Summary
Abstract
Relatively few patients (≤20%) with chronic hepatitis C achieve a sustained virological response after interferon-α monotherapy. Hence, alternative treatment strategies such as the addition of the broad spectrum antiviral agent ribavirin to interferon-a-2b have been investigated.
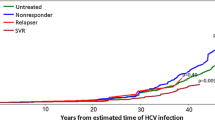
Combination therapy with subcutaneous interferon-α-2b [3 million units (MU) three times per week] plus oral ribavirin (1000 to 1200 mg/day) has proven effective in several well designed trials of 24 to 48 weeks’ duration in adult patients with compensated chronic hepatitis C. Compared with interferon-α-2b (3 or 6MU three times per week) with or without placebo, combination treatment with interferon-α-2b plus ribavirin significantly enhanced end-of-treatment and sustained virological and biochemical response rates in treatment-naive and treatment-experienced patients [sustained virological response rates in treatmentnaive recipients (6 to 19% vs 31 to 43% of patients); sustained overall (virological plus biochemical) response rates in nonresponders to (1 vs 14%) or relapsers (4 to 5% vs 30 to 44%) after previous interferon-a monotherapy]. Forty-eight weeks of combination therapy was superior to 24 weeks in treatment-naive patients infected with hepatitis virus C (HCV) genotype 1, whereas response rates were similar at 24 and 48 weeks in those infected with other HCV genotypes. Furthermore, there were marked improvements in histological inflammatory scores in patients who responded to treatment with either interferon-α-2b plus ribavirin or interferon-α-2b alone.
Although adverse events associated with either drug during combination therapy occurred frequently, these were generally mild to moderate in intensity and were consistent with those reported for each individual agent. Twenty-six percent of patients required dosage modifications of one or both drugs during combination therapy.
Conclusions: Interferon-α-2b plus ribavirin is an efficacious first- and second-line therapy in adult patients with compensated chronic hepatitis C, significantly improving sustained virological and biochemical responses versus interferon-α-2b monotherapy. The tolerability profile of interferon-α-2b plus ribavirin therapy is consistent with the individual profiles of these agents with no evidence of additive effects. The place of interferon-α-2b plus ribavirin combination therapy in relation to newer agents, including pegylated interferons-a and other multidrug regimens, remains to be determined in this rapidly evolving area of therapeutic management. Currently, combination therapy with interferon-α-2b plus ribavirin is recommended as first-line therapy for patients with chronic hepatitis C and compensated liver disease, and is an option for use as second-line therapy in those who have relapsed after, or failed to respond to, previous treatment with interferon-α.
Pharmacodynamic Profile
The precise mechanisms of action of interferon-α-2b and ribavirin, either alone or in combination, are not yet fully defined but appear to be multifactorial and complex. Although inhibition of viral activity and modulation of immune responses are postulated to play a key role in the mechanism of action of these two drugs, several other effects have also been reported that may contribute to their actions in patients with chronic hepatitis C, including effects on proliferation and extracellular matrix formation.
Antiviral activity: Inhibition of viral replication by interferon-α-2b is mediated via binding to specific type I receptors on the cell surface. Thereafter, the internalised interferon-α complex induces the release of more than 20 effector proteins (such as 2′5#x2032;-oligoadenylate synthetase, double-stranded RNA-dependent protein kinase and Mx proteins), which inhibit viral replication and/or function at various stages.
Although ribavirin has been shown to inhibit several viruses in vitro and in vivo, in patients with chronic hepatitis C ribavirin monotherapy lowered serum ALT concentrations, but had a negligible effect on serum hepatitis virus C (HCV) RNA concentrations. Results from in vitro studies suggest that several mechanisms may account for the antiviral effects of this agent, including the depletion of intracellular guanosine pools, inhibition of viral RNA polymerase and/or interference with transcription of viral messenger RNA. Ribavirin is actively transported into cells via membrane transporters, such as the sodium-dependent nucleoside transporters and nitrobenzylthioinosine-sensitive (es)-transporter on erythrocytes. Once internalised, the drug is metabolised by intracellular enzymes into active mono-, di- and triphosphates that act to inhibit viral replication.
No direct synergistic or additive antiviral effects were observed with interferon-α [3 to 6 million units (MU) three times per week] plus oral ribavirin (900 to 1200 mg/day) combination therapy in patients with chronic hepatitis C.
Immunomodulatory effects: Evidence increasingly points to the immunomodulatory effects of interferon-α-2b and ribavirin being responsible for the enhanced antiviral effects of these agents when used as combination therapy in patients with chronic hepatitis C.
Interferons-a exhibit various immunoregulatory effects in vitro including activation of monocytes and macrophages, induction of antigen expression on cell surfaces, increased natural killer cell activity and enhanced cytotoxic T lymphocyte activity. Interferons-a preferentially stimulate CD4+ T-helper type 1 (TH-1) cell cytokine [e.g. interleukin (IL)-2 and interferon-γ] production as opposed to T-helper type 2 cell responses (e.g. IL-4 and IL-10 synthesis).
Oral ribavirin (1000 to 1200 mg/day) monotherapy had no effect on serum IL-2, IL-4 or interferon-y concentrations in patients with chronic hepatitis C in a double-blind, placebo-controlled study. However, in liver transplant patients with recurrent HCV infection, the effects of ribavirin monotherapy on immune responses were equivocal. Nevertheless, in vitro and in vivo studies indicated that ribavirin may alter the balance between immune T-cell responses in favour of TH-1 type responses.
Notably, recent investigations indicated that interferon-a plus ribavirin combination therapy alters immune responses in favour of TH-1 type responses in patients with chronic hepatitis C. In 20 patients with chronic hepatitis C receiving subcutaneous interferon-a (type not stated) 5MU three times per week alone or in combination with oral ribavirin 1200 mg/day, there was a markedly greater upregulation of TH-1 cytokines (interferon-y and IL-2), natural killer cell subsets and accessory molecules (CD54+ CD14+, CD86+ CD14+, CD14/B7) in patients receiving combination therapy compared with interferon-a monotherapy (p < 0.001).
Other effects: Fibrosis, a common manifestation of advanced inflammatory diseases of the liver, is characterised by an increase in hepatic extracellular matrix which, in part, is regulated by transforming growth factor (TGF)-βl. Compared with 23 healthy volunteers, plasma TGF-βl concentrations were significantly elevated (1.9 vs 8.1 μg/L; p < 0.01), and correlated with the degree of fibrosis (p < 0.01), in 43 patients with chronic hepatitis C. Interferons-a reduced serum/plasma concentrations of TGF-μ1 in patients with chronic hepatitis C.
The incidence of neutralising antibodies to interferon-α appears to differ among the recombinant and natural forms of interferon-α. Neutralising antibodies developed in significantly fewer patients with chronic hepatitis C treated with interferon-α-2b (6.9% of 144 recipients; p < 0.01) or interferon-a-nl (1.3% of 78 recipients; p < 0.001) than in those who received interferon-a-2a (20% of 74 recipients). There are currently no reports on the incidence of neutralising antibodies in patients receiving interferon-a-2b plus ribavirin combination therapy.
Pharmacokinetic Profile
Limited data in adult patients with chronic hepatitis C indicated that no significant drug-to-drug interactions occurred between interferon-a-2b and ribavirin following coadministration of single and multiple doses of these agents. Pharmacokinetic parameters of interferon-α-2b or ribavirin have not been evaluated in patients >65 years of age, and there is a paucity of data in those aged <18 years.
Interferon-α-2b: Following subcutaneous administration of single or multiple doses of interferon-α-2b 3MU, maximum peak plasma concentrations (Cmax) were 13.9 and 29.7 IU/ml, respectively, and were attained in 7 and 5 hours in 12 patients with chronic hepatitis C. Total plasma clearance of interferon-α-2b after delivery of a single subcutaneous dose of 3MU was 14.3 L/h. The terminal elimination half-lives (t1/2) of the drug after single or multiple 3MU doses were 6.8 and 6.5 hours, respectively.
Ribavirin: Ribavirin is rapidly and extensively absorbed following oral administration. In 12 patients with chronic hepatitis C, mean Cmax values after single or multiple ribavirin 600mg doses were 0.78 and 3.68 mg/L, respectively, and were reached in 1.7 and 3 hours. The mean steady-state plasma concentration of oral ribavirin (600mg twice daily) was 2.2 mg/L and was attained in ≈4 weeks. The reported oral bioavailability of ribavirin after a single 600mg dose was 64% in six patients with chronic hepatitis C. Ribavirin has a large volume of distribution following oral administration (2825L), confirming the high tissue affinity of this drug. Ribavirin shows no detectable binding to plasma proteins.
Metabolism of ribavirin is mediated via a reversible phosphorylation pathway and a degradative pathway. Currently, there is no evidence of involvement of cytochrome P450 enzymes in the metabolic pathways of ribavirin, with the majority of ribavirin and its triazole metabolites excreted renally. Following multiple 600mg doses, the mean t1/2 of the drug was 298 hours which may reflect the high tissue affinity of the drug and its slow elimination from nonplasma compartments. In six patients with chronic hepatitis C, the mean total clearance of ribavirin following a single oral 600mg dose was 38.2 L/h. Respective mean renal and metabolic clearance rates were 6.9 and 18.1 L/h in six healthy volunteers after administration of a single intravenous 150mg radiolabelled dose of ribavirin followed by an oral 400mg dose of unlabelled drug.
Clearance of ribavirin is reduced in patients with a creatinine clearance of 0.6 to 1.8 L/h (10 to 30 ml/min) compared with healthy participants [creatinine clearance >5.4 L/h (>90 ml/min)]. The drug is not removed during haemodialysis and its use is not recommended in patients with severe renal impairment. Apart from mean Cmax values, pharmacokinetic parameters of oral ribavirin 600mg (single dose) in adult patients with varying degrees of hepatic dysfunction were not significantly different from those of healthy volunteers. Mean Cmax values were 0.89 (mild hepatic dysfunction), 1.05 (moderate), 1.27 (severe) and 0.64 μg/L (volunteers) [p = 0.029 vs volunteers for all groups].
Clinical Efficacy
The efficacy of interferon-α-2b plus ribavirin combination therapy in treatmentnaive and -experienced adult patients (>18 years of age) with chronic hepatitis C has been extensively evaluated in several well designed trials (≥300 enrolled patients). In clinical trials, interferon-α-2b (typically 3MU three times per week) was administered subcutaneously, whereas ribavirin (1000 to 1200 mg/day based on bodyweight, as a twice-daily divided dose) was taken orally.
Treatmentnaive adult patients: Markedly more recipients of first-line interferon-α-2b (3MU thrice weekly) plus ribavirin (1000 to 1200 mg/day) combination therapy achieved end-of-treatment virological (49 to 57% vs 24 to 33%) and biochemical (55 to 71 % vs 24 to 44%) responses than recipients of interferon-α-2b with or without placebo after 24 to 48 weeks’ therapy. Furthermore, sustained virological (31 to 43% vs 6 to 19%) and biochemical (32 to 50 vs 11 to 24%) responses were achieved by a significantly (p ≤ 0.003, all comparisons) greater percentage of patients receiving combination therapy than recipients of interferon-α-2b with or without placebo. Although a comparable number of recipients experienced end-of-treatment virological and biochemical responses after 24 and 48 weeks of combination therapy, an increased percentage of patients achieved a sustained virological response in the 48-week treatment group.
In 670 treatment-naive patients, histological responses paralleled therapeutic responses, with recipients of combination therapy (24 or 48 weeks) experiencing significantly (p ≤ 0.005, both comparisons) greater improvements in histological inflammatory scores than those receiving interferon-a-2b plus placebo for 48 weeks. Overall, irrespective of the treatment group, there was no effect on fibrosis scores, although 11 to 17% of patients in any individual group experienced an improvement in fibrosis score.
Treatment-experienced adult patients (nonresponders): In a large non-blind multicentre 24-week study in nonresponders, significantly (p ≤ 0.001) more recipients of combination therapy (interferon-α-2b 3MU three times weekly plus ribavirin 1000 to 1200 mg/day) achieved sustained overall (virological plus biochemical) responses than recipients of interferon-α-2b 6MU three times per week (14 vs 1% of patients). Induction therapy (interferon-α-2b 3MU once daily) during the first month of interferon-a-2b plus ribavirin treatment provided a similar beneficial effect on virological responses to the standard combination therapy regimen (interferon-α-2b three times per week plus ribavirin).
Treatment-experienced patients (relapsers): In relapsers (patients who had relapsed after previous interferon-a monotherapy), appreciably more recipients of interferon-α-2b plus ribavirin combination therapy experienced end-of-treatment and sustained virological and biochemical responses than those receiving interferon-α-2b 3MU three times per week in 24-week studies. In these two treatment groups, sustained overall (virological plus biochemical) responses were experienced by 30 to 44% and 4 to 5% of patients, respectively.
Furthermore, irrespective of the treatment regimen (interferon-α-2b plus ribavirin or interferon-α-2b monotherapy), improvements in histological activity index (HAI) inflammatory scores showed a significant association with a sustained virological response (p < 0.001) in 277 patients who had relapsed following previous interferon-α monotherapy. Hence, as predicted, significantly more combination therapy than interferon-α-2b plus placebo recipients experienced an improvement in HAI inflammatory score (63 vs 41% of recipients; p < 0.001), with respective mean decreases in HAI inflammatory scores of 2.6 and 0.7 (p < 0.001).
Other studies: In general, data in children and liver transplant recipients with chronic hepatitis C and in those coinfected with HIV are limited; further studies are warranted to confirm preliminary findings.
Interferon-α-2b (3MU three times per week) plus ribavirin (1000 to 1200 mg/day) combination therapy was effective in patients infected with HCV genotype lb, a known predictor of a poor response rate to interferons-a monotherapy treatment. As predicted, subgroup analysis from two large placebo-controlled studies indicated that significantly (p < 0.001) more patients infected with HCV genotypes 2 or 3 responded to combination treatment than those infected with HCV genotype 1. In patients infected with HCV genotype 1, 48 weeks’ combination therapy was significantly better than 24 (28 vs 16% of patients with a sustained virological response; p = 0.01).
Furthermore, combination therapy was also significantly more effective than interferon-α-2b monotherapy in Black patients with chronic hepatitis C and in patients with cirrhosis of the liver at baseline. These two groups of patients have historically proven to be difficult to treat with interferon-a monotherapy.
In treatment-naive patients, factors shown to be correlated with improved response rates were baseline viral load ≤2 x 106 copies/ml (p < 0.001), the absence of cirrhosis at baseline (p < 0.05), female gender (p = 0.05) and young age (p = 0.005). Of note, regardless of the risk factors present, combination therapy recipients achieved significantly better sustained responses than interferon-α-2b monotherapy patients (p < 0.001, all comparisons).
Chronic HCV infection has a significant impact on a patient’s quality of life. In treatment-naive patients and those who had relapsed after previous interferon-α monotherapy, sustained responders to either interferon-α-2b plus ribavirin or interferon-α-2b treatment experienced appreciable improvements in generic and hepatitis-specific quality-of-life scores.
Pharmacoeconomic Considerations
In treatment-naive patients with chronic hepatitis C, interferon-α-2b plus ribavirin for 24 or 48 weeks prolonged quality-adjusted life expectancy and was cost-effective (1999 values; direct and indirect costs) from the societal perspective compared with interferon-α-2b monotherapy in 1744 participants in a US and a multinational trial. Although treatment with combination therapy for 24 or 48 weeks ($US18 300 and $US20 900, respectively) was more costly than that of interferon-α-2b monotherapy (US$15 000) for 48 weeks, combination treatment yielded greater unadjusted and quality-adjusted life expectancy.
Furthermore, sensitivity analysis indicated that 24 and 48 weeks’ combination therapy remained cost effective at<$US7300 per discounted quality-adjusted life year (QALY) gained versus 48 weeks’ monotherapy, irrespective of gender, location, initial liver histology, viral load, viral genotype or the number of predictors of a positive response to therapy. Additionally, 48 weeks of treatment with combination therapy was more cost effective than 24 weeks for all subgroups except viral genotype 2 and 3.
A cost-utility analysis of 345 relapsers indicated that, at a 3% discounted rate, compared with interferon-α-2b alone, lifetime costs with combination therapy were marginally more expensive, but prognosis was improved by 2 QALYs, providing a marginal cost-effectiveness ratio of $US140 per QALY gained (1995 values). Notably, despite the fact that HCV genotype 1 and high viral loads (>2 million copies/ml) are associated with a poor response rate, the marginal cost-effectiveness ratio in relapse patients with both of these characteristics would be $US7700 per QALY gained.
The outcomes and costs (1998 values) of interferon-α-2b plus ribavirin combination therapy have been compared with other treatment strategies using data from several clinical trials. Compared with interferon-α-2b alone for 48 weeks followed by combination therapy in relapsers, combination therapy based on HCV genotype demonstrated the best incremental cost-effectiveness ratio ($US7500 per QALY) and a cost per additional sustained virological response of $US54 000. All other strategies evaluated were dominated.
Tolerability
Adverse effects are commonly observed in patients with chronic hepatitis C during therapy with interferon-a, including interferon-α-2b, and are related to the dose, frequency and duration of treatment and disease stage. In general, collated tolerability data from 2089 participants in clinical trials indicated that the adverse event profile with combination therapy was consistent with profiles observed with the individual drugs. In these patients, anorexia, dyspnoea, pruritus and rash were shown to occur with at least a 5% greater frequency with interferon-α-2b plus ribavirin combination therapy than interferon-α-2b monotherapy.
Adverse events occurring in recipients of interferon-α-2b plus ribavirin or interferon-α-2b involved all organ systems of the body, with the majority of patients experiencing at least one adverse event. These events included haemolytic anaemia (experienced by ≈7% of patients), influenza-like symptoms (>90%), laboratory abnormalities (8 to 35%), and gastrointestinal (10 to 46%), psychiatric (15 to 40%), respiratory tract (10 to 20%) and dermatological (10 to 30%) adverse events.
Although adverse events occurred frequently with interferon-α-2b plus ribavirin combination therapy, dosage modifications of one or both agents as recommended resulted in relatively few patients discontinuing combination treatment in clinical trials. In large randomised trials, 6 to 11 % of recipients of combination therapy discontinued treatment versus 3 to 9% in the interferon-α-2b groups with 24 weeks’ therapy. Pooled data indicated that haemolytic anaemia (haemoglobin concentrations <100 g/L), associated with ribavirin therapy, led to dosage reductions or discontinuation of treatment in 1 to 14% of patients. Following cessation of therapy, haemoglobin concentrations and reticulocyte counts returned to pretreatment concentrations after 3 to 10 weeks. No clinically relevant changes were observed in leucocyte or platelet counts in either treatment group in large clinical trials.
In comparative trials evaluating interferon-α-2b plus ribavirin combination therapy or interferon-α-2b alone, serious (grade 3) or life-threatening (grade 4) adverse events occurred in 17 and 10% of treatment-naive and treatment-experienced patients, respectively. Notably, there was no difference between combination and interferon-α-2b monotherapy groups in the incidence of these grade 3 and 4 adverse events in pooled data. Clinically significant serious (grades 3 or 4) cardiovascular, psychiatric, gastrointestinal, respiratory and dermatological adverse events occurred in 0.9, 1.1, 0.6, 0.4 and 0.1 % of patients, respectively, in clinical trials.
Dosage and Administration
Combination therapy with subcutaneous interferon-α-2b plus oral ribavirin is recommended for the treatment of chronic hepatitis C in adult patients with compensated liver disease who have not been previously treated with interferon-α, or who have failed to respond to or relapsed after a previous interferon-α therapy. There are currently no recommendations for the use of combination therapy in patients <18 years of age. In treatment-naive patients, the recommended duration of treatment is 24 or 48 weeks, based on baseline disease characteristics, response to therapy and tolerability, whereas 24 weeks’ treatment is recommended for treatment-experienced patients.
The recommended dosage of subcutaneous interferon-α-2b is 3MU three times per week, whereas that of ribavirin is 1000 mg/day in patients with a body-weight ≤75kg and 1200 mg/day in those over 75kg (as a twice-daily divided dose). Ribavirin may be administered without regard for food, but should be administered in a consistent manner. Dosage modification of one or both drugs is required in ≈26% of patients.
Combination therapy with interferon-α-2b plus ribavirin is contraindicated in women who are pregnant and in the male partners of women who are pregnant. If pregnancy does occur during or within 6 months of completing therapy, patients must be advised of the significant teratogenic risk of ribavirin therapy to the fetus. In lactating mothers, a decision should be made whether to discontinue treatment with combination therapy or to discontinue nursing.
Combination therapy with interferon-α-2b plus ribavirin is also contraindicated in patients with autoimmune hepatitis or in those with a history of hypersensitivity to either agent or any component of the capsule and/or injection. It should be used with caution in patients with a creatinine clearance <3 L/h (<50 ml/min), since the clearance of ribavirin is reduced in patients with severe renal impairment. Combination therapy is not recommended in patients with haemoglobinopathies, decompensated cirrhosis, previous or current serious psychiatric disorders, diabetes mellitus, pre-existing autoimmune disorders or uncontrolled thyroid disorders.


















Similar content being viewed by others
References
Alter MJ. Epidemiology of hepatitis C. Hepatology 1997; 26 Suppl.: 62–5
Teixeira R, Pastacaldi S, Papatheodoridis GV, et al. Recurrent hepatitis C after liver transplantation. J Med Virol 2000; 61: 443–54
Par A. Diagnosis and management of chronic hepatitis C. Can J Gastroenterol 2000; 14 Suppl. B: 83–8
Kasahara A. Treatment strategies for chronic hepatitis C virus infection. J Gastroenterol 2000; 35: 411–23
Powell DW, Abramson BZ, Balint JA, et al. National Institutes of Health Consensus Development Conference panel statement: management of hepatitis C. Hepatology 1997 Sep; 26 Suppl. l: 2S–10S
Hoofnagle JH. Hepatitis C: the clinical spectrum of disease. Hepatology 1997; 26 Suppl. 1: 15S–20
Lawrence SP. Advances in the treatment of hepatitis C. In: Advances in internal medicine. Vol. 45. St Louis; Mosby Inc, 2000: 65–105
Lam NP. Pharmacological management of chronic viral hepatitis. J Pharm Care Pain Symptom Control 1998; 6(3): 41–62
Par A, Gervain J, Gogl A. Hepatitis C virus infection: pathogenesis, diagnosis and treatment. Scand J Gastroenterol 1998; 33 Suppl. 228: 107–14
Soriano V, Rodríguez-Rosado R, García-Samaniego J. Management of chronic hepatitis C in HIV-infected patients. AIDS 1999 Apr 1; 13: 539–46
Purcell R. The hepatitis C virus: overview. Hepatology 1997; 26 Suppl. 1: 11S–4
Booth JCL, Waters J, Brown JL, et al. The cellular tropism of HCV [abstract no. P/Cl/71]. J Hepatol 1995; 23 Suppl. 1: 104
Berenguer M, Wright TL. Hepatitis C and liver transplantation. Gut 1999 Aug; 45: 159–63
Schalm SW, Fattovich G, Brouwer JT. Therapy of hepatitis C: patients with cirrhosis. Hepatology 1997 Sep; 26 Suppl. 1: 128S–32S
Gitnick G. Hepatitis C: controversies, strategies and challenges. Eur J Surg Suppl 1998; 582: 65–70
Galmiche JP. French consensus conference on hepatitis C: screening and treatment. Gut 1998 Jun; 42: 892–8
Dhumeaux D, Doffoël M, Galmiche J-P. A French consensus conference on hepatitis C: screening and treatment. J Hepatol 1997 Nov;27: 941–4
Bizollon T, Ducerf C, Trepo C, et al. Hepatitis C virus recurrence after liver transplantation. Gut 1999 Apr; 44: 575–8
Tong MJ, El-Farra NS, Reikes AR, et al. Clinical outcomes after transfusion-associated hepatitis C. N Engl J Med 1995; 332: 1463–6
Thomas HC, Booth J, Brown J. Pathophysiology and treatment of hepatitis C. Drugs 1996; 52 Suppl. 2: 1–8
Gutfreund KS, Bain VG. Chronic viral hepatitis C: management update. Can Med Assoc J 2000 Mar 21; 162: 827–33
Foster GR, Goldin RD, Thomas HC. Chronic hepatitis C virus infection causes a significant reduction in quality of life in the absence of cirrhosis. Hepatology 1998; 27: 209–12
Simmonds P, Alberti A, Alter HJ, et al. A proposed system for the nomenclature of hepatitis C viral genotypes. Hepatology 1994; 19: 1321–4
Dusheiko G, Schmilovitz-Weiss H, Brown D, et al. Hepatitis C virus genotypes: an investigation of type-specific differences in geographic origin of disease. Hepatology 1994; 19: 13–8
Krick SE, Gwinn KA, Morgan DR. Pathophysiology and treatment of hepatitis C infection. J Pharm Pract 1999; 12(5): 391–400
Dorr RT. Interferon-α in malignant and viral diseases. Drugs 1993; 45: 177–210
National Institutes of Health Consensus Development Conference Panel. National Institutes of Health Consensus Development Conference Panel Statement: management of hepatitis C. Hepatology 1997; 26 Suppl. 1: 2S–10
Dusheiko G. Side effects of alpha interferon in chronic hepatitis C. Hepatology 1997 Sep; 26 Suppl. 1: 112S–21S
Ahmed A, Keeffe EB. Treatment strategies for chronic hepatitis C: update since the 1997 National Institutes of Health Consensus Development Conference. J Gastroenterol Hepatol 1999 May; 14 Suppl.: S12–18
Booth JCL, O’Grady J, Neuberger J. Clinical guidelines on the management of hepatitis C. Royal College of Physicians of London and the British Society of Gastroenterology. Gut 2001; 49 Suppl. I: il–21
Patterson JL, Fernandez-Larsson R. Molecular mechanisms of action of ribavirin. Rev Infect Dis 1990; 12(6): 1139–46
Cirelli R, Tyring SK. Major therapeutic uses of interferons. Clin Immunother 1995; 3: 27–87
Dianzani F. Biological basis for the clinical use of interferon. Gut 1993; 34 Suppl.: S74–76
Staeheli P. Interferon-induced proteins and the antiviral state. Adv Vir Res 1990; 38: 147–200
Samuel CE. Mechanisms of the antiviral action of interferons. Prog Nuc Acid Res Mol Biol 1988; 35: 27–71
Giannelli G, Antonelli G, Fera G, et al. 2′,5#x2032;-Oligoadenylate synthetase activity as a responsive marker during interferon therapy for chronic hepatitis C. J Interferon Res 1993; 13: 57–60
Caselmann WH, Meyer M, Scholz S, et al. Type I interferons inhibit hepatitis B virus replication and induce hepatocellular gene expression in cultured liver cells. J Infect Dis 1993; 166: 966–71
Lam NP, Neumann AU, Gretch DR, et al. Dose-dependent acute clearance of hepatitis C genotype 1 virus with interferon alfa. Hepatology 1997; 26: 226–31
Neumann AU, Lam NP, Dahari H, et al. Hepatitis C viral dynamics in vivo and the antiviral efficacy of interferon-α therapy. Science 1998; 282: 103–7
Reichard O, Andersson J, Schvarcz R, et al. Ribavirin treatment for chronic hepatitis C. Lancet 1991; 337: 1058–61
Di Bisceglie AM, Shindo M, Fong T-L, et al. A pilot study of ribavirin therapy for chronic hepatitis C. Hepatology 1992; 16: 649–54
Reichard O, Yun Z-B, Sönnerborg A, et al. Hepatitis C viral RNA titers in serum prior to, during, and after oral treatment with ribavirin for chronic hepatitis C. J Med Virol 1993; 41: 99–102
Bodenheimer Jr HC, Lindsay KL, Davis GL, et al. Tolerance and efficacy of oral ribavirin treatment of chronic hepatitis C: a multicenter trial. Hepatology 1997; 26: 473–7
Dusheiko G, Main J, Thomas H, et al. Ribavirin treatment for patients with chronic hepatitis C: results of a placebo-controlled study. J Hepatol 1996; 25: 591–8
Paul SD, Ngo LY, Glue P, et al. Intestinal absorption of ribavirin is preferentially mediated by the Na+ nucleoside purine (Nl) transporter. Pharm Res 1998; 15(6): 950–2
Jarvis SM, Thorn JA, Glue P. Ribavirin uptake by human erythrocytes and the involvement of nitrobenzylthioinosine-sensitiv (es)-nucleoside transporters. Br J Pharmacol 1998; 123: 1587–92
Yamada Y, Natsumeda Y, Weber G. Action of the active metabolites of tiazofurin and ribavirin on purified IMP dehydrogenase. Biochemistry 1988; 44: 2236–9
Sidwell RW, Robins RK, Hillyard IW. Ribavirin: an antiviral agent. Pharmacol Ther 1979; 6: 123–46
Glue P. The clinical pharmacology of ribavirin. Semin LiverDis 1999; 19 Suppl. 1: 17–24
Sidwell RW, Huffman JH, Khare GP, et al. Broad-spectrum antiviral activity of Virazole: 1-β-D-ribofuranosyl-1,2,4-triazole-3-carboxamide. Science 1972; 177: 705–6
Lee H-J, Pawlak K, Nguyen BT, et al. Biochemical differences among four inosinate dehydrogenase inhibitors, mycophenolic acid, ribavirin tiazofurin, and selenazofurin, studied in mouse lymphoma cell culture. Cancer Res 1985; 45: 5512–20
Streeter DG, Witkowski JT, Gyaneshwar PK, et al. Mechanism of action of 1-β-D-ribofuranosyl-1,2,4-triazole-3-carboxamide (Virazole), a new broad-spectrum antiviral agent. Proc Nat Acad Sci USA 1973; 70(4): 1174–8
Zeuzem S, Schmidt JM, Lee J-H, et al. Hepatitis C virus dynamics in vivo: effect of ribavirin and interferon alfa on viral turnover. Hepatology 1998; 28: 245–52
Khakoo S, Glue P, Grellier L, et al. Ribavirin and interferon alfa-2b in chronic hepatitis C: assessment of possible pharmacokinetic and pharmacodynamic interactions. Br J Clin Pharmacol 1998 Dec; 46: 563–70
Martin J, Navas S, Quiroga JA, et al. Effects of the ribavirininterferon alpha combination on cultured blood mononuclear cells from chronic hepatitis C patients. Cytokine 1998; 10(8): 635–44
Tilg H. New insights into the mechanisms of interferon alfa: an immunoregulatory and anti-inflammatory cytokine. Gastroenterology 1997; 112: 1017–21
Dunk AA, Novick D, Thomas HC. Natural killer cell activity in hepatocellular carcinoma: in vitro and in vivo responses to interferon. Scand J Gastroenterol 1987; 22: 1245–50
Cacciarelli TV, Martinez OM, Gish RG, et al. Immunoregulatory cytokines in chronic hepatitis C virus infection: pre- and post-treatment with interferon alfa. Hepatology 1996; 24: 6–9
García-Monzón C, García-Buey L, García-Sánchez A, et al. Down-regulation of intercellular adhesion molecule 1 on hepatocytes in viral chronic hepatitis treated with interferon alfa-2b. Gastroenterology 1993; 105: 462–9
Hultgren C, Milich DR, Weiland O, et al. The antiviral compound ribavirin modulates the T helper (Th) 1/Th2 subset balance in hepatitis B and C virus-specific immune responses. J Gen Virol 1998 Oct; 79 (Pt 10): 2381–91
Quadri R, Giostra E, Rubbia-Brandt L, et al. Mechanism of action of ribavirin in treatment of recurrent hepatitis C after liver transplant. J Hepatol 2000; 32 Suppl. 2: 91
Cello J, Flichman D, Castaño G, et al. Study of the effects of ribavirin on cytokine production of recall antigen and PHA-stimulated peripheral mononuclear cells. J Hepatol 1999; 30 Suppl. 1: 70
Lilly LB, Cattral MC, Greig PD, et al. Ribavirin treatment of recurrent hepatitis C virus following liver transplantation: proposed mechanism of action. Transplantation 1998 Jun 27; 65: S32
Ning Q, Brown D, Parodo J, et al. Ribavirin inhibits viralinduced macrophage production of TNF, IL-1, the procoagulant fgl2 prothrombinase and preserves Thl cytokine production but inhibits Th2 cytokine response. J Immunol 1998 Apr 1; 160: 3487–93
Tarn RC, Pai B, Bard J, et al. Ribavirin polarizes human T cell responses towards a Type 1 cytokine profile. J Hepatol 1999 Mar; 30: 376–82
Kissinger GL, Stachowski J, Pollok M, et al. Effects of INF-α- therapy compared to combined therapy with ribavirin/INF-α on cytokine profiles, natural killer cell activity and costimulatory molecule expression in patients with chronic hepatitis C. Hepatology 1998 Oct; 28 Suppl. (Pt 2): 565
Rasul I, Liu M, Ning J, et al. Treatment of hepatitis C infection +/- ribavirin promoted conversion of TH2 to TH1 cytokine profile and decreased inflammation [abstract no. 1733]. Hepatology 1999; 30 Suppl. Pt 2: 594
Pawlowska M, Halota W, Topczewska-Staubach E. Influence of IFN and ribavirin on ICAM-1 serum concentration in chronic C hepatitis treatment. J Hepatol 1998; 28 Suppl. 1: 200
Perry CM, Wilde MI. Interferon-α-2a: a review of its use in chronic hepatitis C. Biodrugs 1998 Jul; 10: 65–89
Perry CM, Wagstaff AJ. Interferon-α-nl: a review of its pharmacological properties and therapeutic efficacy in the management of chronic viral hepatitis. Biodrugs 1998 Feb; 9: 125–54
Antonelli G, Currenti M, Turriziani O, et al. Neutralizing antibodies to interferon-α: relative frequency in patients treated with different interferon preparations. J Infect Dis 1991; 163: 882–5
Wong S, Gauthier T, Kaita KDE, et al. The differential effects of three forms of interferon alfa on hepatic regeneration after partial hepatectomy in the rat. Hepatology 1995; 21: 883–6
Fang JW, Lai VC, Cohard M, et al. The effect of interferon-alfa-2B/ribavirin (Rebetron) on serum transforming growth factor beta-1 in patients with chronic hepatitis C [abstract]. Hepatology 1999 Oct; 30 Suppl. (Pt 2): 593
Ilyin GP, Langouët S, Rissel M, et al. Ribavirin inhibits protein synthesis and cell proliferation induced by mitogenic factors in primary human and rat hepatocytes. Hepatology 1998; 27: 1687–94
Peavy DL, Koff WC, Hyman D, et al. Inhibition of lymphocyte proliferative responses by ribavirin. Infect Immun 1980; 29(2): 583–9
Samuel CE. Antiviral actions of interferon: interferon-regulated cellular proteins and their surprisingly selective antiviral activities. Virology 1991; 183: 1–11
Blair CS, Haydon GH, Hayes PC. Current perspectives on the treatment and prevention of hepatitis C infection. Expert Opin Invest Drug 1996 Dec; 5: 1657–71
Lindsay KL. Therapy of hepatitis C: an overview. Hepatology 1997 Sep; 26 Suppl. 1: 71S–7S
Baron S, Tyring SK, Fleischmann Jr WR, et al. The interferons: mechanisms of action and clinical applications. JAMA 1991; 266(10). 1375–1388
Davis MG, Jansen RW. Inhibition of hepatitis B virus in tissue culture by alpha interferon. Antimicrob Agents Chemother 1994; 38(12): 2921–4
Pawlotsky J-M. Hepatitis C virus resistance to antiviral therapy. Hepatology 2000; 32: 889–96
Enomoto N, Sakuma I, Asahina Y, et al. Mutations in the non-structural protein 5A gene and response to interferon in patients with chronic hepatitis C virus lb infection. N Engl J Med 1996; 334: 77–81
Enomoto N, Sakuma I, Asahina Y, et al. Comparison of fulllength sequences of interferon-sensitive and resistant hepatitis C virus 1b: sensitivity to interferon is conferred by amino acid substitutions in the NS5Aregion. J Clin Invest 1995; 96: 224–30
Castéra L, Germanidis G, Frainais PO, et al. Early changes in HCV hypervariable region 1 (HVR1) and non structural (NS) 5A gene quasispecies during interferon-α or ribavirin treatment: clues to the mechanisms of HCV resistance to antiviral therapy [abstract]. Hepatology 1998 Oct; 28 Suppl. (Pt. 2): 288
Gerotto M, Sullivan D, Pontisso P, et al. Evidence for reduced rates of quasispecies diversification during combination interferon plus ribavirin therapy for chronic hepatitis C [abstract no. WP2/10]. J Hepatol 1998; 28 Suppl. 1: 55
Roitt IM. The acquired immune response. In: Roitt IM, editor. Essential immunology. 7th ed. London: Blackwell Scientific Publications, 1991: 129–52
Orland JR, Wright TL, Cooper S. Acute hepatitis C. Hepatology 2001; 33(2): 321–7
Thomas HC, Waters JA. Future approaches to treatment of chronic hepatitis B and hepatitis C infection. J Viral Hepatitis 1997; 4 Suppl. 2: 92–7
Rice CM, Walker CM. Hepatitis C virus-specific T lymphocyte responses. Curr Opin Immunol 1995; 7: 532–8
Koskinas J, McFarlane BM, Nouri-Aria KT, et al. Cellular and humoral immune reactions against autoantigens and hepatitis C viral antigens in chronic hepatitis C. Gastroenterology 1994; 107: 1436–42
Botarelli P, Brunetto MR, Minutello MA, et al. T-lymphocyte response to hepatitis C virus in different clinical courses of infection. Gastroenterology 1993; 104: 580–7
Battegay M, Fikes J, Di Bisceglie AM, et al. Patients with chronic hepatitis C have circulating cytotoxic T cells which recognize hepatitis C virus-encoded peptides binding to HLA-A2.1 molecules. J Virol 1995; 69(4): 2462–70
Koziel MJ, Dudley D, Afdhal N, et al. Hepatitis C virus (HCV)-specific cytotoxic T lymphocytes recognize epitopes in the core and envelope proteins of HCV. J Virol 1993; 67: 7522–32
Diepolder HM, Zachoval R, Hoffmann RM, et al. Possible mechanism involving T-lymphocyte response to non-structural protein 3 in viral clearance in acute hepatitis C virus infection. Lancet 1995; 346: 1006–7
Grüner NH, Gerlach TJ, Jung M-C, et al. Association of hepatitis C virus-specific CD8+ T cells with viral clearance in acute hepatitis C. J Infect Dis 2000; 181: 1528–36
Missale G, Bertoni R, Lamonaca V, et al. Different clinical behaviors of acute hepatitis C virus infection are associated with different vigor of the anti-viral cell-mediated immune response. J Clin Invest 1996; 98: 706–14
Sai SL, Liaw YF, Chen MH, et al. Detection of type-2-like T-helper cells in acute hepatitis C virus infection: implications for hepatitis C virus chronicity. Hepatology 1997; 25: 449–58
Congia M, Clememte MG, Dessi C, et al. HLA class II genes in chronic hepatitis C virus: infection and associated immunological disorders. Hepatology 1996; 24: 1338–41
Tibbs C, Donaldson P, Underhill J, et al. Evidence that the HLA DQA1 *03 allele confers protection from chronic HCV-infection in northern European caucasoids. Hepatology 1996; 24: 1342–5
Pape GR, Gerlach TJ, Diepolder HM, et al. Role of specific T-cell response for clearance and control of hepatitis C virus. J Viral Hepatol 1999; 6 Suppl. 1: 36–40
Cucchiarini M, Kammer AR, Grabscheid B, et al. Vigorous peripheral blood cytotoxic T cell responses during the acute phase of hepatitis C virus infection. Cell Immunol 2001; 203: 111–23
Battegay M. Immunity to hepatitis C virus: a further piece of the puzzle. Hepatology 1996; 24(4): 961–3
Lechmann M, Ihlenfeldt HG, Braunschweiger I, et al. T- and B-cell responses to different hepatitis C virus antigens in patients with chronic hepatitis C infection and in healthy antihepatitis C virus-positive blood donors without viremia. Hepatology 1996; 24: 790–5
Lechner F, Gruener NH, Urbani S, et al. CD8+ T lymphocyte responses are induced during acute hepatitis C virus infection but are not sustained. Eur J Immunol 2000; 30: 2479–87
Nouri-Aria KT, Alexander GJM, Magrin S, et al. Differential effect of alpha-interferons on CD4- and CD8-positive lymphocytes in chronic hepatitis B virus carriers. J Hepatol 1988; 7: 1–6
Bolacchi F, Bergamini A, Tisone G, et al. Ribavirin decreases interferon-gamma production in liver transplant recipients with recurrent HCV infection. J Hepatol 2000; 32 Suppl. 2: 50
Castilla A, Prieto J, Fausto N. Transforming growth factors β1 and alpha in chronic liver disease. N Engl J Med 1991; 324(14): 933–40
Merrilees MJ, Scott L. Transforming growth factor beta. Patient Manage N Z 1994; 23(3): 13–5
Tsushima H, Kawata S, Tamura S, et al. Reduced plasma transforming growth factor-βl levels in patients with chronic hepatitis C after interferon-cc therapy: association with regression of hepatic fibrosis. J Hepatol 1999; 30: 1–7
Sanderson N, Factor V, Nagy P, et al. Hepatic expression of mature transforming growth factor-β 1 in transgenic mice results in multiple tissue lesions. Proc Nat Acad Sci USA 1995; 92: 2572–6
Capra F, Casaril M, Gabrielli GB, et al. Alpha-interferon in the treatment of chronic viral hepatitis: effects on fibrogenesis serum markers. J Hepatol 1993; 18: 112–8
Zöhrens G, Armbrust T, Meyer Zum Büschenfelde K-H, et al. Interferon-α-2a increases serum concentration of hyaluronic acid and type III procollagen aminoterminal propeptide in patients with chronic hepatitis B virus infection. Dig Dis Sci 1994; 39(9): 2007–13
Milella M, Antonelli G, Santantonio T, et al. Neutralizing antibodies to recombinant alpha-interferon and response to therapy in chronic hepatitis C virus infection. Liver 1993; 13: 146–50
Milella M, Antonelli G, Santantonio G, et al. Treatment with natural IFN of hepatitis C patients with or without antibodies to recombinant IFN. Hepatogastroenterology 1995; 42: 201–4
Antonelli G, Giannelli G, Pistello M, et al. Clinical significance of recombinant interferon-α2 neutralizing antibodies in hepatitis patients. J Interferon Res 1994; 14: 211–3
Rebetron. 2000 Mosby’s GenRx Update 3 [online]. Available from URL: http://www.mosbysgenrx [Accessed 2001 Jan 10]
Cada DJ, Levien T, Baker DE. Paricalcitol injection and ribavirin/interferon alfa-2b. Hosp Pharm 1999; 34(3): 303–38
Bunn CS, Kelly D, Murray KF, et al. Safety, efficacy and pharmacokinetics of interferon-alfa-2b and ribavirin in children with chronic hepatitis C [abstract no. 763]. Hepatology 2000; 32 Pt. 2: 350A
Preston SL, Drusano GL, Glue P, et al. Pharmacokinetics and absolute bioavailability of ribavirin in healthy volunteers as determined by stable-isotope methodology. Antimicrob Agents Chemother 1999 Oct; 43: 2451–6
Glue P, Schenker S, Gupta S, et al. The single dose pharmacokinetics of ribavirin in subjects with chronic liver disease. Br J Clin Pharmacol 2000 May; 49: 417–21
Dieterich DT, Purow JM, Rajapaksa R. Activity of combination therapy with interferon alfa-2b plus ribavirin in chronic hepatitis C patients co-infected with HIV. Semin Liver Dis 1999; 19 Suppl. 1: 87–94
Ribavirin. Presc Int 2000; 9(47): 72–5
Hoggard PG, Kewn S, Barry MG, et al. Effects of drugs on 2’,3’-dideoxy-2′,3′-didehydrothymidine phosphorylation in vitro. Antimicrob Agents Chemother 1997; 41(6): 1231–6
Japour AJ, Lertora JJ, Meehan PM, et al. A phase-I study of the safety, pharmacokinetics, and antiviral activity of combination didanosine and ribavirin in patients in HIV-1 disease. J Acquir Immune Defic Syndrom Hum Retrovirol 1996; 13: 235–46
Barbaro G, Di Lorenzo G, Soldini M, et al. Evaluation of long-term efficacy of interferon α-2b and ribavirin in combination in naive patients with chronic hepatitis C: an Italian multicenter experience. J Hepatol 2000 Sep; 33: 448–55
Ferenci P, Brunner H, Vogel W, et al. Interferon induction therapy in combination with ribavirin in chronic hepatitis C [abstract]. J Hepatol 2000; 32 Suppl. 2: 38
McHutchinson JG, Gordon SC, Schiff ER, et al. Interferon alfa-2b alone or in combination with ribavirin as initial treatment for chronic hepatitis C. N Engl J Med 1998 Nov 19; 339(21): 1485–92
Pol S, Nalpas B, Bourlière M, et al. Combination of ribavirin and interferon-alfa surpasses high doses of interferon-alfa alone in patients with genotype-lb-related chronic hepatitis C. Hepatology 2000 Jun; 31: 1338–44
Poynard T, Marcellin P, Lee SS, et al. Randomised trial of interferon α-2b plus ribavirin for 48 weeks or for 24 weeks versus interferon α-2b plus placebo for 48 weeks for treatment of chronic infection with hepatitis C virus. Lancet 1998 Oct 31; 352: 1426–32
Barbaro G, Di Lorenzo G, Belloni G, et al. Interferon α-2B and ribavirin in combination for patients with chronic hepatitis C who failed to respond to, or relapsed after, interferon alpha therapy: a randomized trial. Am J Med 1999 Aug; 107: 112–8
De Lédinghen V, Bernard PH, Trimoulet P, et al. Retreatment for chronic hepatitis C of interferon non-responder patients. Preliminary results of a multicenter, randomised, controlled trial of interferon plus ribavirin versus interferon alone [abstract no. 848]. Hepatology 1998; 28 (4 Pt. 2): 374A
Gish RG, Wakil AE, Brooks LJ, et al. Arandomized trial of daily interferon α-2b in combination with ribavirin vs three times a week for one month, followed by three times a week for one year in relapse and nonresponder patients [abstract no. 1132]. Hepatology 2000; 32 Pt. 2: 442
Davis GL, Esteban-Mur R, Rustgi V, et al. Interferon alfa-2b alone or in combination with ribavirin for the treatment of relapse of chronic hepatitis C. N Engl J Med 1998 Nov 19; 339: 1493–9
Goodman Z, Albrecht JK, Ling MH, et al. Clinical resolution of hepatitis C in the era of interferon-α/ribavirin combination therapy — data on interferon-cc relapsers at the end of 6-month follow-up [abstract]. Hepatology 1998 Oct; 28 Suppl. Pt. 2: 507
Waters B, Fleckenstein JF, Ismail MK, et al. Efficacy of interferon and ribavirin for hepatitis C in patients previously treated with interferon alone [abstract]. Hepatology 1998 Oct; 28 Suppl. Pt 2: 283A
Saracco G, Ciancio A, Olivero A, et al. A randomized 40 arm multicenter study of interferon alfa-2b plus ribavirin in the treatment of patients with chronic hepatitis C not responding to interferon alone. Hepatology 2001; 34: 133–8
Abergel A, Bonny C, Henquell C, et al. Treatment of severe hepatitis C: interferon + ribavirin vs interferon [abstract]. J Hepatol 1999; 30 Suppl. 1: 124
Bellobuono A, Tempini S, Idéo GM, et al. IFN-α and ribavirin combination therapy reduces the occurrence of breakthrough in chronic hepatitis C [abstract no. P/C06/60]. J Hepatol 2000; 32 Suppl. 2: 111
Bernatik T, Klinker H, Scheurlen M, et al. Interferon/ribavirin combination therapy with and without daily dosing in retreatment of chronic hepatitis C [abstract no. C06/042]. J Hepatol 2000; 32 Suppl. 2: 187
Bjøro K, Bell H, Helium KB, et al. Rapid viral clearance with IFN-α 2b induction therapy and ribavirin for chronic HCV infection [abstract]. J Hepatol 2000; 32 Suppl. 2: 38
Bradley L, Freilich M, Nightengale A, et al. Intron A + ribavirin induction therapy for treatment of community patients with chronic hepatitis C not previously treated with interferon [abstract no. 6532]. Gastroenterology 2000; 118 Suppl. 2 Pt. 2: A1440
Chemello L, Cavalletto L, Bernardinello E, et al. Retreatment of chronic hepatitis C (CHC) with sequential interferon-ribavirin combination (INF-RIBA) therapy [abstract no. P/C06/005]. J Hepatol 1998; 28 Suppl. 1: 109
Dettmer RM, Aytaman A, Bloom AA, et al. Multicenter, placebo-controlled, double-blind trial of interferon α-2B plus ribavirin vs. interferon alone for retreatment of non-responders and relapsers with chronic hepatitis C who have failed previous treatment with interferon: a 48 week review [abstract]. Hepatology 1999 Oct; 30 Suppl. Pt.2: 201
Fehér J, Lengyel G, Bálint T, et al. The efficacy of combined interferon-alfa-2B and ribavirin therapy in patients with chronic hepatitis C: final reports of a multicenter study with 100 patients in Hungary [abstract]. J Hepatol 2000; 32 Suppl. 2: 202
Fehér J, Lengyel G. Combined interferon and ribavirin therapy in patients with chronic hepatitis C. Preliminary results of a prospective multicenter study [abstract]. Z Gastroenterol 1998 May; 36: 422
Ferenci P, Kopty C, Vogel W, et al. Effect of initial interferon dosing and dose on early response to combination therapy with ribavirin in chronic hepatitis C [abstract]. J Hepatol 1999; 30 Suppl. 1: 123
Gabbay J, Hofmann CM, Shiftman ML, et al. Interferon (IFN) and ribavirin (RVN) for treatment (TX) of chronic HCV in IFN non-responders (NRs) [abstract no. 284]. Am J Gastroenterol 1998; 93(9): 1680
Gallego A, Garcia-Samaniego J, Diago M, et al. Retreatment with IFN alfa 2B + ribavirin (24 vs 48 weeks) for patients with chronic hepatitis C who relapsed or did not respond to IFN alone [abstract]. J Hepatol 2000; 32 Suppl. 2: 107
Kwo PY, Fields S, Chalasani N, et al. Alfa-interferon with ribavirin for the treatment of chronic hepatitis C in treatment naive patients [abstract no. 6616]. Gastroenterology 2000; 118(4) Suppl. 2 (Pt 2): A1459
Lewis JH, Collier KP, Epstein MS, et al. Does race predict outcome in intron-A plus ribavirin (rebetron) for the treatment of chronic hepatitis C in prior interferon monotherapy non-responders? Results of the Washington, DC Metropolitan Area Hepatitis C Investigators Study [abstract]. Gastroenterology 2000 Apr; 118 Suppl. 2 (Pt 2): 1463
Lewis JH, Carroll J, Epstein MS, et al. Intron A plus ribavirin for the treatment of chronic hepatitis C in prior interferon monotherapy non-responders and relapsers: results of the Washington, DC Metropolitan Area Hepatitis C Investigators Study [abstract]. Gastroenterology 1999 Apr; 116 Pt 2: 75
Lewis JH, Collier KP, Epstein MS, et al. Intron-A plus ribavirin (Rebetron) for the treatment of chronic hepatitis C in prior interferon monotherapy non-responders (NRS): final results of the Washington, DC Metropolitan Area Hepatitis C Investigators Study [abstract no. 6633]. Gastroenterology 2000; 118 Suppl. 2 (Pt 2): A1464
Sievert W, Batey R, Reed W, et al. Efficacy, safety and tolerability of daily, high dose interferon α-2B with or without ribavirin for retreatment of HCV infected patients who did not respond to initial interferon monotherapy: an interim report of the AusHep 6 study [abstract]. Hepatology 1999 Oct; 30 Suppl. (Pt 2): 268A
Steindl-Munda PJ, Kopty DC, Ferenci P, et al. Retreatment of IFN nonresponders or relapsers with chronic hepatitis C with high dose interferon in combination with ribavirin [abstract]. J Hepatol 2000; 32 Suppl. 2: 103
Sulkowski MS, Ball LM, Tice AD, et al. Antiviral efficacy and safety of ribavirin with daily versus TIW interferon A-2B for chronic HCV infection [abstract]. Gastroenterology 2000 Apr; 118 Suppl. 2 (Pt 2): A1492
Salmeron J, Vivaldi RM, De la Mata M, et al. Interferon alfa plus ribavirin in chronic hepatitis C relapsers and non-responders to previous interferon alfa course [abstract]. J Hepatol 2000; 32 Suppl. 2: 185
Sarabanchong V, Reinus J, Clain DJ, et al. Double-blind, placebo-controlled trial of interferon α-2b plus ribavirin versus interferon α-2b for retreatment of patients with chronic hepatitis C who failed previous treatment with interferon alpha [abstract]. Hepatology 1998 Oct; 28 Suppl. (Pt 2): 703A
Renner-Schneiter EC, Dufour J-F, Fried R, et al. Interferon-α (IFN) induction dosing and ribavirin (R) in IFN non-responders (NR) with chronic hepatitis C (CHC): interim analysis of an ongoing study (SASL 10) [abstract no. P/C06/30]. J Hepatol 2000; 32 Suppl. 2: 104
Portal I, Bourlière M, Halfen P, et al. Retreatment with interferon-ribavirin according to viremia of interferon responderrelapser patients: French multicenter randomized controlled study [abstract]. J Hepatol 2000; 32 Suppl. 2: 97
Pimstone NR, Canio JB, Powell JS, et al. Virologic response in re-treatment of chronic responders (NR) and responder-relapsers (RR): INF induction followed by combination ribavirin vs combination ribavirin: high dose IFN (780 MIU/52 weeks) [abstract no. 1589]. Hepatology 2000; 32 Pt 2: 557
Monsour H, Mailliard M, Abou-Awdi N, et al. Preliminary analysis of a multicenter trial of ribavirin plus interferon α-2b previous predictors of response invalidated [abstract]. Hepatology 1998 Oct; 28 Suppl. (Pt 2): 577A
Mangia A, Villani MR, Minerva N, et al. End of therapy response in naive pts: 6MU IFN α-2B + ribavirin vs IFN α-2B 6MU alone [abstract]. J Hepatol 1999; 30 Suppl. 1: 137
Min AD, Jones JL, Lebovics E, et al. Interferon alfa-2B and ribavirin in patients with resistant chronic hepatitis C [abstract]. Hepatology 1999 Oct; 30 Suppl. (Pt 2): 192A
Pimstone NR, Canio JB, Chiang MH, et al. Ribavirin/interferon α-2b (IFN) therapy is very effective in the treatment of chronic hepatitis C genotype 2 and 3 patients who have failed to respond virologically to IFN monotherapy [abstract no. 1961]. Gastroenterology 2001; 120 Suppl. 1: 382
Pimstone NR, Canio JB, Chiang MH, et al. Re-treatment virologic response in chronic hepatitis C virologic non-responders (NR) and responder-relapsers (RR) to interferon (IFN) monotherapy: IFN α-2b induction followed by combination ribavirin/interferon α-2b vs combination ribavirin/interferon α-2b (780 MIU/52 weeks Rebetron therapy) [abstract no. 2885]. Gastroenterology 2001; 120 Suppl. 1: A568
Lebovics E, Castillo E, Rampersaud P, et al. Induction interferon α-2b 5MU daily for 4 weeks followed by combination interferon-ribavirin versus interferon-ribavirin without induction therapy for previously untreated chronic hepatitis C [abstract no. 2899]. Gastroenterology 2001; 120 Suppl. 1: A570
Lawitz EJ, Kadakia SC, Jeffries M, et al. Continuous combination therapy has superior viral clearance compared to standard combination therapy: a multicenter, randomised trial [abstract no. 1954]. Gastroenterology 2001; 120 Suppl. 1: A381
Reichard O, Norkrans G, Frydén A, et al. Randomised, double-blind, placebo-controlled trial of interferon α-2b with and without ribavirin for chronic hepatitis C. Lancet 1998 Jan 10; 351: 83–7
Lo Iacono O, Castro A, Diago M, et al. Interferon alfa-2b plus ribavirin for chronic hepatitis C patients who have not responded to interferon monotherapy. Aliment Pharmacol Ther 2000 Apr; 14: 463–9
Brouwer JT, Hansen BE, Niesters HGM, et al. Early prediction of response in interferon monotherapy and in interferonribavirin combination therapy for chronic hepatitis C: HCV RNA at 4 weeks versus ALT. J Hepatol 1999 Feb; 30: 192–8
Ferenci P, Stauber R, Steindl-Munda P, et al. Interim analysis of a randomized controlled trial of combination of ribavirin and high dose interferon-α in interferon nonresponders with chronic hepatitis C. J Viral Hepatitis 1999 Jul; 6 Suppl. 1: 53–8
Barbaro G, Di Lorenzo G, Soldini M, et al. Intravenous recombinant interferon-beta versus interferon-α-2b and ribavirin in combination for short-term treatment of chronic hepatitis C patients not responding to interferon-a. Scand J Gastroenterol 1999 Sep; 34: 928–33
Min AD, Jones JL, Esposito S, et al. Efficacy of high-dose interferon in combination with ribavirin in patients with chronic hepatitis C resistant to interferon alone. Am J Gastroenterol 2001; 96(4): 1143–9
Shiffman ML, Hofmann CM, Gabbay J, et al. Treatment of chronic hepatitis C in patients who failed interferon monotherapy: effects of higher doses of interferon and ribavirin combination therapy. Am J Gastroenterol 2000; 95: 2928–35
Mangia A, Villani MR, Minerva N, et al. Efficacy of 5MU of interferon in combination with ribavirin for naive patients with chronic hepatitis C virus: a randomized controlled trial. J Hepatol 2001; 34: 441–6
Christensson B, Wiebe T, Åkesson A, et al. Interferon-α and ribavirin treatment of hepatitis C in children with malignancy in remission. Clin Infect Dis 2000 Mar; 30: 585–6
Koretz RL. Making end points meet. Gastroenterology 1999 May; 116: 1266–7
Davis GL, Lau JYN. Choice of appropriate end points of response to interferon therapy in chronic hepatitis C virus infection. J Hepatol 1995; 22 Suppl. 1: 110–4
McHutchinson JG, Poynard T, Davis GI, et al. Evaluation of hepatic HCV RNA before and after treatment with interferon alfa 2b or combined with ribavirin in chronic hepatitis [abstract no. 810]. Hepatology 1999; 30 Pt 2: 363A
Knodell RG, Ishak KG, Black WC, et al. Formulation and application of a numerical scoring system for assessing histological activity in asymptomatic chronic active hepatitis. Hepatology 1981; 1(5): 431–5
Bedossa P, Poynard T. An algorithm for the grading of activity in chronic hepatitis C. Hepatology 1996; 24: 289–93
Poynard T, McHutchinson J, Davis GL, et al. Impact of interferon alfa-2b and ribavirin on progression of liver fibrosis in patients with chronic hepatitis C. Hepatology 2000; 32: 1131–7
Brillanti S, Levantesi F, Masi L, et al. Triple antiviral therapy as a new option for patients with interferon nonresponsive chronic hepatitis C. Hepatology 2000 Sep; 32: 630–4
Mazzaferro V, Regalia E, Pulvirenti A, et al. Prophylaxis against HCV recurrence after liver transplantation: effect of interferon and ribavirin combination. Transplant Proc 1997 Feb–Mar; 29: 519–21
Ben-Ari Z, Mor E, Shaharabani E, et al. Combination of interferon-α and ribavirin therapy for recurrent hepatitis C virus infection after liver transplantation. Transplant Proc 2000; 32: 714–6
Gopal DV, Rabkin JM, Berk BS, et al. Treatment of progressive hepatitis C recurrence after liver transplantation with combination interferon plus ribavirin. Liver Transpl 2001; 7(3): 181–90
Nasti G, Di Gennaro G, Rizzardini G, et al. Chronic hepatitis C in HIV-coinfected patients: feasibility and efficacy of interferon-a-2b and ribavirin combination therapy. J Acquir Immune Defic Syndr 2001; 26(3): 299–300
Schalm SW, Brouwer JT. Antiviral therapy of hepatitis C. Scand J Gastroenterol 1997; 32 Suppl. 223: 46–9
Davis GL, Lau JYN. Factors predictive of a beneficial response to therapy of hepatitis C. Hepatology 1997 Sep; 26 Suppl. 1: 122S–7S
Reddy KR, Hoofnagle JH, Tong MJ, et al. Racial differences in responses to therapy with interferon in chronic hepatitis C. Hepatology 1999; 30(3): 787–93
Van Der Poel CL, Cuypers HT, Reesink HW. Hepatitis C virus six years on. Lancet 1994; 344: 1475–9
Gordon SC, Fang JW, Silverman AL, et al. The significance of baseline serum alanine aminotransferase on pretreatment disease characteristics and response to antiviral therapy in chronic hepatitis C. Hepatology 2000 Aug; 32: 400–4
McHutchinson JG, Poynard T, Pianko S, et al. The impact of interferon plus ribavirin on response to therapy in Black patients with chronic hepatitis C. Gastroenterology 2000; 119: 1317–23
Bonkovsky HL, Woolley JM. Reduction of health-related quality of life in chronic hepatitis C and improvement with interferon therapy. Consensus Interferon Study Group. Hepatology 1999; 29: 264–70
Bayliss MS, Gandek B, Bungay KM, et al. A questionnaire to assess the generic and disease-specific health outcomes of patients with chronic hepatitis C. Qual Life Res 1998; 7: 39–55
Ware Jr JE, Bayliss MS, Mannocchia M, et al. Health-related quality of life in chronic hepatitis C: impact of disease and treatment response. Hepatology 1999; 30: 550–5
McHutchinson JG, Ware Jr JE, Bayliss MS, et al. The effects of interferon alfa-2b in combination with ribavirin on health related quality of life and work productivity. J Hepatol 2001; 34: 140–7
Koff RS. Therapy of hepatitis C: cost-effectiveness analysis. Hepatology 1997; 26 Suppl. 1: 152–5
Koff RS. Cost-effectiveness of treatment for chronic hepatitis C. J Hepatol 1999; 31 Suppl. 1: 255–8
Koff RS. Cost-effectiveness of combined interferon and ribavirin versus interferon alone. Clin Liver Dis 1999; 3(4): 827–41
Wong JB, Poynard T, Ling M-H, et al. Cost-effectiveness of 24 or 48 weeks of interferon α-2b alone or with ribavirin as initial treatment of chronic hepatitis C. Am J Gastroenterol 2000 Jun; 95: 1524–30
Wong JB, Davis GL, Pauker SG. Cost effectiveness of ribavirin/interferon alfa-2b after interferon relapse in chronic hepatitis C. Am J Med 2000 Apr 1; 108: 366–73
Younossi ZM, Singer ME, McHutchison JG, et al. Cost effectiveness of interferon a-2b combined with ribavirin for the treatment of chronic hepatitis C. Hepatology 1999 Nov; 30: 1318–24
Bennett WG, Inoue Y, Beck R, et al. Estimates of the costeffectiveness of a single course of interferon-α 2b in patients with histologically mild chronic hepatitis C. Ann Intern Med 1997; 127: 855–65
Wong JB, Bennett WG, Koff RS, et al. Pretreatment evaluation of chronic hepatitis C: risks, benefits and costs. JAMA 1998; 280: 2088–93
Yano M, Kumada H, Kage M, et al. The long-term pathological evolution of chronic hepatitis C. Hepatology 1996; 23: 1334–40
Fattovich G, Giustina G, Degos F, et al. Morbidity and mortality in compensated cirrhosis type C: a retrospective follow-up study of 384 patients. Gastroenterology 1997; 112: 463–72
Kim WR, Poterucha JJ, Hermans JE, et al. Cost-effectiveness of 6 and 12 months of interferon-α therapy for chronic hepatitis C. Ann Intern Med 1997; 127: 866–74
Tsukuma H, Hiyama T, Tanaka S, et al. Risk factors for hepatocellular carcinoma among patients with chronic liver disease. N Engl J Med 1993; 328: 1797–801
Colombo M, De Franchis R, Nino ED, et al. Hepatocellular carcinoma in Italian patients with cirrhosis. N Engl J Med 1991; 325(10): 675–80
Younossi AM, Mullen KD, Zakko W, et al. Interferon α-2b and ribavirin vs interferon α-2b and amantadine for chronic hepatitis C (non-responder): a multi-center, randomized, double-blind trial [abstract no. 487]. Hepatology 1998 Oct; 28 Suppl. Pt 2: 284A
Schavrcz R, Ando Y, Sonnerberg A, et al. Combination treatment with interferon-α-2b and ribavirin for chronic hepatitis C in patients who failed to show a sustained response to interferon alone: Swedish experience. J Hepatol 1995; 23 Suppl. 1: 17–21
Haria M, Benfield P. Interferon-α-2a: a review of its pharmacological properties and therapeutic use in the management of viral hepatitis. Drugs 1995 Nov; 50: 873–96
Poynard T, Leroy V, Cohard M, et al. Meta-analysis of interferon randomized trials in the treatment of viral hepatitis C: effects of dose and duration. Hepatology 1996; 24: 778–89
Maddrey WC. Safety of combination interferon alfa-2b/ribavirin therapy in chronic hepatitis C-relapsed and treatmentnaive patients. Semin Liver Dis 1999; 19 Suppl. 1: 67–75
Schering Corporation. Rebetron prescribing information. Kentucky, New Jersey, USA, 1998
Carella C, Mazziotti G, Morisco F, et al. Long-term outcome of interferon-α-induced thyroid autoimmmunity and prognostic influence of thyroid autoantibody pattern at the end of treatment. J Clin Endocrinol Metab 2001; 86: 1925–9
Deutsch M, Dourakis S, Manesis EK, et al. Thyroid abnormalities in chronic viral hepatitis and their relationship to interferon alfa therapy. Hepatology 1997; 26: 206–10
Dumoulin FL, Leifeld L, Sauerbruch T, et al. Autoimmunity induced by interferon-a therapy for chronic viral hepatitis. Biomed Pharmacother 1999; 53: 242–54
Fernandez-Soto L, Gonzalez A, Escobar-Jimenez F, et al. Increased risk of autoimmune thyroid disease in hepatitis C vs hepatitis B before, during and after discontinuing interferon therapy. Arch Intern Med 1998; 158: 1445–8
Bhatti AM, McGarrity TJ, Gabbay R, et al. Diabetic ketoacidosis induced by interferon alfa and ribavirin in the patient with hepatitis C [abstract no. 524]. Am J Gastroenterol 2000; 95(9): 2564
Bonkovsky HL. Therapy of hepatitis C: other options. Hepatology 1997 Sep; 26 Suppl. 1: 143S–51S
Gish RG. Future directions in the treatment of patients with chronic hepatitis C virus infection. Can J Gastroenterol 1999 Jan–Feb; 13: 57–62
Schering-Plough Corporation, Enzon. Schering-Plough Corporation (SGP) and Enzon (ENZN) announces PEG-Intron and rebetrol combination therapy receives FDA approval for the treatment of chronic hepatitis C; ENZN stock is up +9.1 % on Wednesday at 10:00 am EST [online]. Available from URL: http://www.schering-plough.com [Accessed 2002 Jan 15]
Shiffman ML. Pegylated interferons: what role will they play in the treatment of chronic hepatitis C? Curr Gastro Rep 2001; 3: 30–7
Glue P, Rouzier-Panis R, Raffanel C, et al. A dose-ranging study of pegylated interferon alfa-2b and ribavirin in chronic hepatitis C. Hepatology 2000; 32: 647–53
Lindsay KL, Trepo C, Heintges T, et al. A randomised, double-blind trial comparing pegylated interferon alfa-2b to interferon alfa-2b as initial treatment for chronic hepatitis C. Hepatology 2001; 34: 395–403
Manns MP, McHutchinson JG, Gordon SC, et al. Peginterferon alfa-2b plus ribavirin compared with interferon alfa-2b plus ribavirin for initial treatment of chronic hepatitis C: a randomised trial. Lancet 2001; 358: 958–65
Collier J, Chapman R. Combination therapy with interferon-α and ribavirin for hepatitis C: practical treatment issues. Biodrugs 2001; 15(4): 225–38
US Department of Veterans Affairs. Hepatitis C: treatment guidelines [online]. Available from URL: http://www.va.gov/heapatitisc/mdtreatl.htm [Accessed 2001 Jan 9]
Canadian Consensus Conference Rapporteur Group. Canadian Consensus Conference on the management of viral hepatitis. Can J Gastroenterol 2000; 14 Suppl. B: 5–20B
Consensus Panel. EASL International Consensus Conference on Hepatitis C. J Hepatol 1999 May; 30: 956–61
Author information
Authors and Affiliations
Corresponding author
Additional information
Various sections of the manuscript reviewed by: B. Christensson, Lund University Hospital, Lund, Sweden; S. Kakamu, Aichi Medical University, Aichi, Japan; J.G. McHutchinson, Scripps Clinic, Division of Gastroenterology/Hepatology, La Jolla, California, USA; G. Mieli-Vergani, King’s College and St. Thomas’ Hospitals’ Medical and Dental School, London, England; R. Sterling, Medical School of Virginia, Richmond, Virginia, USA; M. L. Shiffman, Medical School of Virginia, Richmond, Virginia, USA.
Data Selection
Sources: Medical literature published in any language since 1983 on interferon-alpha-2B/ribavirin, identified using Medline and EMBASE, supplemented by AdisBase (a proprietary database of Adis International). Additional references were identified from the reference lists of published articles. Bibliographical information, including contributory unpublished data, was also requested from the company developing the drug.
Search strategy: Medline search terms were ‘interferon-alpha-2B and ribavirin’. EMBASE search terms were ‘interferon-alpha-2B and Ribavirin’. AdisBase search terms were ‘interferon-alpha-2B and ribavirin’. Searches were last updated 14 January 2002.
Selection: Studies in patients with chronic hepatitis C who received subcutaneous interferon-α-2b plus oral ribavirin combination therapy. Inclusion of studies was based mainly on the methods section of the trials. When available, large, well controlled trials with appropriate statistical methodology were preferred. Relevant pharmacodynamic and pharmacokinetic data are also included.
Index terms: chronic hepatitis C, pharmacodynamics, pharmacokinetics, therapeutic use.
Rights and permissions
About this article
Cite this article
Scott, L.J., Perry, C.M. Interferon-α-2b Plus Ribavirin. Drugs 62, 507–556 (2002). https://doi.org/10.2165/00003495-200262030-00009
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-200262030-00009