Abstract
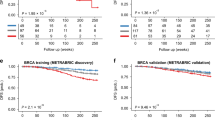
Nischarin has been demonstrated to have tumor suppressor functions. In this review, we comprehensively discuss up to date information about Nischarin. In addition, this paper aims to report the prognostic value, clinical relevance, and biological significance of the Nischarin gene (NISCH) in breast cancer (BCa) patients using the Molecular Taxonomy of Breast Cancer International Consortium (METABRIC) and The Cancer Genome Atlas (TCGA) datasets. We evaluated NISCH gene expression and its correlation to patient survival, baseline expression, and expression variation based on age groups, tumor stage, tumor size, tumor grade, and lymph node status in different subtypes of BCa. Since NISCH has been extensively reported to inhibit EMT and cancer cell migration, we also checked for the correlation between NISCH and EMT genes in addition to the correlation between NISCH and cell migration genes. Our results indicate that NISCH is a tumor suppressor that plays a critical role in BCa initiation, progression, and tumor development. We find that there is a higher level of NISCH expression in normal breast tissues compared to breast cancer tissues. Also, aggressive subtypes of breast cancers, such as the triple negative/basal category, have decreased levels of NISCH as the disease progresses. Finally, we report that NISCH is inversely correlated with many EMT and cancer cell migration genes in BCa. Interestingly, we identified a significant negative correlation between NISCH expression and its methylation in breast cancer patients. Overall, the goal of this report is to establish a strong clinical basis for further investigation into the cellular, molecular, and physiological roles of NISCH in BCa. Ultimately, NISCH gene expression might be clinically harnessed as a biomarker or predictor of invasiveness and metastasis in BCa.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 50 print issues and online access
$259.00 per year
only $5.18 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Alahari SK, Lee JW, Juliano RL. Nischarin, a novel protein that interacts with the integrin α5 subunit and inhibits cell migration. J Cell Biol. 2000;151:1141–54.
Maziveyi M, Alahari SK. Breast cancer tumor suppressors: a special emphasis on novel protein nischarin. Cancer Res. 2015;75:4252–9.
Baranwal S, Wang Y, Rathinam R, Lee J, Jin L, McGoey R, et al. Molecular characterization of the tumor-suppressive function of nischarin in breast cancer. J Natl Cancer Inst. 2011;103:1513–28.
Jain P, Baranwal S, Dong S, Struckhoff AP, Worthylake RA, Alahari SK. Integrin-binding protein nischarin interacts with tumor suppressor liver kinase B1 (LKB1) to regulate cell migration of breast epithelial cells. J Biol Chem. 2013;288:15495–509.
Ding Y, Zhang R, Zhang K, Lv X, Chen Y, Li A, et al. Nischarin is differentially expressed in rat brain and regulates neuronal migration. PLoS ONE. 2013;8:e54563.
Ding Y, Li Y, Lu L, Zhang R, Zeng L, Wang L, et al. Inhibition of nischarin expression promotes neurite outgrowth through regulation of PAK activity. PLoS ONE. 2015;10:e0144948.
Maziveyi M, Dong S, Baranwal S, Mehrnezhad A, Rathinam R, Huckaba TM, et al. Exosomes from nischarin-expressing cells reduce breast cancer cell motility and tumor growth. Cancer Res. 2019;79:2152–66.
McAndrews KM, Kalluri R. Nischarin regulates secretion of exosomes and cancer progression. Cancer Res. 2019;79:2099–101.
Cai Y-J, Ma B, Wang M-L, Chen J, Zhao F-G, Zhou J-D, et al. Impact of Nischarin on EMT regulators in breast cancer cell lines. Oncol Lett. 2020;20:1–1.
Dong S, Ruiz‐Calderon B, Rathinam R, Eastlack S, Maziveyi M, Alahari SK. Knockout model reveals the role of Nischarin in mammary gland development, breast tumorigenesis and response to metformin treatment. Int J cancer. 2020;146:2576–87.
Maziveyi M, Dong S, Baranwal S, Alahari SK. Nischarin regulates focal adhesion and Invadopodia formation in breast cancer cells. Mol cancer. 2018;17:1–11.
Eastlack SC, Dong S, Mo YY, Alahari SK. Expression of long noncoding RNA MALAT1 correlates with increased levels of Nischarin and inhibits oncogenic cell functions in breast cancer. PLoS ONE. 2018;13:e0198945.
Guo Z, Yuan Y, Guo Y, Wang H, Song C, Huang M. Nischarin attenuates apoptosis induced by oxidative stress in PC12 cells. Exp therapeutic Med. 2019;17:663–70.
Ding Y, Milosavljevic T, Alahari SK. Nischarin inhibits LIM kinase to regulate cofilin phosphorylation and cell invasion. Mol Cell Biol. 2008;28:3742–56.
Chang C, Wei W, Han D, Meng J, Zhu F, Xiao Y, et al. Expression of Nischarin negatively correlates with estrogen receptor and alters apoptosis, migration and invasion in human breast cancer. Biochemical biophysical Res Commun. 2017;484:536–42.
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2021. CA: a cancer J clinicians. 2021;71:7–33.
Tsang J, Tse GM. Molecular classification of breast cancer. Adv Anat Pathol. 2020;27:27–35.
Nagini S. Breast cancer: current molecular therapeutic targets and new players. Anti-Cancer Agents Medicinal Chem (Former Curr Medicinal Chem-Anti-Cancer Agents). 2017;17:152–63.
Piletz JE, Jones JC, Zhu H, Bishara O, Ernsberger P. Imidazoline receptor antisera-selected cDNA clone and mRNA distribution. Ann N. Y Acad Sci. 1999;881:1–7.
Ostrow KL, Hoque MO, Loyo M, Brait M, Greenberg A, Siegfried JM, et al. Molecular analysis of plasma DNA for the early detection of lung cancer by quantitative methylation-specific PCR. Clin Cancer Res. 2010;16:3463–72.
Lim KP, Hong W. Human Nischarin/imidazoline receptor antisera-selected protein is targeted to the endosomes by a combined action of a PX domain and a coiled-coil region. J Biol Chem. 2004;279:54770–82.
Kuijl C, Pilli M, Alahari SK, Janssen H, Khoo PS, Ervin KE, et al. Rac and Rab GTPases dual effector Nischarin regulates vesicle maturation to facilitate survival of intracellular bacteria. EMBO J. 2013;32:713–27.
Jin L, Wessely O, Marcusson EG, Ivan C, Calin GA, Alahari SK. Prooncogenic factors miR-23b and miR-27b are regulated by Her2/Neu, EGF, and TNF-α in breast cancer. Cancer Res. 2013;73:2884–96.
Zhang L, Zhao TY, Hou N, Teng Y, Cheng X, Wang B, et al. Generation and primary phenotypes of imidazoline receptor antisera-selected (IRAS) knockout mice. CNS Neurosci Ther. 2013;19:978–81.
Li F, Wu N, Su R, Chen Y, Lu X, Liu Y, et al. Imidazoline receptor antisera-selected/Nischarin regulates the effect of agmatine on the development of morphine dependence. Addict Biol. 2012;17:392–408.
Crompton M, Purnell T, Tyrer HE, Parker A, Ball G, Hardisty-Hughes RE, et al. A mutation in Nischarin causes otitis media via LIMK1 and NF-kappaB pathways. PLoS Genet. 2017;13:e1006969.
Dong S, Baranwal S, Garcia A, Serrano-Gomez SJ, Eastlack S, Iwakuma T, et al. Nischarin inhibition alters energy metabolism by activating AMP-activated protein kinase. J Biol Chem. 2017;292:16833–46.
Dong S, Bluher M, Zhang Y, Wu H, Alahari SK. Development of insulin resistance in Nischarin mutant female mice. Int J Obes (Lond). 2019;43:1046–57.
Chen J, Feng WL, Mo WJ, Ding XW, Xie SN. Expression of integrin-binding protein Nischarin in metastatic breast cancer. Mol Med Rep. 2015;12:77–82.
Li J, He X, Dong R, Wang Y, Yu J, Qiu H. Frequent loss of NISCH promotes tumor proliferation and invasion in ovarian cancer via inhibiting the FAK signal pathway. Mol Cancer Ther. 2015;14:1202–12.
Zhao Y, Liang X, Zhu F, Wen Y, Xu J, Yang J, et al. A large-scale integrative analysis of GWAS and common meQTLs across whole life course identifies genes, pathways and tissue/cell types for three major psychiatric disorders. Neurosci Biobehav Rev. 2018;95:347–52.
Rathnam C, Lee S, Jiang X. An algorithm for direct causal learning of influences on patient outcomes. Artif Intell Med. 2017;75:1–15.
Geng R, Wang Q, Chen E, Zheng QY. Current understanding of host genetics of otitis media. Front Genet. 2019;10:1395.
Zhang J, Abdel-Rahman AA. Inhibition of nischarin expression attenuates rilmenidine-evoked hypotension and phosphorylated extracellular signal-regulated kinase 1/2 production in the rostral ventrolateral medulla of rats. J Pharm Exp Ther. 2008;324:72–78.
Wu N, Su RB, Liu Y, Lu XQ, Zheng JQ, Cong B, et al. Modulation of agmatine on calcium signal in morphine-dependent CHO cells by activation of IRAS, a candidate for imidazoline I1 receptor. Eur J Pharm. 2006;548:21–28.
Li F, Wu N, Su RB, Zheng JQ, Xu B, Lu XQ, et al. Involvement of phosphatidylcholine-selective phospholipase C in activation of mitogen-activated protein kinase pathways in imidazoline receptor antisera-selected protein. J Cell Biochem. 2006;98:1615–28.
Chen MJ, Zhu HE, Piletz JE. Intracellular effect of imidazoline receptor on alpha(2A)-noradrenergic receptor. Ann N. Y Acad Sci. 2003;1009:427–38.
Li S, Wu N, Zhao TY, Lu GY, Wang ZY, Li F, et al. The role of IRAS/Nischarin involved in the development of morphine tolerance and physical dependence. Biochem Biophys Res Commun. 2019;512:460–6.
Li F, Ma H, Wu N, Li J. IRAS modulates opioid tolerance and dependence by regulating mu opioid receptor trafficking. Mol Neurobiol. 2016;53:4918–30.
Amisten S, Duner P, Asplund O, Mohammed Al-Amily I, Groop L, Salehi A. Activation of imidazoline receptor I2, and improved pancreatic beta-cell function in human islets. J Diabetes Complications. 2018;32:813–8.
Lin MH, Hsu CC, Lin J, Cheng JT, Wu MC. Investigation of morin-induced insulin secretion in cultured pancreatic cells. Clin Exp Pharm Physiol. 2017;44:1254–62.
Hotta K, Kitamoto A, Kitamoto T, Mizusawa S, Teranishi H, So R, et al. Replication study of 15 recently published Loci for body fat distribution in the Japanese population. J Atheroscler Thromb. 2013;20:336–50.
Heid IM, Jackson AU, Randall JC, Winkler TW, Qi L, Steinthorsdottir V, et al. Meta-analysis identifies 13 new loci associated with waist-hip ratio and reveals sexual dimorphism in the genetic basis of fat distribution. Nat Genet. 2010;42:949–60.
Uren C, Henn BM, Franke A, Wittig M, van Helden PD, Hoal EG, et al. A post-GWAS analysis of predicted regulatory variants and tuberculosis susceptibility. PLoS One. 2017;12:e0174738.
Keller B, Garcia-Sevilla JA. Effects of I2-imidazoline receptor (IR) alkylating BU99006 in the mouse brain: Upregulation of nischarin/I1-IR and mu-opioid receptor proteins and modulation of associated signalling pathways. Neurochem Int. 2017;108:169–76.
Nagakura Y, Ide R, Saiki C, Sato Hashizume N, Imai T. Expression of nischarin, an imidazoline 1 receptor candidate protein, in the ventrolateral medulla of newborn rats. Neurosci Lett. 2021;761:136113.
Wu X, Xu W, Cui G, Yan Y, Wu X, Li L, et al. The expression pattern of Nischarin after lipopolysaccharides (LPS)-induced neuroinflammation in rats brain cortex. Inflamm Res. 2013;62:929–40.
Keller B, Mestre-Pinto JI, Alvaro-Bartolome M, Martinez-Sanvisens D, Farre M, Garcia-Fuster MJ, et al. A biomarker to differentiate between primary and cocaine-induced major depression in cocaine use disorder: the role of platelet IRAS/Nischarin (I1-imidazoline receptor). Front Psychiatry. 2017;8:258.
Keller B, Garcia-Sevilla JA. Dysregulation of IRAS/nischarin and other potential I1-imidazoline receptors in major depression postmortem brain: downregulation of basal contents by antidepressant drug treatments. J Affect Disord. 2017;208:646–52.
Ding YM, Li YY, Wang C, Huang H, Zheng CC, Huang SH, et al. Nischarin-siRNA delivered by polyethylenimine-alginate nanoparticles accelerates motor function recovery after spinal cord injury. Neural Regen Res. 2017;12:1687–94.
Wiatrak B, Kubis-Kubiak A, Piwowar A, Barg E. PC12 Cell line: cell types, coating of culture vessels, differentiation and other culture conditions. Cells. 2020;9:1–76.
Guo Z, Huang M, Yuan Y, Guo Y, Song C, Wang H, et al. Nischarin downregulation attenuates cell injury induced by oxidative stress via Wnt signaling. Neuroreport. 2020;31:1199–207.
McGuire A, Brown JA, Malone C, McLaughlin R, Kerin MJ. Effects of age on the detection and management of breast cancer. Cancers. 2015;7:908–29.
Shaw RJ, Bardeesy N, Manning BD, Lopez L, Kosmatka M, DePinho RA, et al. The LKB1 tumor suppressor negatively regulates mTOR signaling. Cancer Cell. 2004;6:91–99.
Acknowledgements
We wish to thank the Fred G. Brazda Foundation and the Department of Biochemistry and Molecular Biology, Louisiana State University School of Medicine and Health Sciences Center, New Orleans, for their financial support.
Author information
Authors and Affiliations
Contributions
SO wrote the first draft, HY did bioinformatic analysis and prepared figures, KN, NA, BB, MB contributed to the text, TC created some figures, and SKA finalized the text and figures.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Okpechi, S.C., Yousefi, H., Nguyen, K. et al. Role of Nischarin in the pathology of diseases: a special emphasis on breast cancer. Oncogene 41, 1079–1086 (2022). https://doi.org/10.1038/s41388-021-02150-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41388-021-02150-4
This article is cited by
-
Identification of a psychiatric risk gene NISCH at 3p21.1 GWAS locus mediating dendritic spine morphogenesis and cognitive function
BMC Medicine (2023)
-
Nischarin expression may have differing roles in male and female melanoma patients
Journal of Molecular Medicine (2023)