Abstract
Purpose
Surgical approach to rectal cancer has evolved in recent decades, with introduction of minimally invasive surgery (MIS) techniques and local excision. Since implementation might differ internationally, this study is aimed at evaluating trends in surgical approach to rectal cancer across different countries over the last 10 years and to gain insight into patient, tumour and treatment characteristics.
Methods
Pseudo-anonymised data of patients undergoing resection for rectal cancer between 2010 and 2019 were extracted from clinical audits in the Netherlands (NL), Sweden (SE), England-Wales (EW) and Australia-New Zealand (AZ).
Results
Ninety-nine thousand five hundred ninety-seven patients were included (38,413 open, 55,155 MIS and 5416 local excision). An overall increase in MIS was observed from 29.9% in 2010 to 72.1% in 2019, with decreasing conversion rates (17.5–9.0%). The MIS proportion was highly variable between countries in the period 2010–2014 (54.4% NL, 45.3% EW, 39.8% AZ, 14.1% SE, P < 0.001), but variation reduced over time (2015–2019 78.8% NL, 66.3% EW, 64.3% AZ, 53.2% SE, P < 0.001). The proportion of local excision for the two periods was highly variable between countries: 4.7% and 11.8% in NL, 3.9% and 7.4% in EW, 4.7% and 4.6% in AZ, 6.0% and 2.9% in SE.
Conclusions
Application and speed of implementation of MIS were highly variable between countries, but each registry demonstrated a significant increase over time. Local excision revealed inconsistent trends over time.
Similar content being viewed by others
Introduction
The operative approach to rectal cancer has continued to evolve over the past decade, with reduction of invasiveness of surgery whilst maintaining oncological quality [1]. Although there was a rapid adoption of laparoscopic surgery for colon cancer following the publication of the COST study [2] and other trials, minimally invasive surgery (MIS) for rectal cancer has been more controversial. A number of randomized trials have compared a laparoscopic approach to open surgery in rectal cancer. Whilst the COLOR II trial [3] showed benefits in terms of recovery and equivalent oncological outcomes, ALaCaRT [4] and ACOSOG Z6051 [5] failed to demonstrate non-inferiority in pathological outcomes for T1–T3 and stage II and III rectal tumours, although 2-year oncological outcomes were comparable [6, 7]. Ongoing efforts have focused on refining MIS for surgical resection of especially low rectal tumours. This led to the introduction of transanal total mesorectal excision in 2010 [8, 9] and robot-assisted laparoscopic surgery in 2001 [10]. Adoption of new technology has occurred at differing paces internationally, based on local health economic and surgical factors. Evaluation of the adoption of minimally invasive surgery is important to understand the current variability in health technology usage and to plan future studies evaluating the impact on patient outcomes.
Implementation of new techniques and quality of care is currently monitored by clinical audits at a national level. The Dutch ColoRectal Audit (DCRA) in the Netherlands, Swedish ColoRectal Cancer Registry (SCRCR) in Sweden, National Bowel Cancer Audit (NBOCA) in England and Wales and the Bowel Cancer Outcomes Registry (BCOR) in Australia and New Zealand are four clinical audits that provide valuable information on new treatment strategies and measure quality of care [11,12,13,14]. Combining these data can provide insights into variability in colorectal cancer care internationally, such as uptake of new techniques and treatment approaches [15, 16]. International benchmarking will allow evaluation of national performance and may identify areas for potential further improvement [17]. This study is part of an international collaboration between colorectal registries that supports (inter)national learning, improving and harmonisation.
The aim of this study is to evaluate the surgical approach applied to rectal cancer based on four national registries over the last 10 years and to gain more insight into patient, tumour and treatment characteristics at an international level.
Material and methods
This international retrospective population-based cohort study obtained pseudo-anonymised data from the DCRA, SCRCR, NBOCA and BCOR. All patients (n = 99,597) undergoing rectal cancer surgery from January 1, 2010, and December 31, 2019, were extracted from the registries. Each individual registry extracted their data from their own local registry under their own existing ethical framework, and only pseudo-anonymised data were shared internationally. No additional ethical approval or informed consent was required for this study.
ICORC
International Colorectal Cancer Registry Collaboration (ICORC) is an international collaborative aiming to improve colorectal cancer care globally by, among other things, agreeing on a minimum dataset with common definitions across registries and comparing care and outcomes internationally. The included registries in this study were founders of ICORC in 2021.
Dutch colorectal audit
The DCRA is a national clinical audit in the Netherlands that is mandatory and registers multidisciplinary data from all colorectal cancer patients who undergo surgery. The registration reports high validity of data with completeness of > 95% during the entire study period [11]. Local excisions are only registered as separate surgical approach since 2012.
Swedish colorectal cancer registry
All patients diagnosed with colorectal cancer in Sweden are registered in the mandatory SCRCR, which includes surgical as well as oncological and diagnostic elements. Data completeness is > 98% with high validity in the entire study period [18].
National bowel cancer audit
In NBOCA, multidisciplinary data from all colorectal cancer patients in England and Wales are mandatorily collected. It had a national coverage of 90–95% during the study period.
Bowel cancer outcomes registry
The BCOR records surgical outcomes for colorectal cancer patients in Australia and New Zealand [12]. It is a voluntary audit which includes over 48,000 patients since 2007. Coverage for all colorectal cancer patients was around 35% during the study period.
Data extraction
Local investigators from each registry collected the following variables: patient and disease characteristics, surgical and treatment characteristics and postoperative pathology. Surgical approach was categorised into open, MIS and local excision (including local excision followed by completion surgery). MIS includes conventional laparoscopic, robotic, hybrid and transanal approaches. We were not able to separately analyse the different MIS techniques between the countries due to availability of required variables in the datasets. Conversion was defined as conversion from MIS to open surgery. Conversion proportions were calculated with MIS patients as the denominator. BMI was classified into < 18.5, 18.5–30 and ≥ 30 kg/m2, and age into < 70 years and ≥ 70 years. American Association of Anesthesiologists (ASA) score and Charlson Comorbidity Index (CCI) were categorised as 1–2 and > 2 [19]. Neoadjuvant radiotherapy was classified into no radiotherapy, short-course radiotherapy (SCRT), chemoradiotherapy (CRT) and other radiotherapy schemes. Missing data were handled with use of missing categories, which were excluded from analysis.
Outcome parameters and time periods
Primary outcomes were surgical approach across different countries over years. Preoperative, tumour and treatment characteristics were compared between countries and within two time periods; year of surgery January 1, 2010, to December 31, 2014, and January 1, 2015, to December 31, 2019.
Statistical analyses
Local investigators of each registry reported all characteristics in absolute numbers with percentages for the two time periods. Clear definitions and an R-script were provided to harmonise local analysis. One investigator (JMLS) combined the aggregated results from each country to compare the categorical or dichotomous outcomes by time period with Pearson Chi-square or Fisher’s exact test. Statistical significance was defined as a P value of less than 0.01. For all statistical analyses, R studio version 4.2.1 (2022) was used.
Results
A total of 99,597 patients that underwent rectal cancer surgery between January 1, 2010, and December 31, 2019, were included in this study; 27,545 from the Netherlands, 48,304 from England and Wales, 9483 from Australia and New Zealand and 14,265 from Sweden (Fig. 1).
Preoperative patient characteristics
Preoperative patient characteristics are presented in Table 1. Registered patients undergoing rectal cancer surgery had the highest proportion of age < 70 years in Australia and New Zealand in both time periods (59.6% in 2010–2014 and 59.7% in 2015–2019) and the lowest proportion in Sweden (50.9% and 48.1%, respectively). Around 64% of patients were male, which was relatively constant over time and between countries. BMI was substantially different between countries and increased over time, most prominently in Australia-New Zealand. Concerning clinical staging in 2010–2014, England and Wales and Australia and New Zealand showed high percentages of unknown cT category (26.7% and 58.3%) compared to the Netherlands and Sweden (8.8% and 7.7%). Registration of cT category improved over time in all four countries, and differences decreased.
Pathological tumour characteristics
The percentage of (y)pT0-1 tumours in 2010–2014 was 41.2% in patients registered in Australia and New Zealand, which was substantially higher compared to the other three countries (15.7% in the Netherlands, 14.5% in England and Wales and 13.0% in Sweden; P < 0.001). This may reflect the lower percentage of national coverage of the registry or a true difference in disease pattern. This proportion increased to 23.0% in the Netherlands in 2015–2019 and remained stable in other countries (England-Wales 15.0%, Australia-New Zealand 44.0%, Sweden 13.8%, P < 0.001). Positive nodal staging was observed in 33.2% in the Netherlands, 31.2% in England and Wales, 33.0% in Australia and New Zealand and 37.7% in Sweden (P < 0.001) in 2010–2014 (Table 2). This remained stable in the second time period. The percentage of registered patients who had synchronous metastatic disease was 8.4% in the Netherlands, 8.0% in England and Wales, 12.0% in Australia and New Zealand and 8.1% in Sweden (P < 0.001), and this proportion slightly decreased in all countries in 2015–2019.
Treatment characteristics
Details on neoadjuvant radiotherapy and surgical characteristics are displayed in Table 2. Concerning radiotherapy, in 2010–2014, SCRT was administered to 41.0% of patients registered in the Netherlands and 46.7% in Sweden, but only 11.5% in England and Wales and 7.6% in Australia and New Zealand (P < 0.001). This decreased to 23.6% in the Netherlands and 6.5% in England and Wales in the period 2015–2019 and remained stable in Sweden (46.1%) and Australia and New Zealand (7.0%, P < 0.001). The proportion of patients treated with neoadjuvant CRT in the two time periods was 32.2% and 31.2% in the Netherlands, 23.6% and 24.4% in England and Wales, 34.7% and 41.1% in Australia and New Zealand and 15.2% and 13.1% in Sweden. During surgery, an anastomosis was formed in 61.9% in England and Wales in 2010–2014, compared to 48.6% in both the Netherlands and Sweden (P < 0.001). In the same period, any type of stoma was created in each of the countries in 84.1%, 78.3%, 79.6% and 85.5% (P < 0.001). In 2015–2019, the most remarkable changes were observed in the Netherlands with an increase in the proportion of anastomosis (from 48.6 to 63.5%) combined with a decrease in stoma rate (from 79.6 to 59.8%), whilst these proportions remained similar in the three other countries.
Surgical approach
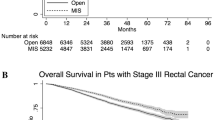
The surgical approach was open in 38,413 (38.8%), MIS in 55,155 (55.7%) and local excision in 5416 patients (5.5%). Overall conversion proportion from MIS was 12.3% (6759 out of 55,155 MIS patients).
There was an overall decrease in patients treated with an open approach from 66.8% in 2010 to 20.7% in 2019, in favour of MIS which increased from 29.9% to 72.1 (Fig. 2a). Conversion rate decreased from 17.5 to 9.0%. The number of patients treated with a surgical local excision, with or without complete rectal resection, doubled over the years (3.3% in 2010, 7.2% 2019).
There were significant differences in the speed of implementation of MIS between registered patients in different countries (Fig. 2b). Based on steeper curves, implementation started later in Sweden and was faster in Sweden and the Netherlands compared to England and Wales and Australia and New Zealand. The percentage of patients treated with MIS increased in all countries but at variable levels. In the Netherlands, MIS increased from 38.0% in 2010 to 80.3% in 2019, with predominance of MIS since 2012, and a plateau phase since 2016 (Table 3). The implementation of MIS in registered patients progressed similarly in England and Wales and Australia and New Zealand (33.3 to 70.4% and 30.1 to 73.0%), with predominance of MIS since 2013 and 2015; however, a plateau phase was not yet identified (Fig. 2 and Table 3). In Sweden, only 6.0% of patients were treated with MIS in 2010, with a predominance of MIS since 2017, and the proportion of MIS increased to 65.2% in 2019.
The conversion rate of MIS varied between countries from 10.1 to 19.8% in the period 2010–2014 and from 6.8 to 12.7% in the period 2015–2019. Conversion rates decreased over time in all countries. Change in use of local excisions was also highly variable between countries; this increased from 4.7 to 11.8% in the Netherlands and from 3.9 to 7.4% in England and Wales, remained stable in Australia and New Zealand (4.7 to 4.6%) and decreased from 6.0 to 2.9% in Sweden in the period 2010–2019.
Discussion
This international cohort study based on data from four colorectal cancer registries comprising nearly 100,000 patients provides insight in the evolution of surgical approach for rectal cancer resection, together with patient, tumour and treatment characteristics of these rectal cancer populations between 2010 and 2019. Some remarkable differences in patient characteristics and neoadjuvant therapy were observed between countries. The implementation of MIS has increased in all countries over time to an overall proportion of 72.1% in 2019. There were, however, significant differences in the implementation speed of MIS across countries. A predominance in using MIS for rectal cancer was reached in 2012 in the Netherlands, 2013 in England and Wales, 2015 in Australia and New Zealand and 2017 in Sweden. The implementation speed in Sweden and the Netherlands was faster compared to England and Wales and Australia and New Zealand, though implementation started later in Sweden. Also change in use of local excisions was highly variable between countries, and Sweden was the only country with a registered decrease in the application of local excision.
The present study shows that the conversion rate decreased from 17.5% in 2010 to 9.0% in 2019. This likely reflects more experience with MIS among colorectal surgeons, as conversion is often considered an assessment tool for MIS learning curve [20]. Unfortunately, clinical outcomes could not be evaluated in the present study, due to the fact that not all the national registries allow us to share outcome data for comparative analyses at an international level. However, multiple randomized controlled trials have demonstrated comparable intraoperative complication rates and postoperative morbidity and mortality for MIS and open surgery [3, 4, 6, 21,22,23]. Phase IV studies have shown even better postoperative outcomes of MIS at a population level [24]. In addition, MIS is associated with less long-term surgical complications such as incisional hernia and adhesion-related small bowel obstruction, especially if conversion rates are low [25]. Therefore, we should interpret the observed increase in application of MIS with decreasing conversion rates among the four analysed registries as an important gain in quality of care.
The speed and degree of implementation of MIS is influenced by many factors. The necessary equipment must become available, which needs initial investments with re-allocation of budgets. This might have been a problem at the time as there was still doubt about the additional value of MIS over open surgery, with ongoing debates between early and late adopters during surgical congresses in the early years of the study period. Furthermore, there needs to be an infrastructure for training and proctoring of the surgeons in order to guarantee safe implementation [26,27,28]. Also, institutional volumes might have a significant impact, as sufficient case load is needed to complete the learning curve in a timely manner. Having a low volume might even be the reason not to implement new techniques at all. Case volumes might substantially vary within countries, as well as between countries, related to characteristics of the health care system and geographical factors.
Case selection might also influence speed of implementation, which might be more relevant in rectal cancer as compared to colon cancer. The deeper part of the pelvis adds to the technical challenges during laparoscopy, and alternative MIS techniques have therefore been introduced for rectal procedures. Transanal approach was developed to improve oncological and functional outcomes for mid or low-rectal cancer, with comparable intraoperative and postoperative morbidity and conversion rates compared to laparoscopy as concluded in a systematic review and meta-analysis [29]. Robot surgery is considered of value in complex colorectal cancer and has the advantage of a shorter learning curve compared to conventional laparoscopy with ergonomic advantages for the surgeon, although costs are higher [20, 30, 31]. A recent study suggests that robotic surgery might facilitate implementation of MIS at a national level [16]. Access to robotic surgery is increasing rapidly and likely to continue to increase as a proportion of rectal cancer surgery.
Besides an increase in MIS, the proportion of patients treated with a surgical local excision has also doubled overall to 7.2% in 2019. This technique is considered safe for early rectal cancers without histological risk factors [32, 33] and might also be used for small residual lesions after neo-adjuvant radiotherapy. The implementation has been variable between countries, which is likely due to multiple factors including stage distribution (e.g., influenced by national screening programmes), availability of equipment (transanal MIS platforms), surgeons with specific expertise and dedicated multidisciplinary teams with focus on rectal preserving treatment strategies and patient preferences [34].
Although this is beyond the scope of the present study, we also observed substantial differences in the utilisation of neoadjuvant radiotherapy. A substantial reduction in short-course radiotherapy was observed in the Netherlands, aligned with national guideline changes [24], whilst such a reduction was not found for Sweden. In England and Wales, a minority of patients received radiotherapy in 2010–2014, which further decreased thereafter. In Australia-New Zealand, a stable proportion of about 50% of patients received neoadjuvant radiotherapy, mostly chemoradiotherapy. Local guidelines might be an explanation for these differences. There was no data available on application of total neoadjuvant therapy.
The number of patients included in the study from different countries is highly variable, which is partly due to different population sizes. However, only three of the included countries have a mandatory audit with national coverage, whereas the BCOR in Australia and New Zealand is a voluntary audit which might cause registration bias. This might also explain the difference in age distribution and tumour stage in Australia and New Zealand, which included younger patients with lower tumour stages. Different proportions of unknown clinical staging were observed in our study, which could imply registration problems or differences in methods of preoperative clinical staging between countries.
There is still a lack of consensus on the definition of rectal cancer internationally. A range of definitions for rectum and the rectosigmoid junction are used [35, 36]. Australia and New Zealand define rectal cancer as cancer that clinically, radiologically, or endoscopically is considered to be located in the rectum below the rectosigmoid junction, equal to or less than 15 cm from the anal verge on rigid endoscopy. In England and Wales and Sweden, the definition of rectal cancer is a tumour within 15 cm from the anal verge on rigid endoscopy. This method has several problems which include most patients currently being diagnosed with flexible scopes and patient variation in anal and rectal anatomy. In the Netherlands, the sigmoid take-off has been implemented since 2019 to define rectal cancer based on imaging, following an international Delphi consensus [37]. International harmonisation of the definition of rectal cancer would improve the reliability of comparative analyses of rectal cancer registries.
The current study has certain limitations due to its design. Most importantly, no information was available on outcome parameters to make a comparison between effectiveness of surgical approaches possible. Also, some characteristic had missing values, such as BMI, ASA, CCI, neoadjuvant radiotherapy and surgical approach. Data analysis was performed in each registry to an aggregated level and later combined for statistical analysis. Although clear definitions and an R-script were provided to harmonise local analysis, a linked database would be of added value. Furthermore, the information on how the registry data was collected was beyond the scope of the manuscript. Future research and collaboration are ongoing and will elaborate on this.
Conclusion
The proportion of MIS as a surgical approach to rectal cancer increased over a decade at an international level, with a decreasing number of open resections and conversion rates. There was however inter-national variability in the implementation speed and proportion of MIS during the entire study period. Implementation of local excisions was also highly variable between countries.
Data availability
Data will be made available on reasonable request.
Change history
08 February 2024
A Correction to this paper has been published: https://doi.org/10.1007/s00384-024-04599-7
References
Ryan OK, Ryan ÉJ, Creavin B, Rausa E, Kelly ME, Petrelli F et al (2021) Surgical approach for rectal cancer: a network meta-analysis comparing open, laparoscopic, robotic and transanal TME approaches. Eur J Surg Oncol 47(2):285–295
Mathew G, Agha R, Albrecht J, Goel P, Mukherjee I, Pai P et al (2021) STROCSS 2021: strengthening the reporting of cohort, cross-sectional and case-control studies in surgery. Int J Surg 96:106165
Bonjer HJ, Deijen CL, Abis GA, Cuesta MA, van der Pas MH, de Lange-de Klerk ES et al (2015) A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med 372(14):1324–1332
Stevenson AR, Solomon MJ, Lumley JW, Hewett P, Clouston AD, Gebski VJ et al (2015) Effect of laparoscopic-assisted resection vs open resection on pathological outcomes in rectal cancer: the ALaCaRT randomized clinical trial. JAMA 314(13):1356–1363
Fleshman J, Branda M, Sargent DJ, Boller AM, George V, Abbas M et al (2015) Effect of laparoscopic-assisted resection vs open resection of stage II or III rectal cancer on pathologic outcomes: the ACOSOG Z6051 randomized clinical trial. JAMA 314(13):1346–1355
Stevenson ARL, Solomon MJ, Brown CSB, Lumley JW, Hewett P, Clouston AD et al (2019) Disease-free survival and local recurrence after laparoscopic-assisted resection or open resection for rectal cancer: the Australasian laparoscopic cancer of the rectum randomized clinical trial. Ann Surg 269(4):596–602
Fleshman J, Branda ME, Sargent DJ, Boller AM, George VV, Abbas MA et al (2019) Disease-free survival and local recurrence for laparoscopic resection compared with open resection of stage II to III rectal cancer: follow-up results of the ACOSOG Z6051 randomized controlled trial. Ann Surg 269(4):589–595
Wasmuth HH, Faerden AE, Myklebust T, Pfeffer F, Norderval S, Riis R et al (2020) Transanal total mesorectal excision for rectal cancer has been suspended in Norway. Br J Surg 107(1):121–130
Roodbeen SX, Penna M, van Dieren S, Moran B, Tekkis P, Tanis PJ, Hompes R (2021) Local recurrence and disease-free survival after transanal total mesorectal excision: results from the international TaTME registry. J Natl Compr Canc Netw 19(11):1232–1240
Jayne D, Pigazzi A, Marshall H, Croft J, Corrigan N, Copeland J et al (2017) Effect of robotic-assisted vs conventional laparoscopic surgery on risk of conversion to open laparotomy among patients undergoing resection for rectal cancer: the ROLARR randomized clinical trial. JAMA 318(16):1569–1580
Van Leersum NJ, Snijders HS, Henneman D, Kolfschoten NE, Gooiker GA, ten Berge MG et al (2013) The Dutch surgical colorectal audit. Eur J Surg Oncol 39(10):1063–1070
Hunter RA, Moore J (2016) Evolution of the Bi-National Colorectal Cancer Audit: history, governance and future directions. ANZ J Surg 86(6):431–432
Kodeda K, Nathanaelsson L, Jung B, Olsson H, Jestin P, Sjövall A et al (2013) Population-based data from the Swedish colon cancer registry. Br J Surg 100(8):1100–1107
NBOCA (2022) National bowel cancer audit annual report 2022. Available from: https://www.nboca.org.uk/content/uploads/2023/01/NBOCA-2022-Final.pdf
Detering R, Saraste D, de Neree Tot Babberich MPM, Dekker JWT, Wouters M, van Geloven AAW et al (2020) International evaluation of circumferential resection margins after rectal cancer resection: insights from the Swedish and Dutch audits. Colorectal Dis 22(4):416–29
Warps AK, Saraste D, Westerterp M, Detering R, Sjövall A, Martling A et al (2022) National differences in implementation of minimally invasive surgery for colorectal cancer and the influence on short-term outcomes. Surg Endosc 36(8):5986–6001
van de Velde CJ, Boelens PG, Borras JM, Coebergh JW, Cervantes A, Blomqvist L et al (2014) EURECCA colorectal: multidisciplinary management: European consensus conference colon & rectum. Eur J Cancer 50(1):1.e-.e34
Moberger P, Sköldberg F, Birgisson H (2018) Evaluation of the Swedish Colorectal Cancer Registry: an overview of completeness, timeliness, comparability and validity. Acta Oncol 57(12):1611–1621
Armitage JN, van der Meulen JH (2010) Identifying co-morbidity in surgical patients using administrative data with the Royal College of Surgeons Charlson Score. Br J Surg 97(5):772–781
Barrie J, Jayne DG, Wright J, Murray CJ, Collinson FJ, Pavitt SH (2014) Attaining surgical competency and its implications in surgical clinical trial design: a systematic review of the learning curve in laparoscopic and robot-assisted laparoscopic colorectal cancer surgery. Ann Surg Oncol 21(3):829–840
van der Pas MH, Haglind E, Cuesta MA, Fürst A, Lacy AM, Hop WC, Bonjer HJ (2013) Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol 14(3):210–218
Kang SB, Park JW, Jeong SY, Nam BH, Choi HS, Kim DW et al (2010) Open versus laparoscopic surgery for mid or low rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): short-term outcomes of an open-label randomised controlled trial. Lancet Oncol 11(7):637–645
Fleshman J, Sargent DJ, Green E, Anvari M, Stryker SJ, Beart RW Jr et al (2007) Laparoscopic colectomy for cancer is not inferior to open surgery based on 5-year data from the COST Study Group trial. Ann Surg 246(4):655–62; discussion 62–4
Gietelink L, Wouters M, Marijnen CAM, van Groningen J, van Leersum N, Beets-Tan RGH et al (2017) Changes in nationwide use of preoperative radiotherapy for rectal cancer after revision of the national colorectal cancer guideline. Eur J Surg Oncol 43(7):1297–1303
Pecorelli N, Greco M, Amodeo S, Braga M (2017) Small bowel obstruction and incisional hernia after laparoscopic and open colorectal surgery: a meta-analysis of comparative trials. Surg Endosc 31(1):85–99
Bosker R, Groen H, Hoff C, Totte E, Ploeg R, Pierie JP (2011) Effect of proctoring on implementation and results of elective laparoscopic colon surgery. Int J Colorectal Dis 26(7):941–947
Mackenzie H, Cuming T, Miskovic D, Wyles SM, Langsford L, Anderson J et al (2015) Design, delivery, and validation of a trainer curriculum for the national laparoscopic colorectal training program in England. Ann Surg 261(1):149–156
Hanna GB, Mackenzie H, Miskovic D, Ni M, Wyles S, Aylin P et al (2022) Laparoscopic colorectal surgery outcomes improved after national training program (LAPCO) for specialists in England. Ann Surg 275(6):1149–1155
Simillis C, Lal N, Thoukididou SN, Kontovounisios C, Smith JJ, Hompes R et al (2019) Open versus laparoscopic versus robotic versus transanal mesorectal excision for rectal cancer: a systematic review and network meta-analysis. Ann Surg 270(1):59–68
Ngu JC, Kim SH (2019) Robotic surgery in colorectal cancer: the way forward or a passing fad. J Gastrointest Oncol 10(6):1222–1228
Odermatt M, Ahmed J, Panteleimonitis S, Khan J, Parvaiz A (2017) Prior experience in laparoscopic rectal surgery can minimise the learning curve for robotic rectal resections: a cumulative sum analysis. Surg Endosc 31(10):4067–4076
Chiniah M, Ganganah O, Cheng Y, Sah SK (2016) Transanal endoscopic microsurgery is an oncologically safe alternative to total mesorectal excision for stage I rectal cancer: results of a meta-analysis of randomized controlled trials. Int J Colorectal Dis 31(8):1501–1504
Kidane B, Chadi SA, Kanters S, Colquhoun PH, Ott MC (2015) Local resection compared with radical resection in the treatment of T1N0M0 rectal adenocarcinoma: a systematic review and meta-analysis. Dis Colon Rectum 58(1):122–140
Bach SP (2022) Can we Save the rectum by watchful waiting or TransAnal surgery following (chemo)Radiotherapy versus Total mesorectal excision for early REctal Cancer (STAR-TREC)? Protocol for the international, multicentre, rolling phase II/III partially randomized patient preference trial evaluating long-course concurrent chemoradiotherapy versus short-course radiotherapy organ preservation approaches. Colorectal Dis 24(5):639–651
D’Souza N,de Neree Tot Babberich MPM, Lord A, Shaw A, Abulafi M, Tekkis P et al (2018) The rectosigmoid problem. Surg Oncol 27(3):521–525
Massalou D, Moszkowicz D, Mariage D, Baqué P, Camuzard O, Bronsard N (2018) Is it possible to give a single definition of the rectosigmoid junction? Surg Radiol Anat 40(4):431–438
DʼSouza N, de Neree Tot Babberich MPM, d'Hoore A, Tiret E, Xynos E, Beets-Tan RGH et al (2019) Definition of the rectum: an international, expert-based Delphi consensus. Ann Surg 270(6):955–9
Acknowledgements
List of ICORC Collaborators: Tarik Samour, Bowel Cancer Outcomes Registry (BCOR)—Australia and New Zealand; Hidde Kroon, Bowel Cancer Outcomes Registry (BCOR)—Australia and New Zealand; Sze-Lin Peng, Bowel Cancer Outcomes Registry (BCOR)—Australia and New Zealand; Neal Rawson, Queensland Health—Australia; Shoni Philpot, Queensland Health—Australia; Ian Hayes, Australian Comprehensive Cancer Outcomes and Research Database (ACCORD)—Australia; Lene Hjerrild Iversen, Danish Colorectal Cancer Group (DCCG)—Denmark; Jon Kroll Bjerregaard, Danish Colorectal Cancer Group (DCCG)—Denmark; Camilla Qvortrup, Danish Colorectal Cancer Group (DCCG)—Denmark; Ismail Gögenür, Danish Colorectal Cancer Group (DCCG)—Denmark; Richard Spence, Dalhousie University—Canada; Rob Tollenaar, Dutch ColoRectal Audit (DCRA)—the Netherlands; Roel Hompes, Dutch ColoRectal Audit (DCRA)—the Netherlands; Federico Ghignone, Italian Bower Cancer Outcome Registry—Italy; Helen Blake, National Bowel Cancer Audit (NBOCA)—United Kingdom; Nicola Fearnhead, National Bowel Cancer Audit (NBOCA)—United Kingdom; Jan van der Meulen, National Bowel Cancer Audit (NBOCA)—United Kingdom; Mike Braun, National Bowel Cancer Audit (NBOCA)—United Kingdom; Arne Wibe, Norwegian Colorectal Cancer registry—Norwegian; Janet Graham, West of Scotland Cancer Network (WoSCAN)—Scotland; Graham Mackay, NHS Greater Glasgow and Clyde (NHSGGC)—Scotland; David Morrison, Public Health Scotland—Scotland; Ingvar Syk, Swedish Colorectal Cancer Register (SCRCR) —Sweden; Clifford Ko, American College of Surgeons—United States of America; Nicolas Avellaneda, Argentina CRC registry—Argentina.
Author information
Authors and Affiliations
Consortia
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and statistical analysis were performed by Sijmons. The first draft of the manuscript was written by Sijmons, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Not required.
Informed consent
Not required.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: Under the collaborators the co-author's family name has been change from Samour to Sammour
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sijmons, J.M.L., Dekker, J.W.T., Tuynman, J.B. et al. Evolution of surgical approach to rectal cancer resection: A multinational registry assessment. Int J Colorectal Dis 39, 15 (2024). https://doi.org/10.1007/s00384-023-04578-4
Accepted:
Published:
DOI: https://doi.org/10.1007/s00384-023-04578-4