Abstract
Studies show a compelling association between gambling disorder and posttraumatic stress disorder. However, there have been no randomized controlled trials for this co-morbidity. The aim of the current study was to compare two evidence-based models, one that addresses both disorders and another that addresses gambling alone. Sixty-five men and women with gambling disorder and posttraumatic stress disorder were randomized to one of two treatment conditions delivered via telehealth, Seeking Safety (integrated treatment for gambling and posttraumatic stress disorder) or Cognitive-Behavioral Therapy for Pathological Gambling (for gambling alone), in a randomized controlled non-inferiority trial. Primary outcomes were net gambling losses and number of sessions gambling. Secondary outcomes were posttraumatic stress disorder symptoms, coping skills, general psychiatric symptoms, global functioning, and gambling cognitions. Assessment occurred at baseline, 6-weeks, 3 months (end of treatment) and 1-year. On most measures, including primary outcomes, participants improved significantly over time with no difference between treatment conditions. Seeking Safety patients had significantly higher session attendance. Effect sizes were large for gambling, posttraumatic stress disorder and coping. All other measures except one showed medium effect sizes. Therapeutic alliance, treatment satisfaction, and the telehealth format were all rated positively. This was the first randomized trial of Seeking Safety in a gambling disorder population. Seeking Safety showed comparable efficacy to an established gambling disorder intervention; and significantly higher Seeking Safety attendance indicates especially strong engagement. Our finding of overall comparable results between the two treatments is consistent with the comorbidity treatment literature.
Trial registration: ClinicalTrials.gov NCT02800096; Registration date: June 14, 2016.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gambling disorder (GD) is associated with several co-occurring mental health conditions (Petry et al., 2005). There is compelling evidence for an association between trauma and posttraumatic stress disorder (PTSD), and GD (Moore & Grubbs, 2021); Individuals with GD experience higher levels of childhood trauma and adverse childhood events than individuals with no such history (Hodgins et al., 2010; Lotzin et al., 2018; Poole et al., 2017). Estimates of PTSD among those in treatment for GD range from 12.5 to 34% (Ledgerwood et al., 2006). An epidemiological household survey found lifetime comorbidity between PTSD and GD is 14.8%; and GD is a significant predictor of PTSD (Kessler et al., 2008). Several studies show the relationship between gambling problems and childhood adversity (Kausch et al., 2006; Peltzer et al., 2006; Petry et al., 2005; Scherrer et al., 2007). There are also a growing number of studies that show trauma and PTSD to be highly co-morbid with GD (Biddle et al., 2005; Grubbs et al., 2018, 2019; Ledgerwood et al., 2015; Levens et al., 2005; Taber et al., 1987). However, there are currently no randomized trials of the efficacy of treatments that address co-morbid GD and PTSD. Moreover, evidence-based therapy for GD has not addressed PTSD and likewise, PTSD treatment studies have not addressed GD, nor even assessed for gambling problems.
The present study examined the relative efficacy of two evidence-based therapies: Seeking Safety (SS) and Cognitive Behavior Therapy for Pathological Gambling (CBT-PG), using a randomized controlled non-inferiority trial design.
SS is a present-focused, cognitive behavioral therapy adapted from its original use addressing SUD that provides psychoeducation and coping skills to address co-occurring PTSD and GD. SS is based on five principles (Najavits, 2002): (a) Safety; (b) Integrated treatment; (c) A focus on ideals; (d) An emphasis on three content areas: cognitive, behavioral, and interpersonal; and (e) Attention to clinician processes. Safety encompasses elements including discontinuing or at least decreasing addictive behavior such as problematic gambling, reducing suicidality, letting go of dangerous relationships (such as domestic abuse and addicted friends), gaining control over extreme symptoms such as dissociation, self-harm, and aggression toward others. The concept of first-stage treatment as stabilization and safety has been consistently recommended separately in both the PTSD and addiction literatures (Evans & Sullivan, 1995; Herman, 1992; Kofoed et al., 1993). SS is designed to treat PTSD and addiction simultaneously, and an integrated model is consistently recommended as more sensitive to patient needs. A survey of people with this addiction comorbidity found that they also prefer simultaneous treatment (Brown et al., 1998), a finding replicated with people who had PTSD and problem gambling (Najavits, 2011).
Each disorder individually, and in combination, leads to a loss of ideals. SS seeks to instill countervailing humanistic themes to restore patients' feeling of potential for a better future. The title of each topic is framed as a positive ideal that is the opposite of some pathological characteristic of PTSD and addiction. For example, the topic Honesty combats denial, lying, and the “false self”. The three content areas (cognitive, behavioral, and interpersonal) are each recovery domains that aim to address the “whole person”—mind, actions, and relationships. Finally, clinician processes are explicitly addressed in SS, including building an alliance, compassion for patients’ experience and using adaptive coping skills in one’s own life.
Because SS is present-focused, it does not require patients to describe past trauma, thus promoting stabilization and functioning. It has no known adverse events in over 20 years of implementation among substance use treatment populations across thousands of programs and as documented in a major multisite trial (Killeen et al., 2008). SS is easy to follow and written in clear language; it has been used with highly diverse patients in age, ethnicity, reading level, cognitive ability, and level of symptoms and chronicity. Its high flexibility represents an important public health goal: to provide effective treatment with diverse settings, clinicians, and patients. It has also been successfully conducted by peers (Najavits et al., 2014).
SS is the only integrated PTSD/addiction model that has been studied in any problem gambling population. Clinicians are trained to apply SS to current problems in patients' lives, and thus the coping skills can be applied to any addiction and any trauma, as well as other problem areas of a person’s life. SS has been successfully implemented with diverse populations including patients with homelessness, domestic violence, adolescents, military veterans, criminal justice involvement, people living with HIV, people living with serious and persistent mental illness, as well as people of diverse ethnicities and cultures (Najavits et al., 2013). SS was, from the beginning, designed for flexible implementation as patients with PTSD and addictions enter treatment through many pathways.
There has been one pilot study of SS for GD (Najavits et al., 2013), conducted by a Canadian treatment program. The SS pilot study on PTSD and GD evaluated seven men and women outpatients with current comorbid GD and PTSD, and included 29% minorities (Najavits et al., 2013). Improvements were found on several measures of PTSD/trauma, gambling, functioning and psychopathology. One variable indicated worsening (employment), possibly reflecting measurement issues. SS attendance was excellent (average of 18.86 sessions). The overall conclusion was that SS can be effectively conducted for comorbid PTSD and GD, with improvements in numerous domains and high acceptability. However, this was a small-sample pilot, with important methodology limitations.
CBT-PG was selected as the comparison intervention in this non-inferiority trial for several reasons. First, there is a strong evidence-base for CBT-PG. CBT in general is the most evidence-based type of behavioral therapy for GD (Cowlishaw et al., 2012; Petry et al., 2017), and within different CBTs, the CBT-PG developed by Dr. Ladouceur is one of the earliest and strongest in its evidence-base. Both Sylvain et al. (1997) and Ladouceur et al. (2001) compared CBT-PG to a wait-list control in samples with GD, and both studies found that CBT-PG showed greater improvement on gambling outcomes and maintenance of gains through one year. Smith et al., (2013) compared the cognitive modules to a behavioral exposure model in a sample with problem gambling and found that both study arms showed significant improvement in gambling which was maintained through 6-month follow-up. Second, CBT-PG is a 12-session model, thus allowing for equivalent-dosage comparison as SS also is evidence-based in 12-session delivery (Hien et al., 2015; Najavits et al., 2013). Furthermore, CBT-PG focuses only on gambling and not on PTSD. Thus, it allowed us to compare a model that addresses addiction only (CBT-PG) to an integrated model designed to address both addiction and PTSD (SS). This question—the impact of integrated versus non-integrated treatment for co-occurring disorders (COD)—is one of the key issues in the COD field currently (Torchalla et al., 2012), and has never been studied in relation to GD and PTSD. Thus, our aim was to conduct a randomized controlled non-inferiority trial of SS compared with CBT-PG.
Method
Study Design
This non-inferiority RCT compared telehealth-delivered SS to CBT-PG. Both models were identical in terms of dosage; only their content differed. They were conducted in weekly individual sessions of 1 h, with end of treatment at 3 months. Follow-up assessments occurred at post-treatment and 12 months. We used intent-to-treat analysis and followed all patients at all assessment points regardless of intervention attendance (Walker et al., 2006). Patients were allowed to receive any other services they naturalistically were receiving or sought out ("treatment as usual"; TAU), for ethical reasons and to promote generalizability. The only exception was current formal PTSD treatment as described in our exclusionary criteria below. We sought to control for modality (individual telehealth) and gambling treatment (both treatments address it), while varying PTSD focus (only SS provided it). The study was approved by the research ethics board of the University of Windsor as well as the New England Institutional Review Board (IRB). The University of Manitoba and Wayne State University approved the University of Windsor as the IRB of record.
Participants
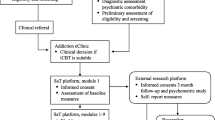
Our sample was recruited from the adult population of the provinces of Manitoba and Ontario, Canada. Recruitment occurred via: (a) online forums (e.g., Craigslist); (b) email to gambling and mental health programs; and (c) posting on professional listservs. All potential participants underwent a brief web-based screen to determine potential eligibility prior to completing the informed consent form. Recruitment is shown in the CONSORT diagram (Fig. 1). Participants were enrolled starting October 2016, and data collection ended in June 2021 at the end of the funding period.
We randomized 65 men and women with current comorbid GD and PTSD across the full range of severity of both disorders (GD could be mild, moderate or severe; PTSD could be full or subthreshold), for the broadest possible public health relevance (Ferris, & Wynne, 2001; McLaughlin et al., 2015). Our definition of GD was based on the Diagnostic Interview for Gambling Severity for DSM-5. Our definition of PTSD was based on the PTSD criteria for DSM-5 using the Clinician-Administered PTSD Scale (CAPS) (Weathers et al., 2013a, 2013b), which is widely viewed as the gold-standard PTSD assessment (Foa et al., 2010). Our scoring of the CAPS for study inclusionary purposes (including both PTSD and subthreshold PTSD) was consistent with the National Center for PTSD—established criteria (total score of 0–19 = asymptomatic/few symptoms, 20–39 = mild PTSD/subthreshold, 40–59 = moderate PTSD/threshold, 60–79 = severe PTSD symptomatology, ≥ 80 = extreme PTSD symptomatology).
Exclusion criteria were: current uncontrolled psychotic or bipolar I disorder; suicidal or homicidal ideation with intent and/or plan; and currently engaging in or planning to engage in manualized, formal, evidence-based PTSD therapy (e.g., Eye Movement Desensitization or Reprocessing Therapy; Prolonged Exposure; Cognitive Processing Therapy) as those would confound our evaluation of SS. We allowed other types of treatments (e.g., Gambler’s Anonymous, medication, other therapies) for several reasons. First, given the telehealth nature of our study, we were not going to be providing face-to-face clinical contact, and ethically it would have been inappropriate to prohibit face-to-face care. Second, in the real-world patients who attend a telehealth intervention would not be restricted from attending other treatments, thus reducing generalizability. Third, patients with a clinical emergency would be referred to any necessary care. We kept our exclusionary criteria minimal to promote generalizability.
Basis for Sample Size
Interpretation of non-inferiority results is based on the two-sided 95% confidence intervals (CI) of the group difference. It was decided a priori that if the lower two-sided 95% confidence limit of the group difference were to lie above the predefined non-inferiority limit (D), which marks the limit for clinically not relevant group differences, non-inferiority of the SS to CBT-PG would be concluded (i.e., SS is no worse than CBT-PG). For determining the non-inferiority limit, we relied on Ladouceur et al. (2001) which is the most relevant RCT as it evaluated CBT-PG and used two variables that are considered key outcomes for gambling treatment trials, per the Alberta consensus statement (Walker et al., 2006): total amount of money spent on gambling and frequency of gambling. We used posttest data on those two variables. The non-inferiority limit (D) was predefined as < 0.5 of the CBT effect. Alpha level was set at 0.05 for the power calculations. The null hypothesis to reject states SS is worse than CBT-PG in decreasing gambling problems. For the proposed study, a sample of 70 participants (n = 35 per arm) would, for “total amount of money spent on gambling,” assuming mss = 44, mCBT = 39, and SD = 173, result in a power of 85% to reject the null hypothesis. Likewise, for “number of gambling sessions” with mss = 0.7, mCBT = 0.5, and SD = 1.4, we would have a power of 88% to reject the null hypothesis. Our final analytic sample was 65 participants, which is slightly lower than our projected sample.
Transparency and Openness
We report how we determined our samples size, and all study procedures consistent with the Journal Article Reporting Standards (JARS; Appelbaum et al., 2018).
Randomization and Conduct of Treatments
Randomization was conducted using a web-based clinical trials randomizer. To keep the study blind, a staff member (not the PI or study assessor) was responsible for randomization.
Both treatments were conducted in individual format as: (a) both CBT-PG and SS are evidence-based in this modality; and (b) it is most feasible for scheduling telehealth sessions. Sessions were conducted weekly for 12 weeks. Clinician training and fidelity monitoring were conducted in identical dosage for each condition. The developer of each model (Dr. Najavits for SS and Dr. Ladouceur for CBT-PG) conducted an initial 1-day therapist training via webinar. Fidelity checks were conducted by expert raters. We recruited four Manitoba-based clinicians, two clinicians per study arm with no cross-over between arms so as to avoid contamination.
Seeking Safety
The SS manual provides a clinician guide and patient handouts. Each SS session focuses on a topic that represents a safe coping skill relevant to both PTSD and gambling. There are 25 SS topics, but the model was designed for a high level of flexibility and any number of topics can be done in the time available (Najavits, 2009). Each SS topic offers: (a) A brief summary; (b) A clinician orientation that provides background about the topic, clinical strategies for conducting the session, discussion of counter-transference issues, and "tough cases" of typical difficulties patients may raise; (c) A quotation that is read aloud at the start of each session to emotionally engage patients; (d) A patient handout that summarizes the main points in the session and ideas for “commitments” (i.e., homework). The session structure has: (a) Check-in: patients report, since the last session, addictive behavior frequency and quantity (and any other unsafe behaviors), positive coping, emotional state, and completion of the homework (about 5 min); (b) Quotation: the quotation is read aloud and discussed (about 3 min); (c) Relate the topic to patients' lives: the topic (a safe coping skill) is taught and rehearsed (30–40 min); (d) Check-out: patients name one thing they got out of the session and select a "commitment" (homework) to complete.
CBT-PG
This evidence-based 12-session GD model by Ladouceur and Lachance (Ladouceur et al., 2007a, 2007b) has two primary components: cognitive correction and relapse prevention, plus a session of motivational interviewing. Cognitive correction helps to correct patients’ misconceptions about randomness, with four targets: (a) understanding the idea of randomness (e.g., each “throw of the dice” is independent); (b) understanding erroneous beliefs held by gamblers (e.g., how an illusion of control contributes to gambling habits); (c) erroneous perceptions that predominate during gambling, e.g., making links between independent events; and (d) correcting verbalizations and faulty beliefs using a recording of the patient’s verbalizations during a session of imaginal gambling (“If I lose four times in a row, I will win for sure the next time”). Relapse prevention is based on Marlatt and Donovan’s (2005) model, including promoting awareness of high-risk situations and thoughts that might lead to gambling again. Motivational enhancement derives from Miller and Rollnick (1991) to build motivation to work on recovery from problem gambling.
Measures
We conducted three major assessments at which all measures were collected: baseline, end of treatment (EOT), and 12-month follow-up (except for the SCID exclusionary criteria modules for mania and psychosis). We also had one minor assessment at 6 weeks (treatment midpoint) comprised of a smaller battery. Patients were paid $40 for each major assessment, and $25 for the minor assessment via Amazon gift cards. The first three assessments were paid after the post-treatment assessment ($105 total), with the final assessment paid upon completion of the 12 month follow-up.
Basic Eligibility Screen
We used a GD/PTSD screening used in our prior pilot SS study, which also includes demographics (age, ethnicity, etc.).
Psychopathology
We used the Clinician-Administered PTSD Scale (CAPS) to assess DSM-5 PTSD (Najavits, 2009), with an inclusion severity score of 20 or higher (see Participants section). The Diagnostic Interview of Gambling Severity (DIGS) was used to assess for current DSM-5 GD (Winters et al., 2002). To ensure current GD, we confirmed that patients reported past-month gambling on the Timeline Follow-back. We used the MINI Neuropsychiatric Interview to assess for the study exclusion diagnoses. Our primary outcomes, money spent gambling and number of gambling sessions, were assessed per the Alberta consensus guidelines. Money spent gambling was net loss in the prior month using the Timeline Follow-back (Hodgins et al., 2003; Walker et al., 2006). Number of gambling sessions was assessed as number of days in the past month during which gambling occurred, using the Timeline Follow-back. These primary outcomes were assessed by a blind rater at all timepoints.
Secondary outcomes included the PTSD Checklist (PCL) for DSM-5 (), as the PCL has been found highly convergent with the CAPS, and the Trauma Symptom Checklist 40 (Briere, 1996), which assesses a broader range of trauma symptoms than the PCL. We also included the Brief Symptom Inventory 18 (Derogatis, 2001) for overall psychiatric symptoms, and the Brief Addiction Monitor (Cacciola et al., 2013) as SUD is often comorbid with gambling problems.
Coping/Functioning/Cognition
The Gamblers’ Beliefs Questionnaire (Steenbergh et al., 2002), and Gambling Self-Efficacy Questionnaire (May et al., 2003) were used to assess secondary aspects of GD including gambling related cognitive distortions and perceived efficacy to control one’s gambling behavior. The PTSD World Assumptions Scale was included to assess patients’ assumptions about the world and meaningfulness of events (Janoff-Bulman, 1989). The Basis-32 was included to assess overall physical and psychological functioning (Eisen et al., 1999). The Coping Self-Efficacy Scale was used to assess patients’ perceived ability to cope with life stressors (Tobin et al., 1989).
Treatment Measures
Helping Alliance Questionnaire (HAQ) (Luborsky et al., 1996) was used to assess the degree to which patients experienced treatment as helpful. The Treatment Services Review (McLellan, 1989) was used to assess patient use of other (TAU) treatments. The Client Satisfaction Questionnaire (CSQ) (Larsen et al., 1979) was used to assess treatment satisfaction. Finally, the Telepresence in Videoconference Scale (TVS) (Bouchard et al., 2006) was used to evaluate acceptability of the telehealth format.
Fidelity for SS was assessed using the SS Adherence Scale (Najavits, & Liese, 2003), and for CBT-PG using the fidelity check measure for that model (Smith et al., 2011) rotating across sessions and patients (to sample across treatment content), based on the full recording per session (telehealth sessions were recorded). Fidelity was rated by individual expert in SS and CBT-PG, respectively.
Measures were collected at baseline, midpoint (6 weeks), and end of treatment (EOT), as well as 12 month follow-up, except the MINI, the CAPS and DIGS (done at all points except mid-point), the CSQ, and the TVS (done at mid-point and end of treatment only). At 6 weeks a smaller battery was collected, consisting of the two primary outcomes (net loss of money spent gambling and number of days gambling in past month), the two trauma measures (PCL, TSC-40), the BSI-18, and the BASIS-32. Data collection was electronic for self-report measures and phone for interview-based measures.
Data Analysis
We used descriptive statistics to characterize the sample and two-tailed independent samples t-tests or chi square tests to compare by study condition at baseline. To minimize Type 1 error, we analyzed one summary score per variable rather than including subscales except for the BAM, which has three summary scores (risk, use and protective factors). We used multiple imputation procedures in SPSS to address missing data to include the full intent-to-treat sample; we used the pooled result of 100 imputations. For continuous variables, imputed outcome data were analyzed with two-way mixed analysis of variance (ANOVA). Mauchley’s test of sphericity was conducted and if significant, Greenhouse–Geisser estimates were used. Effect sizes are reported as partial eta-squared and interpreted as 0.01 (small), 0.09 (medium), and 0.25 (large) (Watson et al., 2016). All results are reported on the intent-to-treat sample.
Results
There were no differences between treatment conditions on any characteristic at baseline, so the full sample is described here. The mean age of the sample was 44.93 (sd = 11.99). In terms of gender, 58.7% was female, 39.7% male, and 1.7% nonbinary. Race/ethnicity was 68.8% White, 31.3% minority. In the sample, minority representation was 12.5% Indigenous, 9.4% Asian, 6.3% Black and 3.2% Hispanic. The most common gambling types were: slots (76.1% of the sample), internet gambling (48.5%), lottery (48.5%) and blackjack (34.3%). The two treatment conditions did not differ at baseline on any of the twelve gambling types surveyed.
Outcomes are summarized in Table 1. Overall, the findings were highly consistent. On almost every measure the sample improved significantly over time but there was no difference between treatment conditions. This held true on our primary outcomes (gambling net losses and number of gambling sessions) as well as secondary outcomes that included psychopathology, beliefs about gambling, gambling self-efficacy, functioning, PTSD symptoms on both interview and self-report measures, and coping. The only non-significant measures were the Columbia Suicide Scale (though that did reach trend level) and the World Assumptions Scale. The only significant difference between treatment conditions (across all study results) was that SS had higher session attendance than CBT-PG: Mean = 8.61 (sd = 4.59) vs. 6.03 (sd = 0.4.48), t = 2.24, p < 0.03.
We found large effect sizes for change across time for gambling (number of sessions gambled, DIGS number of symptoms, and gambling self-efficacy) and PTSD (the PTSD Checklist and the CAPS), as well as coping (the Coping Self-Efficacy Scale). There were medium effect sizes on all other measures (net loss gambling, Gamblers Beliefs, Trauma Symptom Checklist and the Brief Symptom Inventory) except the BASIS-32, which had a small effect size. We are not interpreting the effect size for the Columbia Suicide Scale or World Assumptions Scale as the main effects for these were not significant.
As for which timepoints showed change, the predominant pattern of significant improvement was from baseline to later timepoints (6 weeks, end of treatment, and sometimes to one-year follow-up) as noted by the significant “a”, “b” and “c” entries in the last column of Table 1. On one measure there was continued improvement from end of treatment to one-year follow-up (Gambling Self-Efficacy Questionnaire). However, three measures showed significant worsening from end of treatment to 12 months follow-up (the DIGS, Gamblers Beliefs Questionnaire and the Coping Self-Efficacy Scale). Yet on all three of these measures, patients were still significantly improved compared to baseline.
Therapeutic alliance, scaled 1–6 with higher scores representing better alliance, was strong in both treatment conditions at 5.19 for SS (sd = 0.54) and 4.57 for CBT-PG (sd = 0.22) at 6 weeks, with no difference between conditions. The patient satisfaction scale, scaled 0–3, had the same pattern: very strong in SS (M = 2.26, sd = 0.41) and CBT-PG (M = 2.39, sd = 0.28) with no difference between them. The telepresence scale, scored 0–10 (higher is better) assessing acceptability of the telehealth format, showed high acceptability (SS M = 7.84, sd = 1.54, CBT-PG M = 7.84, sd = 1.54) with no difference between conditions.
On the Treatment Services Review patients were asked about their past-month use of behavioral treatments or support (such as 12-step groups) aside from the study treatment they were receiving. Patients in SS showed an increase in total number of sessions across all types from 2.12 (sd = 4.10) at baseline to 7.89 at 6 weeks (sd = 7.11) to 6.65 (sd = 6.24) at end of treatment. Patients in CBT-PG had 6.41 (sd = 9.11) to 5.95 (sd = 9.37) to 5.38 (sd = 6.09) respectively.
Fidelity spot checks for both treatments indicated that all therapists met the fidelity standards for their treatment, with no concerns.
Discussion
This is the first RCT of behavioral therapies for co-occurring GD and PTSD. It was encouraging to see that SS, which has never before had an RCT in a GD population, showed equivalent outcome results to an established evidence-based therapy for GD (CBT-PG). Further, CBT-PG, which does not address PTSD explicitly, showed improvements on PTSD as well as gambling. Our finding of both treatments performing equally well converges with the literature on evidence-based practices, which consistently finds no difference among well-constructed treatments (Najavits et al., 2020). Although it may be surprising that the gambling-only CBT-PG did just as well on PTSD as the integrated SS, this too is consistent with the existing literature on integrated treatments for PTSD/SUD (Najavits et al., 2020). Various studies of GD treatments have also found improvements in mental health symptoms in addition to GD (Carlbring et al., 2008; Petry et al., 2006). The good news is that multiple treatment options work, allowing clinicians and patients to choose what they prefer.
The only difference between conditions was higher treatment attendance in SS. Perhaps by addressing PTSD, not just GD, patients were more engaged in treatment. This conclusion is consistent with research showing patients with both PTSD and GD are more interested in PTSD treatment than gambling treatment (Najavits, 2011).
Another positive finding was that patients improved across time on almost all study measures, including gambling, PTSD, other psychiatric symptoms, functioning, and coping. The strong effect sizes on GD, PTSD and coping measures indicates that the treatments were helpful, which is an important finding as this population is known to be difficult to reach, with low treatment engagement. We also found medium effect sizes on other study measures, representing important additional outcomes (gambling cognitions, functioning, and psychiatric symptoms).
Our use of telehealth for service delivery likely enhanced treatment engagement. Patients gave strong satisfaction ratings regarding telehealth delivery (as well as treatment satisfaction and therapeutic alliance). There have been few studies that delivered GD treatment remotely, but all of those also showed GD symptom improvement (Carlbring et al., 2008; Hodgins et al., 2001, 2009). No published studies have directly compared CBT for GD delivered remotely to CBT delivered in person. However, a direct comparison of telehealth and in-person general counseling for GD revealed equal effectiveness between the two modalities (Tse et al., 2013). A recent review noted that, by and large, telehealth treatments for addictions result in comparable findings to in-person treatment, and that telehealth may improve engagement through increased treatment access and convenience (e.g., Mark et al., 2022). The relative dearth of direct comparisons between telehealth and in-person treatments coupled with a lack of a waitlist or no-treatment control group in the present study warrants some caution around interpretation of the generalizability of our findings. Nevertheless, our trial began prior to the COVID-19 pandemic but is certainly timely given the rapid increase in telehealth for addiction and mental health disorders (Blanco et al., 2021; Monaghesh et al., 2020).
Only two measures did not show a pattern of improvement: the World Assumptions Scale and the Columbia Suicide Scale. The latter likely did not have a finding because the base rate for suicide is low, although it is always important to assess given the strong association between gambling problems and suicide (Ledgerwood et al., 2004, 2005). A small number of measures (gambling severity and coping self-efficacy) showed significant worsening from end of treatment to 12-month follow-up despite demonstrating improvement from baseline. These end of treatment to 12-month results indicate the need for continued therapy to help people sustain gains achieved during treatment. Both PTSD and GD are chronic conditions, especially for those with severe disorders.
Patients in both conditions reported use of additional supports and services. There is no interpretation of these findings per se (increasing use of treatment could be considered positive or negative, depending on the individual patient). However, it is part of the SS model to encourage people to use outside supports; and given their low rate of resource usage at baseline it makes sense that SS patients would increase use of supports over time.
Strengths and Limitations
Some of the methodological strengths of our study include strong minority participation; interview-based diagnoses of GD and PTSD; blind evaluation of primary outcomes; fidelity assessment; and use of validated measures.
There were, however, several limitations. Our sample size, although adequate for assessing the study aims, was small. Larger trials may have greater power to detect smaller effect sizes between treatment conditions. Because of our recruitment methods (largely online advertisements), our sample is not representative of all GD populations. Our study assessments relied on patient self-report, and there are no biochemical measures to detect the presence of gambling behavior or PTSD symptoms. This is a limitation of all studies of GD and PTSD. Due to sample size limitations, we were not able to conduct analyses to explore the impact of GD or PTSD symptom severity on outcomes. Nor were we able to conduct analyses to disentangle therapist effects. Much larger sample sizes would be required to explore these issues. Finally, we did not include a non-treatment control or waitlist condition, which would have allowed us to determine the efficacy of SS and CBT-PG compared to either no-treatment or only additional treatment sought in the community. We decided against a no-treatment condition in part due to practicalities such as cost and length of the study. Also, we viewed it as unethical to withhold treatment from those seeking care, especially as both treatment models in our study were already evidence-based for either PTSD or PG, showing superiority to minimal-care approaches (Najavits et al., 2013; Sylvain et al., 1997).
Implications and Conclusions
Our study has implications for the study of GD treatments. Few trials have examined the efficacy of behavioral therapies for GD, and few studies focus on treatment of co-occurring psychopathology in addition to GD (Ladouceur et al., 2001). The present trial demonstrates that concurrent treatment of gambling and PTSD symptoms may result in greater treatment engagement, as shown by increased session attendance. The telehealth format of our study, which was determined prior to the COVID-19 pandemic, has implications for delivery of GD and PTSD treatment for individuals who have barriers to accessing care. Taken together, our study findings show the importance of addressing co-occurring GD and PTSD, and that effective options are available for the treatment of these comorbid conditions.
Data Availability
The datasets generated and analysed for the current study are not publicly available due to the fact that study participants did not give permission for their data to be released.
References
Appelbaum, M., Cooper, H., Kline, R. B., Mayo-Wilson, E., Nezu, A. M., & Rao, S. M. (2018). Journal article reporting standards for quantitative research in psychology: The APA Publications and Communications Board Task Force Report. American Psychologist, 73, 3–25.
Biddle, D., Hawthorne, G., Forbes, D., & Coman, G. (2005). Problem gambling in Australian PTSD treatment-seeking veterans. Journal of Traumatic Stress: Official Publication of the International Society for Traumatic Stress Studies, 18(6), 759–767. https://doi.org/10.1002/jts.20084
Blanco, C., Compton, W. M., & Volkow, N. D. (2021). Opportunities for research on the treatment of substance use disorders in the context of COVID-19. JAMA Psychiatry, 78(4), 357–358. https://doi.org/10.1001/jamapsychiatry.2020.3177
Bouchard, S., & Robillard, G. (2006). Telepresence in videoconference scale. Université du Québec en Outaouais.
Briere, J. (1996). Trauma symptom checklist for children. Odessa, FL: Psychological Assessment Resources, 00253-8.
Brown, P. J., Stout, R. L., & Gannon-Rowley, J. (1998). 15Substance Use disorder-PTSD Comorbidity: Patients’ perceptions of symptom interplay and treatment issues. Journal of Substance Abuse Treatment, 15(5), 445–448. https://doi.org/10.1016/S0740-5472(97)00286-9
Carlbring, P., & Smit, F. (2008). Randomized trial of internet-delivered self-help with telephone support for pathological gamblers. Journal of Consulting and Clinical Psychology, 76(6), 1090–1094. https://doi.org/10.1037/a0013603
Cowlishaw, S., Merkouris, S., Dowling, N., Anderson, C., Jackson, A., & Thomas, S. (2012). Psychological therapies for pathological and problem gambling. Cochrane Database of Systematic Reviews, (11). https://doi.org/10.1002/14651858.CD008937.pub2
Cacciola, J. S., Alterman, A. I., DePhilippis, D., Drapkin, M. L., Valadez Jr, C., Fala, N. C., ... & McKay, J. R. (2013). Development and initial evaluation of the Brief Addiction Monitor (BAM). Journal of Substance Abuse Treatment, 44(3), 256–263. https://doi.org/10.1016/j.jsat.2012.07.013
Derogatis, L. R. (2001). Brief symptom inventory 18. Johns Hopkins University.
Eisen, S. V., Wilcox, M., Leff, H. S., Schaefer, E., & Culhane, M. A. (1999). Assessing behavioral health outcomes in outpatient programs: Reliability and validity of the BASIS-32. The Journal of Behavioral Health Services & Research, 26(1), 5–17. https://doi.org/10.1007/BF02287790
Evans, K., & Sullivan, J. M. (1995). Treating addicted survivors of trauma. Gulford.
Ferris, J. A., & Wynne, H. J. (2001). The Canadian problem gambling index (pp. 1–59). Ottawa, ON: Canadian Centre on substance abuse.
Foa, E. B., Keane, T. M., Friedman, M. J., & Cohen, J. A. (Eds.). (2010). Effective treatments for PTSD: Practice guidelines from the International Society for Traumatic Stress Studies. Guilford.
Grubbs, J. B., Chapman, H., Milner, L., Gutierrez, I. A., & Bradley, D. F. (2018). Examining links between posttraumatic stress and gambling motives: The role of positive gambling expectancies. Psychology of Addictive Behaviors, 32(7), 821–831. https://doi.org/10.1037/adb0000399
Grubbs, J. B., Chapman, H., & Shepherd, K. A. (2019). Post-traumatic stress and gambling related cognitions: Analyses in inpatient and online samples. Addictive Behaviors, 89, 128–135. https://doi.org/10.1016/j.addbeh.2018.09.035
Herman, J. L. (1992). Trauma and recovery. Basic Books.
Hien, D. A., Levin, F. R., Ruglass, L. M., López-Castro, T., Papini, S., Hu, M.-C., Cohen, L. R., & Herron, A. (2015). Combining seeking safety with sertraline for PTSD and alcohol use disorders: A randomized controlled trial. Journal of Consulting and Clinical Psychology, 83(2), 359–369. https://doi.org/10.1037/a0038719
Hodgins, D. C., Currie, S. R., & El-Guebaly, N. (2001). Motivational enhancement and self-help treatments for problem gambling. Journal of Consulting and Clinical Psychology, 69(1), 50–57. https://doi.org/10.1037/0022-006X.69.1.50.
Hodgins, D. C., Currie, S. R., Currie, G., & Fick, G. H. (2009). Randomized trial of brief motivational treatments for pathological gamblers: More is not necessarily better. Journal of Consulting and Clinical Psychology, 77(5), 950–960. https://doi.org/10.1037/a0016318
Hodgins, D. C., & Makarchuk, K. (2003). Trusting problem gamblers: Reliability and validity of self-reported gambling behavior. Psychology of Addictive Behaviors, 17(3), 244–248. https://doi.org/10.1037/0893-164X.17.3.244
Hodgins, D. C., Schopflocher, D. P., el-Guebaly, N., Casey, D. M., Smith, G. J., Williams, R. J., & Wood, R. T. (2010). The association between childhood maltreatment and gambling problems in a community sample of adult men and women. Psychology of Addictive Behaviors, 24(3), 548. https://doi.org/10.1037/a0019946.
Janoff-Bulman, R. (1989). World assumptions scale. University of Massachusetts at Amherst.
Kausch, O., Rugle, L., & Rowland, D. Y. (2006). Lifetime histories of trauma among pathological gamblers. The American Journal on Addictions, 15(1), 35–43. https://doi.org/10.1080/10550490500419045
Kessler, R. C., Hwang, I., LaBrie, R., Petukhova, M., Sampson, N. A., Winters, K. C., & Shaffer, H. J. (2008). DSM-IV pathological gambling in the National Comorbidity Survey Replication. Psychological Medicine, 38(9), 1351–1360. https://doi.org/10.1017/S0033291708002900
Killeen, T., Hien, D., Campbell, A., Brown, C., Hansen, C., Jiang, H., & Nunes, E. (2008). Adverse events in an integrated trauma-focused intervention for women in community substance abuse treatment. Journal of Substance Abuse Treatment, 35(3), 304–311. https://doi.org/10.1016/j.jsat.2007.12.001.
Kofoed, L., Friedman, M. J., & Peck, R. (1993). Alcoholism and drug abuse in patients with PTSD. Psychiatric Quarterly, 64(2), 151–171. https://doi.org/10.1007/BF01065867
Ladouceur, R., Sylvain, C., Boutin, C., Lachance, S., Doucet, C., Leblond, J., & Jacques, C. (2001). Cognitive treatment of pathological gambling. The Journal of Nervous and Mental Disease, 189(11), 774–780. https://doi.org/10.1097/00005053-200111000-00007
Ladouceur, R., & Lachance, S. (2007a). Overcoming pathological gambling: Therapist guide. Oxford University Press.
Ladouceur, R., & Lachance, S. (2007b). Overcoming your pathological gambling: Workbook. Oxford University Press.
Larsen, D. L., Attkisson, C. C., Hargreaves, W. A., & Nguyen, T. D. (1979). Assessment of client/patient satisfaction: Development of a general scale. Evaluation and Program Planning, 2(3), 197–207. https://doi.org/10.1016/0149-7189(79)90094-6
Ledgerwood, D. M., & Milosevic, A. (2015). Clinical and personality characteristics associated with post traumatic stress disorder in problem and pathological gamblers recruited from the community. Journal of Gambling Studies, 31(2), 501–512. https://doi.org/10.1007/s10899-013-9426-1
Ledgerwood, D. M., & Petry, N. M. (2004). Gambling and suicidality in treatment-seeking pathological gamblers. The Journal of Nervous and Mental Disease, 192(10), 711–714. https://doi.org/10.1097/01.nmd.0000142021.71880.ce
Ledgerwood, D. M., & Petry, N. M. (2006). Posttraumatic stress disorder symptoms in treatment-seeking pathological gamblers. Journal of Traumatic Stress: Official Publication of the International Society for Traumatic Stress Studies, 19(3), 411–416. https://doi.org/10.1002/jts.20123
Ledgerwood, D. M., Steinberg, M. A., Wu, R., & Potenza, M. N. (2005). Self-reported gambling-related suicidality among gambling helpline callers. Psychology of Addictive Behaviors, 19(2), 175–183. https://doi.org/10.1037/0893-164X.19.2.175
Levens, S., Dyer, A. M., Zubritsky, C., Knott, K., & Oslin, D. W. (2005). Gambling among older, primary-care patients: An important public health concern. The American Journal of Geriatric Psychiatry, 13(1), 69–76. https://doi.org/10.1097/00019442-200501000-00010
Lotzin, A., Ulas, M., Buth, S., Milin, S., Kalke, J., & Schäfer, I. (2018). Profiles of childhood adversities in pathological gamblers: A latent class analysis. Addictive Behaviors, 81, 60–69. https://doi.org/10.1016/j.addbeh.2018.01.031
Luborsky, L., Barber, J. P., Siqueland, L., Johnson, S., Najavits, L. M., Frank, A., & Daley, D. (1996). The revised helping alliance questionnaire (HAq-II): Psychometric properties. The Journal of Psychotherapy Practice and Research, 5(3), 260.
Mark, T. L., Treiman, K., Padwa, H., Henretty, K., Tzeng, J., & Gilbert, M. (2022). Addiction treatment and telehealth: Review of efficacy and provider insights during the COVID-19 pandemic. Psychiatric Services, 73(5), 484–491. https://doi.org/10.1176/appi.ps.202100088
Marlatt, G. A., & Donovan, D. M. (Eds.). (2005). Relapse prevention: Maintenance strategies in the treatment of addictive behaviors. Guilford.
May, R. K., Whelan, J. P., Steenbergh, T. A., & Meyers, A. W. (2003). The gambling self-efficacy questionnaire: An initial psychometric evaluation. Journal of Gambling Studies, 19(4), 339–357. https://doi.org/10.1023/A:1026379125116
McLaughlin, K. A., Koenen, K. C., Friedman, M. J., Ruscio, A. M., Karam, E. G., Shahly, V., & Kessler, R. C. (2015). Subthreshold posttraumatic stress disorder in the world health organization world mental health surveys. Biological Psychiatry, 77(4), 375–384. https://doi.org/10.1016/j.biopsych.2014.03.028.
McLellan, A. T. (1989). Treatment services review. VA Medical Center & University of Pennsylvania.
Miller, W. R., & Rollnick, S. (1991). Motivational interviewing: Preparing people to change addictive behavior. Guilford.
Monaghesh, E., & Hajizadeh, A. (2020). The role of telehealth during COVID-19 outbreak: A systematic review based on current evidence. BMC Public Health, 20(1), 1–9. https://doi.org/10.1186/s12889-020-09301-4
Moore, L.H., & Grubbs, J.B. (2021). Gambling disorder and comorbid PTSD: A systematic review of empirical research. Addictive Behaviors, 114, 106713, Doi: https://doi.org/10.1016/j.addbeh.2020.106713.
Najavits, L. M. (2002). Seeking safety: A treatment manual for PTSD and substance abuse. The Guilford Press.
Najavits, L. M. (2009). Seeking safety : An implementation guide. In A. Rubin, D. W. Springer (Eds.) The clinician's guide to evidence-based practice. Hoboken, NJ: Wiley.
Najavits, L. M. (2011). Treatments for PTSD and pathological gambling: What do patients want? Journal of Gambling Studies, 27(2), 229–241. https://doi.org/10.1007/s10899-010-9198-9
Najavits, L. M., Clark, H. W., DiClemente, C. C., Potenza, M. N., Shaffer, H. J., Sorensen, J. L., & Zweben, J. E. (2020). PTSD/substance use disorder comorbidity: Treatment options and public health needs. Current Treatment Options in Psychiatry, 7(4), 544–558. https://doi.org/10.1007/s40501-020-00234-8
Najavits, L. M., Hamilton, N., Miller, N., Griffin, J., Welsh, T., & Vargo, M. (2014). Peer-led seeking safety: Results of a pilot outcome study with relevance to public health. Journal of Psychoactive Drugs, 46(4), 295–302. https://doi.org/10.1080/02791072.2014.922227
Najavits, L. M., & Hien, D. (2013). Helping vulnerable populations: A comprehensive review of the treatment outcome literature on substance use disorder and PTSD. Journal of Clinical Psychology, 69(5), 433–479. https://doi.org/10.1002/jclp.21980
Najavits, L. M., & Liese, B. S. (2003). Seeking safety adherence scale (version 3). Unpublished measure. Boston, MA : Harvard Medical School/McLean Hospital.
Najavits, L. M., Smylie, D., Johnson, K., Lung, J., Gallop, R. J., & Classen, C. C. (2013). Seeking safety therapy for pathological gambling and PTSD: A pilot outcome study. Journal of Psychoactive Drugs, 45(1), 10–16. https://doi.org/10.1080/02791072.2013.763557
Peltzer, K., Mabilu, M. G., Mathoho, S. F., Nekhwevha, A. P., Sikhwivhilu, T., & Sinthumule, T. S. (2006). Trauma history and severity of gambling involvement among horse-race gamblers in a South African gambling setting. Psychological Reports, 99(2), 472–476. https://doi.org/10.2466/pr0.99.2.472-476
Petry, N. M., Ammerman, Y., Bohl, J., Doersch, A., Gay, H., Kadden, R., Molina, C., & Steinberg, K. (2006). Cognitive-behavioral therapy for pathological gamblers. Journal of Consulting and Clinical Psychology, 74(3), 555–567. https://doi.org/10.1037/0022-006X.74.3.555
Petry, N. M., Ginley, M. K., & Rash, C. J. (2017). A systematic review of treatments for problem gambling. Psychology of Addictive Behaviors, 31(8), 951–961. https://doi.org/10.1037/adb0000290
Petry, N. M., & Steinberg, K. L. (2005). Childhood maltreatment in male and female treatment-seeking pathological gamblers. Psychology of Addictive Behaviors, 19(2), 226. https://doi.org/10.1037/0893-164X.19.2.226
Petry, N. M., Stinson, F. S., & Grant, B. F. (2005). Comorbidity of DSM-IV pathological gambling and other psychiatric disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry, 66(5), 564–574. https://doi.org/10.4088/jcp.v66n0504
Poole, J. C., Kim, H. S., Dobson, K. S., & Hodgins, D. C. (2017). Adverse childhood experiences and disordered gambling: Assessing the mediating role of emotion dysregulation. Journal of Gambling Studies, 33(4), 1187–1200. https://doi.org/10.1007/s10899-017-9680-8
Scherrer, J. F., Xian, H., Kapp, J. M. K., Waterman, B., Shah, K. R., Volberg, R., & Eisen, S. A. (2007). Association between exposure to childhood and lifetime traumatic events and lifetime pathological gambling in a twin cohort. The Journal of Nervous and Mental Disease, 195(1), 72–78. https://doi.org/10.1097/01.nmd.0000252384.20382.e9
Smith, D. P., Battersby, M. W., Harvey, P. W., Pols, R. G., & Ladouceur, R. (2011). Cognitive and behavioural session analysis/integrity check. Flinders University.
Smith, D. P., Battersby, M. W., Harvey, P. W., Pols, R. G., & Ladouceur, R. (2013). Two-group randomised, parallel trial of cognitive and exposure therapies for problem gambling: A research protocol. BMJ Open, 3(6), e003244. https://doi.org/10.1136/bmjopen-2013-003244.
Steenbergh, T. A., Meyers, A. W., May, R. K., & Whelan, J. P. (2002). Development and validation of the Gamblers’ Beliefs Questionnaire. Psychology of Addictive Behaviors, 16(2), 143–149. https://doi.org/10.1037/0893-164X.16.2.143
Sylvain, C., Ladouceur, R., & Boisvert, J.-M. (1997). Cognitive and behavioral treatment of pathological gambling: A controlled study. Journal of Consulting and Clinical Psychology, 65(5), 727–732. https://doi.org/10.1037/0022-006X.65.5.727
Taber, J. I., McCormick, R. A., & Ramirez, L. F. (1987). The prevalence and impact of major life stressors among pathological gamblers. International Journal of the Addictions, 22(1), 71–79. https://doi.org/10.3109/10826088709027414
Tobin, D. L., Holroyd, K. A., Reynolds, R. V., & Wigal, J. K. (1989). The hierarchical factor structure of the Coping Strategies Inventory. Cognitive Therapy and Research, 13(4), 343–361. https://doi.org/10.1007/BF01173478
Torchalla, I., Nosen, L., Rostam, H., & Allen, P. (2012). Integrated treatment programs for individuals with concurrent substance use disorders and trauma experiences: A systematic review and meta-analysis. Journal of Substance Abuse Treatment, 42(1), 65–77. https://doi.org/10.1016/j.jsat.2011.09.001
Tse, S., Campbell, L., Rossen, F., Wang, C.-W., Jull, A., Yan, E., & Jackson, A. (2013). Face-to-face and telephone counseling for problem gambling: A pracmatic multisite randomized study. Research on Social Work Practice, 23, 57–65. https://doi.org/10.1177/1049731512466150
Walker, M., Toneatto, T., Potenza, M. N., Petry, N., Ladouceur, R., Hodgins, D. C., & Blaszczynski, A. (2006). A framework for reporting outcomes in problem gambling treatment research: The Banff, Alberta Consensus. Addiction, 101(4), 504–511. https://doi.org/10.1111/j.1360-0443.2005.01341.x.
Watson, J. C., Lenz, A. S., Schmit, M. K., & Schmit, E. L. (2016). Calculating and reporting estimates of effect size in counseling outcome research. Counseling Outcome Research and Evaluation, 7(2), 111–123. https://doi.org/10.1177/2150137816660584
Weathers, F. W., Blake, D. D., Schnurr, P. P., Kaloupek, D. G., Marx, B. P., & Keane, T. M. (2013a). The clinician-administered PTSD Scale for DSM-5 (CAPS-5): Past-month version. National Center for PTSD, Veterans Affairs Boston Healthcare System.
Weathers, F. W., Litz, B. T., Keane, T. M., Palmieri, P. A., Marx, B. P., & Schnurr, P. P. (2013b). The ptsd checklist for dsm-5 (pcl-5). Scale available from the National Center for PTSD at www. ptsd. va. gov, 10(4), 206.
Winters, K. C., Specker, S., & Stinchfield, R. D. (2002). Diagnostic Interview for gambling severity-revised (DIGS-R). University of Minnesota Medical School.
Acknowledgements
We warmly thank the study therapists (Marsha Harris; Debra Kostyk, MSW, RSW; Melissa Muir; and Kathie Neufeld), as well as our research assistants (Marisa Morrill and Gabriel Logounov); and Dr. Robert Ladouceur (the developer of CBT for PG).
Funding
This research was funded by the Manitoba Gambling Research Program of Manitoba Liquor and Lotteries; however, the findings and conclusions of this paper are those solely of the authors and do not necessarily represent the views of Manitoba Liquor and Lotteries. Dr. Tracie O. Afifi is supported by a Tier I Canada Research Chair in Childhood Adversity and Resilience.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Lisa Najavits is the author of Seeking Safety and director of Treatment Innovations, which provides training on the model. Drs. Ledgerwood and Afifi have nothing to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Najavits, L.M., Ledgerwood, D.M. & Afifi, T.O. A Randomized Controlled Trial for Gambling Disorder and PTSD: Seeking Safety and CBT. J Gambl Stud 39, 1865–1884 (2023). https://doi.org/10.1007/s10899-023-10224-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10899-023-10224-z