicated pericarditis: understanding risk factors and pathophysiology to inform imaging and treatment. J Am Coll Cardiol. 2016;68(21):2311–28.
Fitzpatrick DP, Wyso EM, Bosher LH, Richardson DW. Restoration of normal intracardiac pressures after extensive pericardiectomy for constrictive pericarditis. Circulation. 1962;25(3):484–92.
Hemmati P, Greason KL, Schaff HV. Contemporary techniques of pericardiectomy for pericardial disease. Cardiol Clin. 2017;35(4):559–66.
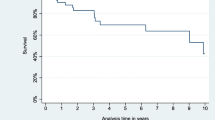
•• Tzani A, Doulamis IP, Tzoumas A, Avgerinos DV, Koudoumas D, Siasos G, et al. Meta-analysis of population characteristics and outcomes of patients undergoing pericardiectomy for constrictive pericarditis. Am J Cardiol. 2021;1(146):120–7. This systematic review and meta-analysis aim to describe the characteristics and outcomes of patients with constrictive pericarditis who underwent pericardiectomy, providing a comprehensive analysis of this population in the current era.
George TJ, Arnaoutakis GJ, Beaty CA, Kilic A, Baumgartner WA, Conte JV. Contemporary etiologies, risk factors, and outcomes after pericardiectomy. Ann Thorac Surg. 2012;94(2):445–51.
Komoda T, Frumkin A, Knosalla C, Hetzer R. Child-Pugh score predicts survival after radical pericardiectomy for constrictive pericarditis. Ann Thorac Surg. 2013;96(5):1679–85.
Avgerinos D, Rabitnokov Y, Worku B, Neragi-Miandoab S, Girardi LN. Fifteen-year experience and outcomes of pericardiectomy for constrictive pericarditis. J Card Surg. 2014;29(4):434–8.
Bertog SC, Thambidorai SK, Parakh K, Schoenhagen P, Ozduran V, Houghtaling PL, et al. Constrictive pericarditis: etiology and cause-specific survival after pericardiectomy. J Am Coll Cardiol. 2004;43(8):1445–52.
Gatti G, Fiore A, Ternacle J, Porcari A, Fiorica I, Poletti A, et al. Pericardiectomy for constrictive pericarditis: a risk factor analysis for early and late failure. Heart Vessels. 2020;35(1):92–103.
Kang SH, Song JM, Kim M, Choo SJ, Chung CH, Kang DH, et al. Prognostic predictors in pericardiectomy for chronic constrictive pericarditis. J Thorac Cardiovasc Surg. 2014;147(2):598–605.
Gillaspie EA, Stulak JM, Daly RC, Greason KL, Joyce LD, Oh J, et al. A 20-year experience with isolated pericardiectomy: analysis of indications and outcomes. J Thorac Cardiovasc Surg. 2016;152(2):448–58.
Nishimura S, Izumi C, Amano M, Imamura S, Onishi N, Tamaki Y, et al. Long-term clinical outcomes and prognostic factors after pericardiectomy for constrictive pericarditis in a Japanese population. Circ J. 2017;81(2):206–12.
•• Murashita T, Schaff HV, Daly RC, Oh JK, Dearani JA, Stulak JM, et al. Experience with pericardiectomy for constrictive pericarditis over eight decades. Ann Thorac Surg. 2017;104(3):742–50. The study highlights a notable shift in the etiology of the disease over the research period. It also demonstrates that long-term survival following pericardiectomy is influenced by various patient characteristics, including the etiology of the constriction and the severity of symptoms. This article, featuring the most extensive cohort of retrospective patients to date, underscores these significant findings.
Szabó G, Schmack B, Bulut C, Soós P, Weymann A, Stadtfeld S, et al. Constrictive pericarditis: risks, aetiologies and outcomes after total pericardiectomy: 24 years of experience†. Eur J Cardiothorac Surg. 2013;44(6):1023–8.
Pahwa S, Crestanello J, Miranda W, Bernabei A, Polycarpou A, Schaff H, et al. Outcomes of pericardiectomy for constrictive pericarditis following mediastinal irradiation. J Card Surg. 2021;36(12):4636–42.
Wang H, Wei J, Zheng Q, Meng L, Xin Y, Yin X, et al. Radiation-induced heart disease: a review of classification, mechanism and prevention. Int J Biol Sci. 2019;15(10):2128–38.
Koutroumpakis E, Deswal A, Yusuf SW, Abe JI, Nead KT, Potter AS, et al. Radiation-induced cardiovascular disease: mechanisms, prevention, and treatment. Curr Oncol Rep. 2022;24(5):543–53.
• Tabucanon RS, Wang TKM, Chetrit M, Furqan MM, Chan N, Pande A, et al. Worsened tricuspid regurgitation following pericardiectomy for constrictive pericarditis. Circ Cardiovasc Imaging. 2021;14(10):e012948. This article emphasizes the importance of assessing and managing tricuspid regurgitation in patients undergoing pericardiectomy, given its potential worsening after the procedure and its implications for patient survival.
Calderon-Rojas R, Greason KL, King KS, Oh JK, Stulak JM, Daly RC, et al. Tricuspid valve regurgitation in patients undergoing pericardiectomy for constrictive pericarditis. Semin Thorac Cardiovasc Surg. 2020;32(4):721–8.
Góngora E, Dearani JA, Orszulak TA, Schaff HV, Li Z, Sundt TM. Tricuspid regurgitation in patients undergoing pericardiectomy for constrictive pericarditis. Ann Thorac Surg. 2008;85(1):163–71.
Tariq MU, Aman W, Karwa A, Benatti R, Klein A. Right ventricular dilatation post pericardiectomy causes tricuspid regurgitation. J Am Coll Cardiol. 2015;65(10_Supplement):A1315–A1315.
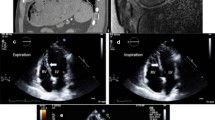
• Alajaji W, Xu B, Sripariwuth A, Menon V, Kumar A, Schleicher M, et al. Noninvasive multimodality imaging for the diagnosis of constrictive pericarditis. Circ Cardiovasc Imaging. 2018;11(11):e007878. This article provides a summary of the available multimodal imaging techniques used in the diagnosis of constrictive pericarditis, as well as their differentiation from other conditions such as restrictive cardiomyopathy using these images.
Klein AL, Abbara S, Agler DA, Appleton CP, Asher CR, Hoit B, et al. American Society of Echocardiography clinical recommendations for multimodality cardiovascular imaging of patients with pericardial disease: endorsed by the Society for Cardiovascular Magnetic Resonance and Society of Cardiovascular Computed Tomography. J Am Soc Echocardiogr. 2013;26(9):965–1012.e15.
Talreja DR, Nishimura RA, Oh JK, Holmes DR. Constrictive pericarditis in the modern era: novel criteria for diagnosis in the cardiac catheterization laboratory. J Am Coll Cardiol. 2008;51(3):315–9.
Feng D, Glockner J, Kim K, Martinez M, Syed IS, Araoz P, et al. Cardiac magnetic resonance imaging pericardial late gadolinium enhancement and elevated inflammatory markers can predict the reversibility of constrictive pericarditis after antiinflammatory medical therapy. Circulation. 2011;124(17):1830–7.
Brucato A, Lim-Watson MZ, Klein A, Imazio M, Cella D, Cremer P, et al. Interleukin-1 trap rilonacept improved health-related quality of life and sleep in patients with recurrent pericarditis: results from the phase 3 clinical trial RHAPSODY. J Am Heart Assoc. 2022;11(20):e023252.
Zhu P, Mai M, Wu R, Lu C, Fan R, Zheng S. Pericardiectomy for constrictive pericarditis: single-center experience in China. J Cardiothorac Surg. 2015;10(1):34.
Chowdhury UK, Seth S, Reddy SM. Pericardiectomy for chronic constrictive pericarditis via left anterolateral thoracotomy. Oper Tech Thorac Cardiovasc Surg. 2008;13(1):14–25.
Chowdhury UK, Subramaniam GK, Kumar AS, Airan B, Singh R, Talwar S, et al. Pericardiectomy for Constrictive pericarditis: a clinical, echocardiographic, and hemodynamic evaluation of two surgical techniques. Ann Thorac Surg. 2006;81(2):522–9.
Mitchell JD, Cehic DA, Morgia M, Bergom C, Toohey J, Guerrero PA, et al. Cardiovascular manifestations from therapeutic radiation: a multidisciplinary expert consensus statement from the International Cardio-Oncology Society. JACC CardioOncol. 2021;3(3):360–80.
Castro-Varela A, Schaff HV. Dr Stuart Harrington: historical challenges and success in pericardiectomy. JTCVS Open. 2022;2(10):303–7.
Johansson L. Diseases of the pericardium. In: Derra E, editor. Encyclopedia of Thoracic Surgery / Handbuch Der Thoraxchirurgie: Band / Volume 2: Spezieller Teil 1 / Special Part 1 [Internet]. Berlin, Heidelberg: Springer; 1959 [cited 2023 Aug 29]. p. 614–46. Available from: https://doi.org/10.1007/978-3-642-94757-5_13.
Churchill ED. Decortication of the heart (Delorme) for adhesive pericarditis. Arch Surg. 1929;19(6):1457–69.
McCaughan BC, Schaff HV, Piehler JM, Danielson GK, Orszulak TA, Puga FJ, et al. Early and late results of pericardiectomy for constrictive pericarditis. J Thorac Cardiovasc Surg. 1985;89(3):340–50.
Cho YH, Schaff HV, Dearani JA, Daly RC, Park SJ, Li Z, et al. Completion pericardiectomy for recurrent constrictive pericarditis: importance of timing of recurrence on late clinical outcome of operation. Ann Thorac Surg. 2012;93(4):1236–40.
Rupprecht L, Schmid C. More reasons for pericardiectomy without cardiopulmonary bypass. Ann Thorac Surg. 2018;105(4):1280.
Shiraishi M, Yamaguchi A, Muramatsu K, Kimura N, Yuri K, Matsumoto H, et al. Validation of Waffle procedure for constrictive pericarditis with epicardial thickening. Gen Thorac Cardiovasc Surg. 2015;63(1):30–7.
Aksüt M, Altaş Ö, Kırali K. Intraoperative accidents and postoperative complications in the surgery of the pericardium. In: Nistor CE, Tsui S, Kırali K, Ciuche A, Aresu G, Kocher GJ, editors. Thoracic surgery: cervical, thoracic and abdominal approaches [Internet]. Cham: Springer International Publishing; 2020 [cited 2023 Aug 30]. p. 663–9. Available from: https://doi.org/10.1007/978-3-030-40679-0_58.
Unzué L, García E, Díaz-Antón B, Fernández-Portales J, Teijeiro R, Rodríguez-del-Río M. Percutaneous closure of a giant coronary artery fistula after surgical pericardiectomy. Review of the literature. Cardiovasc Revasc Med. 2017;18(5):384–9.
Busch C, Penov K, Amorim PA, Garbade J, Davierwala P, Schuler GC, et al. Risk factors for mortality after pericardiectomy for chronic constrictive pericarditis in a large single-centre cohort. Eur J Cardiothorac Surg. 2015;48(6):e110–6.
• Fang L, Zheng H, Yu W, Chen G, Zhong F. Effects of intraoperative fluid management on postoperative outcomes after pericardiectomy. Front Surg. 2021;8:673466. This retrospective study underscores the significance of intravenous fluid management during surgery, emphasizing that employing restrictive fluid therapy is linked to enhanced postoperative recovery and advocates it as the suitable fluid management approach for patients undergoing pericardiectomy.
Vistarini N, Chen C, Mazine A, Bouchard D, Hebert Y, Carrier M, et al. Pericardiectomy for constrictive pericarditis: 20 years of experience at the Montreal Heart Institute. Ann Thorac Surg. 2015;100(1):107–13.
Maciolek K, Asfaw ZE, Krienbring DJ, Arnsdorf SE, Balkhy HH. Robotic endoscopic off-pump total pericardiectomy in constrictive pericarditis. Innovations. 2016;11(2):134–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Michael Zhen-Yu Tong reports consulting and speaking honorarium for Abbott and Abiomed. The other authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Moros, D., Zaki, A. & Tong, M.ZY. Surgical Approaches for Pericardial Diseases: What Is New?. Curr Cardiol Rep 25, 1705–1713 (2023). https://doi.org/10.1007/s11886-023-01986-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11886-023-01986-4