J.ophthalmol.(Ukraine).2022;5:19-22.
|
http://doi.org/10.31288/oftalmolzh202251922 Received: 24.06.2022; Accepted: 03.08.2022; Published on-line: 27.10.2022 Using a liposomal ozone-based solution in comprehensive treatment of bacterial keratitis V. M. Sakovych, O. V. Aleksieieva Dnipro State Medical University; Dnipro (Ukraine) TO CITE THIS ARTICLE: Sakovych VM, Aleksieieva OV. Using a liposomal ozone-based solution in comprehensive treatment of bacterial keratitis. J.ophthalmol.(Ukraine).2022;5:19-22. http://doi.org/10.31288/oftalmolzh202251922 Background: Keratitis is an inflammatory eye disease frequently leading to complications, significantly decreased vision and visual disability. Common infectious agents include, in particular, aggressive Gram-negative microflora and opportunistic bacteria. The use of conventional antibacterial therapy does not guarantee a positive treatment effect. Infections caused by antibiotic-resistant germs frequently result in increased hospitalization rates with an increased length of inpatient stay at hospital and can cause severe corneal opacities. Formation of biofilms is a cause of increased antibiotic resistance. Purpose: To improve the efficacy of treatment of bacterial keratitis by integrating an adjunctive liposomal ozone-based solution into comprehensive treatment. Material and Methods: Forty-four patients (44 eyes) with bacterial keratitis, aged from 29 to 75 years, were involved in the study. Patients were divided into an ozone group of 21 patients and a control group of 23 patients. All patients were administered antibacterial therapy, mydriatics, desensibilizing agents, tissue preparations and vitamins. In addition, patients of the ozone group received an eye drop of ozone-based solution four times a day for 10 days. Results: The method allowed for a significant (р < 0.001) reduction in conjunctival discharge, mixed conjunctival injection, corneal edema and inflammatory response, leeading to a 3.3 ± 0.1 day reduction in the length of inpatient stay at the hospital. Conclusion: Utilizing a liposomal ozone-based solution as an adjunct to the comprehensive treatment of bacterial keratitis is a novel treatment method making it possible to accelerate corneal epithelization and reduction in inflammation, and to shorten the length of treatment. Keywords: bacterial keratitis, liposomal ozone-based solution, comprehensive treatment, clinical scores
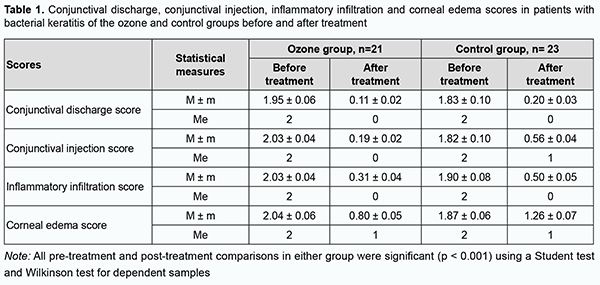
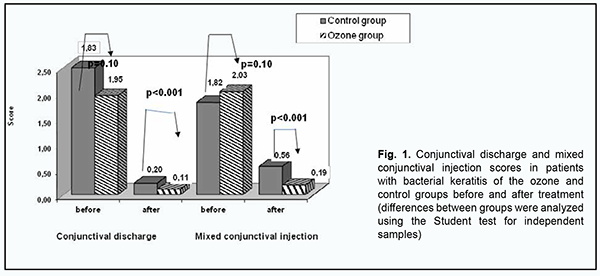
Introduction Corneal infectious agents include, in particular, aggressive Gram-negative microflora and opportunistic bacteria of genera Streptococcus, Staphylococcus, Escherichiae, Enterobacter, Proteus, Pseudomonas, Klebsiellae, etc. [1, 2]. Infectious and traumatic diseases of the cornea require adequate multifactorial therapy capable of protecting against infection and facilitating re-epithelization. Excessive use of antibiotics in the treatment of infections and wide use and inadequate dosage of antibiotics in agriculture and veterinary medicine have, over time, contributed to the emergence of resistant bacteria [3] which cause specific infections, particularly in the eye [4]. Bacterial resistance results in changes in bacteria. They acquire the capacity of surviving in hostile environment. Antibiotics kill sensitive bacteria, but not bacteria with resistance genes, and the progeny of the latter bacteria may quickly become dominant in the total bacterial population. If some bacteria in the infecting population contain an antibiotic resistance gene, they can transfer the gene to other bacteria in the population that are sensitive to the antibiotic. These bacteria that acquire the resistance genes also become resistant. Multiplication of resistant bacteria results in disease progression. Developing new antimicrobial means with a new mechanism of action is an important strategy for the fight against the threat of antibiotic resistance. Ozone is increasingly considered a treatment option for several types of infection [5]. Corneal inflammation represents a challenge in current ophthalmological practice due to various etiologies and the risk of infection and superinfection. The appearance of resistant and multi-resistant bacterial strains has urged researchers to investigate new antimicrobials able to cover a broad spectrum of microorganisms. Of these, liposomal ozonated oil has shown antiseptic and reparative properties and can be proposed for the prevention and treatment of acute and chronic local infections, as an alternative to topical antimicrobial agents, on account of its antibacterial, antifungal and antiviral properties [5-7]. Ozone is an unstable gaseous substance that facilitates tissue restoration, is not toxic for the epithelium, and decomposes into molecular oxygen. Ozonides produced in the reaction of ozone with fatty acids present in vegetable oils enable utilizing the oxidative potential of ozone; they are stable for days to weeks. When in contact with bacteria, ozonides are responsible for direct oxidative damage to nucleic acids and membrane proteins. In addition, they can cause rupture of cell membranes; inhibition of cellular respiration; cessation of enzyme activities; improve local circulation and improves local circulation and production of proinflammatory molecules; stimulate release of growth factors, PDGF, TGF and VEGF; activate perioxidative systems, stimulate interferon synthesis, and increase phagocytosis. Disinfectants OR2 and H2OR2 stimulate proliferation of fibroblasts and keratinoblasts in tissue restoration processes; stimulate interferon synthesis and block pro-inflammatory factors, interleukins [6-9]; and oxidize prostaglandins [10]. It has been demonstrated topical application of ozonated oil can accelerate acute cutaneous wound repair in a guinea pig in association with the increased expression of PDGF, TGF-β, and VEGF. In addition, it was reported that O3 exposure is associated with activation of transcription factor NF-κB; this is important to regulate inflammatory responses and eventually the entire process of wound healing [9]. Liposomal ozonated oil can therefore be a useful alternative for countering the widespread and indiscriminate use of antibiotics, which has led to the emergence of bacterial resistance, especially in Staphylococci sp. Moreover, topical ozonated oil was seen to accelerate acute cutaneous wound repair in Guinea pig models by promoting collagen synthesis and fibroblast proliferation at the injury site. The purpose of the study was to improve the efficacy of treatment of bacterial keratitis by integrating an adjunctive liposomal ozone-based solution into comprehensive treatment. Material and Methods Forty-four patients (44 eyes) with bacterial keratitis, aged from 29 to 75 years, were involved in the study. Of these, 24 were men and 20 were women. Patients were divided into an ozone group of 21 patients and a control group of 23 patients. All patients were administered antibacterial therapy, mydriatics, desensibilizing agents, tissue preparations and vitamins. In addition, patients of the ozone group received an eye drop of ozone-based solution four times a day for 10 days. Patients underwent a routine eye examination including visual acuity, anterior segment slit-lamp biomicroscopy, ophthalmoscopy, anterior-segment optical coherence tomography (OCT), fluorescein staining assessment of corneal epithelization and pachymetry. The scale used for scoring inflammatory response consisted of five categories: mixed conjunctival injection; conjunctival discharge; corneal edema; and inflammatory infiltration of the superficial cornea. Mixed conjunctival injection was scored using the following scale: 0, physiological norm; 1, mild mixed injection; 2, moderate mixed injection; 3, marked mixed injection. Conjunctival discharge was scored using the following scale: 0, no discharge; 1, slight conjunctival mucous discharge; 2, abundant conjunctival mucous discharge; 3, mucopurulent conjunctival discharge. Corneal edema was scored using the following scale: 0, no corneal edema, transparent cornea; 1, local corneal epithelial edema at the site of inflammation; 2, local edema of the epithelium and superficial stroma; 3, local edema of the superficial and middle stroma. Inflammatory infiltration was scored using the following scale: 0, no infiltration; 1, moderate infiltration; 2, apparent infiltration; 3, diffuse infiltration. Conjunctival and corneal infiltrate cultures were taken at admission in all patients. Statistica v.6.1 software was used for statistical analysis. Number of observations (n), mean value (M), standard error of mean (m) and median (Med) were calculated to determine qualitative characteristics, and intensity, extensivity and clearness characteristics, to determine quantitative characteristics. Changes over the course of the disease with the treatment scheme used were reflected in patient’s medical records. All patients signed informed consent as per the Declaration of Helsinki. Results We conducted a microbiological study of conjunctival and corneal infiltrate cultures obtained from patients with bacterial keratitis. Cultures obtained from 10 of these patients (22.7%) gave no growth of pathogenic microflora because the ten patients had received antibacterial therapy at the place of their residence before admission. Cultures obtained from 18 patients (40.9%) gave growth of Gram-positive microflora (Staphylococcus epidermidis, Staphylococcus aureus, Streptococcus pneumoniae and Streptococcus pyogenes). Cultures obtained from 16 patients (36.4%) gave growth of Gram-negative microflora (Escherichia coli, Proteus, and Pseudomonas aeruginosa). Table 1 shows mean pre-treatment and post-treatment scores for the ozone group and controls. Median pre-treatment conjunctival discharge score for both groups was 2, indicating the prevalence of abundant conjunctival mucous discharge in patients of both groups before treatment. After treatment, median pre-treatment conjunctival discharge score for both groups was almost 0, indicating the prevalence of no conjunctival discharge in patients of both groups. Post-treatment changes in this measure were highly significant (р < 0.001). Mean pre-treatment conjunctival discharge scores for the ozone group and controls were 1.95 ± 0.06 and 1.83 ± 0.10, respectively (p = 0.10). After comprehensive treatment incorporating liposomal ozone-based solution, the mean conjunctival discharge score for the ozone group decreased to 0.11 ± 0.02, and was significantly different (p < 0.001) from the mean conjunctival discharge score for the controls (0.20 ± 0.03) (Table 1, Fig. 1).
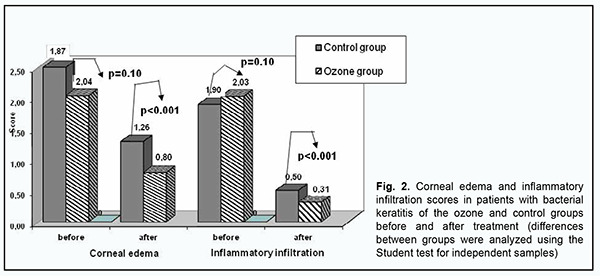
Prior to treatment, mixed conjunctival injection was moderate in the severity in both groups, with a mean mixed conjunctival injection score of 2, and but the difference between groups was not significant (p = 0.10). After treatment, the mixed conjunctival injection score in the ozone group decreased to the normal level (mean value, 0.19 ± 0.02; median value, 0), and this change was statistically significant (р < 0.001). In addition, after treatment, the mixed conjunctival injection score in the control group decreased significantly (р < 0.001), although conforming more closely to mild hyperemia (mean value, 0.56 ± 0.04; median value, 1) than to the norm. There was a significant difference (р < 0.001) in the mixed conjunctival injection score between the groups after treatment (Fig. 1). Table 1 and Fig. 2 demonstrate pre-to post-treatment improvements in corneal edema and inflammatory infiltration in patients of both groups.
Apparent inflammatory infiltration (with a median score of 2) was characteristics for patients at admission, and no infiltration was observed in most (62.8%) patients after treatment, with a mean inflammatory infiltration score decreased to 0.31 ± 0.04 in the ozone group and to 0.50 ± 0.05 in the control group (the intergroup difference was p < 0.001). Prior to treatment, there was local edema of the epithelium and superficial stroma in patients of both groups, with a median corneal edema score of 2. After treatment, there was an improvement in edema in most patients, with no edema in 30.7% and local edema of the epithelium in 35.1% of patients. In addition, after treatment, the mean corneal edema score was significantly lower in patients of the ozone group than in the controls (0.80 ± 0.05 versus 1.26 ± 0.07, respectively, p < 0.001). Moreover, cultures obtained from all patients after treatment gave no growth of pathogenic microflora. The length of inpatient stay at the hospital was shorter for patients of the ozone group than for the controls (11.6 ± 0.5 days versus 14.9 ± 0.6 days, respectively). Therefore, integrating an adjunctive liposomal ozone-based solution into comprehensive treatment for patients with bacterial keratitis led to a 3.3 ± 0.1 day reduction in the length of inpatient stay at hospital. Discussion The method allowed for a significant (р < 0.001) reduction in corneal and conjunctival inflammatory response, leading to acceleration of corneal epithelization and reduction in the length of treatment. Therefore, liposomal ozone-based solution was found to be efficacious in the treatment of bacterial keratitis, which allows recommending it for use in clinical practice.
References 1.Laboratory findings in tear fluid analysis. Ohashi Y, Dogru M, Tsubota K. Clin Chim Acta. 2006 Jul 15;369(1):17-28. 2.Miller D. Update on the epidemiology and antibiotic resistance of ocular infections. Middle East Afri J Ophthalmol. 2017;24(1):30-42. doi: 10.4103/meajo.MEAJO_276_16. 3.Ventola CL. The antibiotic resistance crisis: part 1: causes and threats. PT. 2015;40: 277–283. 4.Ting DSJ, Ho CS, Cairns J, et al. 12-year analysis of incidence, microbiological profiles and in vitro antimicrobial susceptibility of infectious keratitis: the Nottingham Infectious Keratitis Study. Br J Ophthalmol. 2021. 105 (3): 328–333. 5.Smith NL, Wilson AL, Gandhi J, et al. Ozone therapy: an overview of pharmacodynamics, current research, and clinical utility. Med Gas Res. 2017; 7(3):212–219. 6.Spadea L, Tonti E, Spaterna A, Marchegiani A. Use of ozone-based eye drops: a series of cases in veterinary and human spontaneous ocular pathologies. Case Rep Ophthalmol. 2018;9: 287–298. 7.Cagini C, Mariniello M, Messina M, et al. The role of ozonized oil and a combination of tobramycin/dexamethasone eye drops in the treatment of viral conjunctivitis: a randomized clinical trial. Int Ophthalmol. 2020;40(12):3209–3215. 8.Celenza G, Iorio R, Cracchiolo S, et al. Antimycotic activity of ozonized oil in liposome eye drops against Candida spp. Transl Vis Sci Technol. 2020;9:4. 9.Kim HS, Noh SU, Han YW, et al. Therapeutic effects of topical application of ozone on acute cutaneous wound healing. J Korean Med Sci. 2009;24(3):368–374. 10.Patel PV, Gujjari SK. The Morphometrical and Histopathological Changes which were Observed after Topical Ozone Therapy on an Exophytic Fibrous Gingival Lesion: A Case Report. J Clin Diagnostic Res. 2013 Jun;7(6):1239-43.
Disclosures Author Contribution: V.M. Sakovych: Conceptualization, Project administration, Investigation, Data curation, Writing-original draft, Writing-review & editing; O.V. Aleksieieva: Conceptualization, Data curation, Writing-original draft Disclaimer: The opinions presented in this article are those of the authors and do not necessarily represent those of their institutions. Funding sources: none
Conflict of Interest: V.M. Sakovych declares that he has no conflict of interest. .V. Aleksieieva declares that she has no conflict of interest.
|