Abstract
Dental implant stability, which is an important parameter for the surgical outcome, can now be assessed using quantitative ultrasound. However, the acoustical propagation in dental implants remains poorly understood. The objective of this numerical study was to understand the propagation phenomena of ultrasonic waves in cylindrically shaped prototype dental implants and to investigate the sensitivity of the ultrasonic response to the surrounding bone quantity and quality. The 10-MHz ultrasonic response of the implant was calculated using an axisymetric 3D finite element model, which was validated by comparison with results obtained experimentally and using a 2D finite difference numerical model. The results show that the implant ultrasonic response changes significantly when a liquid layer is located at the implant interface compared to the case of an interface fully bounded with bone tissue. A dedicated model based on experimental measurements was developed in order to account for the evolution of the bone biomechanical properties at the implant interface. The effect of a gradient of material properties on the implant ultrasonic response is determined. Based on the reproducibility of the measurement, the results indicate that the device should be sensitive to the effects of a healing duration of less than one week. In all cases, the amplitude of the implant response is shown to decrease when the dental implant primary and secondary stability increase, which is consistent with the experimental results. This study paves the way for the development of a quantitative ultrasound method to evaluate dental implant stability.







Similar content being viewed by others
References
Aparicio C, Lang NR, Rangert B (2006) Validity and clinical significance of biomechanical testing of implant/bone interface. Clin Oral Implant Res 17:2–7
Arndt C, Voigt C, Steinke H, von Salis-Soglio G, Scholz R (2012) Experimental evidence of impingement induced strains at the interface and the periphery of an embedded acetabular cup implant. J Biomech Eng T ASME 134
Balshi SF, Allen FD, Wolfinger GJ, Balshi TJ (2005) A resonance frequency analysis assessment of maxillary and mandibular immediately loaded implants. Int J Oral Maxillofac Implants 20:584–594
Bardyn T, Gedet P, Hallermann W, Buchler P (2009) Quantifying the influence of bone density and thickness on resonance frequency analysis: an in vitro study of biomechanical test materials. Int J Oral Maxillofac Implants 24:1006–1014
Blanco J, Alvarez E, Munoz F, Linares A, Cantalapiedra A (2011) Influence on early osseointegration of dental implants installed with two different drilling protocols: a histomorphometric study in rabbit. Clin Oral Implants Res 22:92–99
Blanes RJ, Bernard JP, Blanes ZM, Belser UC (2007) A 10-year prospective study of ITI dental implants placed in the posterior region. I: clinical and radiographic results. Clin Oral Implants Res 18:699–706
Capek L, Simunek A, Slezak R, Dzan L (2009) Influence of the orientation of the Osstell transducer during measurement of dental implant stability using resonance frequency analysis: a numerical approach. Med Eng Phys 31:764–769. doi:10.1016/j.medengphy.2009.02.003
Chang MC et al (2003) Elasticity of alveolar bone near dental implant–bone interfaces after one month’s healing. J Biomech 36:1209–1214. doi:10.1016/s0021-9290(03)001133-1
Coelho PG et al (2010) Biomechanical evaluation of endosseous implants at early implantation times: a study in dogs. J Oral Maxillofac Surg 68:1667–1675
de Almeida MS, Maciel CD, Pereira JC (2007) Proposal for an ultrasonic tool to monitor the osseointegration of dental implants. Sensors 7:1224–1237
Franchi M et al (2007) Influence of different implant surfaces on peri-implant osteogenesis: histomorphometric analysis in sheep. J Periodontol 78:879–888
Frost HM (2003) Bone’s mechanostat: a 2003 update. Anat Rec A Discov Mol Cell Evol Biol 275A:1081–1101
Gill A, Shellock FG (2012) Assessment of MRI issues at 3-Tesla for metallic surgical implants: findings applied to 61 additional skin closure staples and vessel ligation clips. J Cardiov Magn Reson 14
Glauser R, Sennerby L, Meredith N, Ree A, Lundgren A, Gottlow J, Hammerle CHF (2004) Resonance frequency analysis of implants subjected to immediate or early functional occlusal loading: successful vs. failing implants. Clin Oral Implant Res 15:428–434
Haïat G, Naili S, Vu MB, Desceliers C, Soize C (2011) Equivalent contributing depth investigated by a lateral wave with axial transmission in viscoelastic cortical bone. J Acoust Soc Am 129:114–120
Haïat G, Naili S, Grimal Q, Talmant M, Desceliers C, Soize C (2009) Influence of a gradient of material properties on ultrasonic wave propagation in cortical bone: application to axial transmission. J Acoust Soc Am 125:4043–4052
Haïat G, Naili S, Vu M-B, Desceliers C, Soize C (2011) Equivalent contributing depth investigated by a lateral wave with axial transmission in heterogeneous viscoelastic cortical bone. J Acoust Soc Am 129:EL114–EL120
Haïat G, Padilla F, Laugier P (2008) Fast wave propagation in trabecular bone: numerical study of the influence of porosity and structural anisotropy. J Acoust Soc Am 123:194–705
Haïat G, Padilla F, Peyrin F, Laugier P (2007) Variation of ultrasonic parameters with microstructure and material properties of trabecular bone: a 3D model simulation. J Bone Miner Res 22:665–674
Haïat G, Wang HL, Brunski JB (2014) Effects of biomechanical properties of the bone-implant interface on dental implant stability: from in silico approaches to the patient’s mouth. Annu Rev Biomed Eng 16:187–213
Hughes TJR (2000) The finite element method: linear static and dynamic finite element analysis. Dover civil and mechanical engineering. Dover Publications, Mineola, New York
Huja SS, Katona TR, Burr DB, Garetto LP, Roberts WE (1999) Microdamage adjacent to endosseous implants. Bone 25:217–222
Laugier P, Haïat G (2010) Bone quantitative ultrasound. Springer, Berlin
Luo GM, Sadegh AM, Alexander H, Jaffe W, Scott D, Cowin SC (1999) The effect of surface roughness on the stress adaptation of trabecular architecture around a cylindrical implant. J Biomech 32:275–284
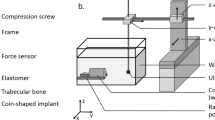
Mathieu V, Anagnostou F, Soffer E, Haiat G (2011a) Numerical simulation of ultrasonic wave propagation for the evaluation of dental implant biomechanical stability. J Acoust Soc Am 129:4062–4072
Mathieu V, Anagnostou F, Soffer E, Haiat G (2011b) Ultrasonic evaluation of dental implant biomechanical stability: an in vitro study. Ultrasound Med Biol 37:262–270
Mathieu V et al (2011c) Micro-Brillouin scattering measurements in mature and newly formed bone tissue surrounding an implant. J Biomech Eng T ASME 133:021006–021006
Mathieu V, Vayron R, Richard G, Lambert G, Naili S, Meningaud JP, Haiat G (2014) Biomechanical determinants of the stability of dental implants: influence of the bone–implant interface properties. J Biomech 47:3–13
Mathieu V, Vayron R, Soffer E, Anagnostou F, Haiat G (2012) Influence of healing time on the ultrasonic response of the bone–implant interface. Ultrasound Med Biol 38:611–618
Meredith N, Alleyne D, Cawley P (1996) Quantitative determination of the stability of the implant–tissue interface using resonance frequency analysis. Clin Oral Implant Res 7:261–267
Meredith N, Friberg B, Sennerby L, Aparicio C (1998) Relationship between contact time measurements and PTV values when using the Periotest to measure implant stability. Int J Prosthodont 11:269–275
Meredith N, Shagaldi F, Alleyne D, Sennerby L, Cawley P (1997) The application of resonance frequency measurements to study the stability of titanium implants during healing in the rabbit tibia. Clin Oral Implant Res 8:234–243
Merheb J, Van Assche N, Coucke W, Jacobs R, Naert I, Quirynen M (2010) Relationship between cortical bone thickness or computerized tomography-derived bone density values and implant stability. Clin Oral Implants Res 21:612–617
Naili S, Vu MB, Grimal Q, Talmant M, Desceliers C, Soize C, Haiat G (2010) Influence of viscoelastic and viscous absorption on ultrasonic wave propagation in cortical bone: application to axial transmission. J Acoust Soc Am 127:2622–2628
Njeh CF, Hans D, Wu C, Kantorovich E, Sister M, Fuerst T, Genant HK (1999) An in vitro investigation of the dependence on sample thickness of the speed of sound along the specimen. Med Eng Phys 21:651–659
Nkenke E, Hahn M, Weinzierl K, Radespiel-Troger M, Neukam FW, Engelke K (2003) Implant stability and histomorphometry: a correlation study in human cadavers using stepped cylinder implants. Clin Oral Implants Res 14:601–609
Pattijn V et al (2007) Resonance frequency analysis of implants in the guinea pig model: influence of boundary conditions and orientation of the transducer. Med Eng Phys 29:182–190
Pattijn V, Van Lierde C, Van der Perre G, Naert I, Sloten JV (2006) The resonance frequencies and mode shapes of dental implants: rigid body behaviour versus bending behaviour—a numerical approach. J Biomech 39:939–947
Rabel A, Kohler SG, Schmidt-Westhausen AM (2007) Clinical study on the primary stability of two dental implant systems with resonance frequency analysis. Clin Oral Invest 11:257–265
Raghavendra S, Wood MC, Taylor TD (2005) Early wound healing around endosseous implants: a review of the literature. Int J Oral Maxillofac Implants 20:425–431
Sansalone V, Bousson V, Naili S, Bergot C, Peyrin F, Laredo JD, Haiat G (2012) Anatomical distribution of the degree of mineralization of bone tissue in human femoral neck: impact on biomechanical properties. Bone 50:876–884
Sansalone V et al (2010) Determination of the heterogeneous anisotropic elastic properties of human femoral bone: from nanoscopic to organ scale. J Biomech 43:1857–1863. doi:10.1016/j.jbiomech.2010.03.034
Sasso M, Haiat G, Talmant M, Laugier P, Naili S (2008a) Singular value decomposition-based wave extraction in axial transmission: application to cortical bone ultrasonic characterization. IEEE Trans Ultrason Ferroelectr Freq Control 55:1328–1332
Sasso M, Haiat G, Yamato Y, Naili S, Matsukawa M (2007) Frequency dependence of ultrasonic attenuation in bovine cortical bone: an in vitro study. Ultrasound Med Biol 33:1933–1942
Sasso M, Haiat G, Yamato Y, Naili S, Matsukawa M (2008b) Dependence of ultrasonic attenuation to bone mass and microstructure in bovine cortical bone. J Biomech 41:347–355
Schulte W et al (1983) Periotest: a new measurement process for periodontal function. Zahnarztl Mitt 73:1229–1230
Seong WJ, Kim UK, Swift JQ, Hodges JS, Ko CC (2009) Correlations between physical properties of jawbone and dental implant initial stability. J Prosthet Dent 101:306–318
Serra G, Morais LS, Elias CN, Meyers MA, Andrade L, Muller C, Muller M (2008) Sequential bone healing of immediately loaded mini-implants. Am J Orthod Dentofacial Orthop 134:44–52
Shalabi MM, Wolke JGC, Cuijpers V, Jansen JA (2007) Evaluation of bone response to titanium-coated polymethyl methacrylate resin (PMMA) implants by X-ray tomography. J Mater Sci Mater Med 18:2033–2039
Souffrant R, Zietz C, Fritsche A, Kluess D, Mittelmeier W, Bader R (2012) Advanced material modelling in numerical simulation of primary acetabular press-fit cup stability. Comput Methods Biomech Biomed Eng 15:787–793
Turkyilmaz I, Aksoy U, McGlumphy EA (2008) Two alternative surgical techniques for enhancing primary implant stability in the posterior Maxilla: a clinical study including bone density, insertion torque, and resonance frequency analysis data. Clin Implant Dent Rel Res 10:231–237
Turkyilmaz I, Tozum TF, Tumer C, Ozbek EN (2006) Assessment of correlation between computerized tomography values of the bone, and maximum torque and resonance frequency values at dental implant placement. J Oral Rehabil 33:881–888
Turkyilmaz I, Tumer C, Ozbek EN, Tozum TF (2007) Relations between the bone density values from computerized tomography, and implant stability parameters: a clinical study of 230 regular platform implants. J Clin Periodontol 34:716–722
Valderrama P, Oates TW, Jones AA, Simpson J, Schoolfield JD, Cochran D (2007) Evaluation of two different resonance frequency devices to detect implant stability: a clinical trial. J Periodont 78:262–272
Van Scotter DE, Wilson CJ (1991) The Periotest method for determining implant success. J Oral Implantol 17:410–413
Vayron R, Barthel E, Mathieu V, Soffer E, Anagnostou F, Haiat G (2011) Variation of biomechanical properties of newly formed bone tissue determined by nanoindentation as a function of healing time. Comput Methods Biomech Biomed Eng 14:139–140
Vayron R, Barthel E, Mathieu V, Soffer E, Anagnostou F, Haiat G (2012) Nanoindentation measurements of biomechanical properties in mature and newly formed bone tissue surrounding an implant. J Biomech Eng 134:021007
Vayron R et al (2013) Variation of the ultrasonic response of a dental implant embedded in tricalcium silicate-based cement under cyclic loading. J Biomech 46:1162–1168
Vayron R, Mathieu V, Michel A, Haïat G (2014a) Assessment of in vitro dental implant primary stability using an ultrasonic method. Ultrasound Med Biol 40(12):2885–2894
Vayron R, Soffer E, Anagnostou F, Haïat G (2014b) Ultrasonic evaluation of dental implant osseointegration. J Biomech47(14):3562–3568
Vayron R, Matsukawa M, Mathieu V, Barthel E, Soffer E, Anagnostou F, Haiat G (2014c) Evolution of bone biomechanical properties at the micrometer scale around titanium implant as a function of healing time. Phys Med Biol 59:1389–1406
Viceconti M, Brusi G, Pancanti A, Cristofolini L (2006) Primary stability of an anatomical cementless hip stem: a statistical analysis. J Biomech 39:1169–1179. doi:10.1016/j.jbiomech.2005.03.024
Viceconti M, Monti L, Muccini R, Bernakiewicz M, Toni A (2001) Even a thin layer of soft tissue may compromise the primary stability of cementless hip stems. Clin Biomech 16:765–775
Wang JY, Tozzi G, Chen J, Contal F, Lupton C, Tong J (2010a) Bone–cement interfacial behaviour under mixed mode loading conditions. J Mech Behav Biomed Mater 3:392–398
Wang ZQ, Zhao ZH, Xue J, Song JL, Deng F, Yang P (2010b) Pullout strength of miniscrews placed in anterior mandibles of adult and adolescent dogs: a microcomputed tomographic analysis. Am J Orthod Dentofac Orthop 137:100–107
Winter W, Mohrle S, Holst S, Karl M (2010) Parameters of implant stability measurements based on resonance frequency and damping capacity: a comparative finite element analysis. Int J Oral Maxillofac Implants 25:532–539
Zhao LX, Xu ZR, Yang Z, Wei X, Tang T, Zhao ZH (2009) Orthodontic mini-implant stability in different healing times before loading: a microscopic computerized tomographic and biomechanical analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 108:196–202
Acknowledgments
This work has been supported by French National Research Agency (ANR) through the PRTS Program (Project OsseoWave ANR-13-PRTS-0015).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vayron, R., Nguyen, VH., Bosc, R. et al. Finite element simulation of ultrasonic wave propagation in a dental implant for biomechanical stability assessment. Biomech Model Mechanobiol 14, 1021–1032 (2015). https://doi.org/10.1007/s10237-015-0651-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10237-015-0651-7