Abstract
Background
Aspirin resistance is defined by platelet function testing and presumed clinical unresponsiveness to aspirin. Aspirin-resistant patients are at a greater risk of clinically important adverse cardiovascular events. We aimed to investigate whether end-stage renal disease patients with aspirin resistance are at increased risk for long-term major adverse clinical events.
Methods
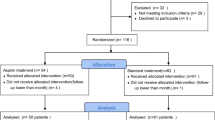
We prospectively enrolled 78 end-stage renal disease patients between January 2008 and November 2008. The effect of aspirin on platelet functions was determined using a new generation impedance aggregometer (Multiplate analyser, Dynabyte Medical, Munich). The primary end-point was the composite of death, myocardial infarction, unstable angina, or cerebrovascular accident. Mean follow-up was 20.7 ± 6.1 months.
Results
Of the patients studied, 34 (43.58 %) were aspirin resistant and 44 (56.42 %) were not aspirin resistant. Among patients who were aspirin resistant, 13 of 34 (38.2 %) experienced death, MI, or CVA, compared to 7 of 44 (15.9 %) patients who were not aspirin resistant (p = 0.034). Multivariate analyses identified aspirin resistance to be independently associated with major adverse long-term outcomes ([HR] 2.722; 95 % CI, 1.068–6.942; p = 0.04).
Conclusion
This study demonstrates that end-stage kidney disease patients resistant to aspirin are at a greater risk of long-term major adverse events than patients who are sensitive to aspirin.


Similar content being viewed by others
References
Antithrombotic Trialists’ Collaboration (2009) Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials. Lancet 373:1849–1860
Gasparyan AY, Watson T, Lip GY (2008) The role of aspirin in cardiovascular prevention: implications of aspirin resistance. J Am Coll Cardiol 51:1829–1843
National Kidney Foundation (2002) K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis 39:S1–266
Luke RG (1998) Chronic renal failure-a vasculopathic state. N Engl J Med 339:841–843
Krasopoulos G, Brister SJ, Beattie WS, Buchanan MR (2008) Aspirin “resistance” and risk of cardiovascular morbidity: systematic review and meta-analysis. BMJ 336:195–198
Tóth O, Calatzis A, Penz S, Losonczy H, Siess W (2006) Multiple electrode aggregometry: a new device to measure platelet aggregation in whole blood. Thromb Haemost 96:781–788
Sibbing D, Braun S, Jawansky S, Vogt W, Mehilli J, Schömig A, Kastrati A, von Beckerath N (2008) Assessment of ADP-induced platelet aggregation with light transmission aggregometry and multiple electrode platelet aggregometry before and after clopidogrel treatment. Thromb Haemost 99:121–126
von Pape KW, Dzijan-Horn M, Bohner J, Spannagl M, Weisser H, Calatzis A (2007) Control of aspirin effect in chronic cardiovascular patients using two whole blood platelet function assays. PFA-100 and Multiplate. Hamostaseologie 27:155–160
Jámbor C, Weber CF, Gerhardt K, Dietrich W, Spannagl M, Heindl B, Zwissler B (2009) Whole blood multiple electrode aggregometry is a reliable point-of-care test of aspirin-induced platelet dysfunction. Anesth Analg 109:25–31
Chamorro A, Blanc R, Ascaso C, Saiz A, Vila N (1997) Factors associated to aspirin failure for secondary stroke prevention. Med Clin (Barc) 109:569–572
Buchanan MR, Brister SJ (1995) Individual variation in the effects of ASA on platelet function: implications for the use of ASA clinically. Can J Cardiol 11:221–227
Cipollone F, Patrignani P, Greco A, Panara MR, Padovano R, Cuccurullo F, Patrono C, Rebuzzi AG, Liuzzo G, Quaranta G, Maseri A (1997) Differential suppression of thromboxane biosynthesis by indobufen and aspirin in patients with unstable angina. Circulation 96:1109–1116
Grotemeyer KH, Scharafinski HW, Husstedt IW (1993) Two-year follow-up of aspirin responder and aspirin non responder. A pilot-study including 180 post-stroke patients. Thromb Res 71:397–403
Fateh-Moghadam S, Plöckinger U, Cabeza N, Htun P, Reuter T, Ersel S, Gawaz M, Dietz R, Bocksch W (2005) Prevalence of aspirin resistance in patients with type 2 diabetes. Acta Diabetol 42:99–103
Gum PA, Kottke-Marchant K, Welsh PA, White J, Topol EJ (2003) A prospective, blinded determination of the natural history of aspirin resistance among stable patients with cardiovascular disease. J Am Coll Cardiol 41:961–965
Roth GJ, Majerus PW (1975) The mechanism of the effect of aspirin on human platelets. I. Acetylation of a particulate fraction protein. J Clin Invest 56:624–632
Kawasaki T, Ozeki Y, Igawa T, Kambayashi J (2000) Increased platelet sensitivity to collagen in individuals resistant to low-dose aspirin. Stroke 31:591–595
Cambria-Kiely JA, Gandhi PJ (2002) Aspirin resistance and genetic polymorphisms. J Thromb Thrombolysis 14:51–58
Cambria-Kiely JA, Gandhi PJ (2002) Possible mechanisms of aspirin resistance. J Thromb Thrombolysis 13:49–56
Bloom A, Greaves M, Preston FE, Brown CB (1986) Evidence against a platelet cyclooxygenase defect in uraemic subjects on chronic haemodialysis. Br J Haematol 62:143–149
Cavarape A, Bauer J, Bartoli E, Endlich K, Parekh N (2003) Effects of angiotensin II, arginine vasopressin and tromboxane A2 in renal vascular bed: role of rho-kinase. Nephrol Dial Transplant 18:1764–1769
Geara AS, Azzi N, Bassil C, El-Sayegh S (2010) Aspirin resistance in hemodialysis patients. Int Urol Nephrol. doi:10.1007/s11255-010-9811
Yusuf S, Zhao F, Mehta SR, Chrolavicius S, Tognoni G, Fox KK (2001) Clopidogrel in effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N Engl J Med 345:494–502
Steinhubl SR, Berger PB, Mann JT 3rd, Fry ET, DeLago A, Wilmer C, Topol EJ, CREDO Investigators (2002) Clopidogrel for the reduction of events during observation. Early and sustained dual oral antiplatelet therapy following percutaneous coronary intervention: a randomized controlled trial. JAMA 288:2411–2420
Acknowledgments
There is no relationship with industry and financial associations that might pose a conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kilickesmez, K.O., Kocas, C., Abaci, O. et al. Follow-up of aspirin-resistant patients with end-stage kidney disease. Int Urol Nephrol 45, 1097–1102 (2013). https://doi.org/10.1007/s11255-012-0217-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-012-0217-x