Microvascular Obstruction in ST-Segment Elevation Myocardial Infarction: Looking Back to Move Forward. Focus on CMR
Abstract
:1. Introduction
2. Pathophysiology
2.1. Predominantly Prior to Reperfusion
2.1.1. Patient Factors
2.1.2. Endothelial Abnormalities
2.1.3. Decrease in Capillary Density
2.2. Predominantly at Reperfusion
2.2.1. Ischemia-Reperfusion Injury
2.2.2. Embolization
2.2.3. Vasoconstriction
2.3. Predominantly Post-Reperfusion
2.3.1. Increase in Endothelial Permeability
2.3.2. External Compression
2.3.3. Inflammation
2.4. From the Onset of Ischemia until Late after Reperfusion
Dynamics and Repair
3. Diagnostic Tools
3.1. Widely Available Tools
3.2. In the Catheterization Lab
3.3. Cardiac Imaging Techniques
4. Clinical and Structural Implications
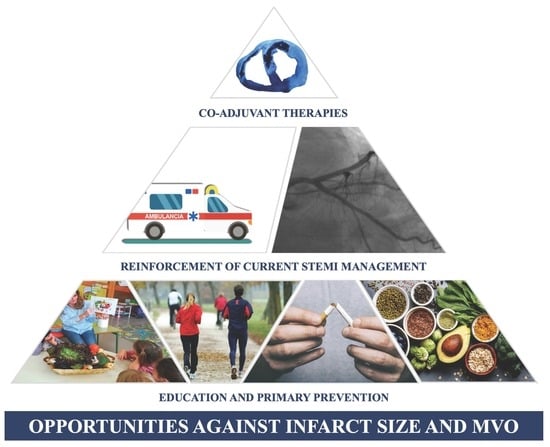
5. Therapeutic Options. Past, Present, and Future
6. Understanding the Dynamics and Repair of MVO for Addressing WH-Questions on Therapy
7. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Herrick, J.B. Clinical features of sudden obstruction of the coronary arteries. JAMA 1912, 59, 2015–2020. [Google Scholar] [CrossRef]
- Menees, D.S.; Peterson, E.D.; Wang, Y.; Curtis, J.P.; Messenger, J.C.; Rumsfeld, J.S.; Gurm, H.S. Door-to-Balloon time and mortality among patients undergoing primary PCI. N. Eng. J. Med. 2013, 369, 901–909. [Google Scholar] [CrossRef] [PubMed]
- Niccoli, G.; Scalone, G.; Lerman, A.; Crea, F. Coronary microvascular obstruction in acute myocardial infarction. Eur. Heart J. 2016, 37, 1024–1033. [Google Scholar] [CrossRef] [PubMed]
- Hamirani, Y.S.; Wong, A.; Kramer, C.M.; Salerno, M. Effect of microvascular obstruction and intramyocardial hemorrhage by CMR on LV remodeling and outcomes after myocardial infarction: A systematic review and meta-analysis. JACC Cardiovasc. Imaging 2014, 7, 940–952. [Google Scholar] [CrossRef] [PubMed]
- Gavara, J.; Rodriguez-Palomares, J.F.; Valente, F.; Monmeneu, J.V.; Lopez-Lereu, M.P.; Bonanad, C.; Ferreira-Gonzalez, I.; Garcia del Blanco, B.; Rodriguez-Garcia, J.; Mutuberria, M.; et al. Prognostic value of strain by tissue tracking cardiac magnetic resonance after ST-segment elevation myocardial infarction. JACC Cardiovasc. Imaging 2018, 11, 1448–1457. [Google Scholar] [CrossRef]
- Kloner, R.A.; Ganote, C.E.; Jennings, R.B. The ‘No-Reflow’ phenomenon after temporary coronary occlusion in the dog. J. Clin. Investig. 1974, 54, 1496–1508. [Google Scholar] [CrossRef]
- Bodi, V.; Monmeneu, J.V.; Ortiz-Perez, J.T.; Lopez-Lereu, M.P.; Bonanad, C.; Husser, O.; Miñana, G.; Gomez, C.; Nuñez, J.; Forteza, M.J.; et al. Prediction of reverse remodeling at cardiac MR imaging soon after first ST-segment-elevation myocardial infarction: Results of a large prospective registry. Radiology 2016, 278, 54–63. [Google Scholar] [CrossRef]
- de Waha, S.; Patel, M.R.; Granger, C.B.; Ohman, E.M.; Maehara, A.; Eitel, I.; Ben-Yehuda, O.; Jenkins, P.; Thiele, H.; Stone, G.W. Relationship between microvascular obstruction and adverse events following primary percutaneous coronary intervention for ST-segment elevation myocardial infarction: An individual patient data pooled analysis from seven randomized trials. Eur. Heart J. 2017, 38, 3502–3510. [Google Scholar] [CrossRef]
- Hollander, M.R.; de Waard, G.A.; Konijnenberg, L.S.; Meijer-van Putten, R.M.; van den Brom, C.E.; Paauw, N.; de Vries, H.E.; Aman, J.; van Nieuw Amerongen, G.P.; Hordijk, P.L.; et al. Dissecting the effects of ischemia and reperfusion on the coronary microcirculation in a rat model of acute myocardial infarction. PLoS ONE 2016, 11, e0157233. [Google Scholar]
- Rios-Navarro, C.; Hueso, L.; Miñana, G.; Nuñez, J.; Ruiz-Sauri, A.; Sanz, M.J.; Canoves, J.; Chorro, F.J.; Piqueras, L.; Bodi, V. Coronary serum obtained after myocardial infarction induces angiogenesis and microvascular obstruction repair. Role of hypoxia-inducible factor-1A. Rev. Esp. Cardiol. 2018, 71, 440–449. [Google Scholar] [CrossRef]
- Davidson, S.M.; Ferdinandy, P.; Andreadou, I.; Botker, H.E.; Heusch, G.; Ibañez, B.; Ovize, M.; Schulz, R.; Yellon, D.M.; Hausenloy, D.J.; et al. Multitarget strategies to reduce myocardial ischemia/reperfusion injury. J. Am. Coll. Cardiol. 2019, 73, 89–99. [Google Scholar] [CrossRef] [PubMed]
- Porto, I.; Biasucci, L.M.; de Maria, G.L.; Leone, A.M.; Niccoli, G.; Burzotta, F.; Trani, C.; Tritarelli, A.; Vergallo, R.; Liuzzo, G.; et al. Intracoronary microparticles and microvascular obstruction in patients with ST elevation myocardial infarction undergoing primary percutaneous intervention. Eur. Heart J. 2012, 33, 2928–2938. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bekkers, S.; Yazdani, S.K.; Virmani, R.; Waltenberger, J. Microvascular obstruction: Underlying pathophysiology and clinical diagnosis. J. Am. Coll. Cardiol. 2010, 55, 1649–1660. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Jiménez, R.; Garcia-Prieto, J.; Sanchez-Gonzalez, J.; Agueo, J.; Lopez-Martin, G.J.; Galan-Arriola, C.; Molina-Iracheta, A.; Doohan, R.; Fuster, V.; Ibañez, B. Pathophysiology underlying the bimodal edema phenomenon after myocardial ischemia/reperfusion. J. Am. Coll. Cardiol. 2015, 66, 816–828. [Google Scholar] [CrossRef] [PubMed]
- Husser, O.; Bodi, V.; Sanchis, J.; Nuñez, J.; Mainar, L.; Chorro, F.J.; Lopez-Lereu, M.P.; Monmeneu, J.V.; Chauster, F.; Forteza, M.J.; et al. White blood cell subtypes after STEMI: Temporal evolution, association with cardiac magnetic resonance—derived infarct size and impact on outcome. Inflammation 2011, 34, 73–84. [Google Scholar] [CrossRef]
- Rios-Navarro, C.; Gavara, J.; Vidal, V.; Bonanad, C.; Racugno, P.; Bayes-Genis, A.; Miñana, G.; Husser, O.; Oltra, R.; Nuñez, J.; et al. Characterization and implications of the dynamics of eosinophils in blood and in the infarcted myocardium after coronary reperfusion. PLoS ONE 2018, 13, e0206344. [Google Scholar] [CrossRef]
- Ge, L.; Zhou, X.; Ji, W.J.; Lu, R.Y.; Zhang, Y.; Zhang, Y.D.; Ma, Y.Q.; Zhao, J.H.; Li, Y.M. Neutrophil extracellular traps in ischemia-reperfusion injury-induced myocardial no-reflow: Therapeutic potential of DNase-based reperfusion strategy. Am. J. Physiol. Heart Circ. Physiol. 2015, 308, H500–H509. [Google Scholar] [CrossRef]
- Husser, O.; Bodi, V.; Sanchis, J.; Nuñez, J.; Lopez-Lereu, M.P.; Monmeneu, J.V.; Gomez, C.; Rumiz, E.; Merlos, P.; Bonanad, C.; et al. Predictors of cardiovascular magnetic resonance-derived microvascular obstruction on patients admission in STEMI. Int. J. Cardiol. 2013, 166, 77–84. [Google Scholar] [CrossRef]
- Husser, O.; Bodí, V.; Sanchis, J.; Nuñez, J.; Mainar, L.; Rumiz, E.; Lopez-Lereu, M.P.; Monmeneu, J.; Chaustre, F.; Trapero, I.; et al. The sum of ST-segment elevation is the best predictor of microvascular obstruction in patients treated successfully by primary percutaneous coronary intervention. Cardiovascular magnetic resonance study. Rev. Esp. Cardiol. 2010, 63, 1145–1154. [Google Scholar] [CrossRef]
- Younger, J.F.; Plein, S.; Barth, J.; Ridgway, J.P.; Ball, S.G.; Greenwood, J.P. Troponin-I concentration 72h after myocardial infarction correlates with infarct size and presence of microvascular obstruction. Heart 2007, 93, 1547–1551. [Google Scholar] [CrossRef]
- Reichek, N. Meta-analysis of MACE in MI. What’s the MO? JACC Cardiovasc. Imaging 2014, 7, 953–955. [Google Scholar] [CrossRef]
- Niccoli, G.; Montone, R.A.; Ibanez, B.; Thiele, H.; Crea, F.; Heusch, G.; Bulluck, H.; Hausenloy, D.J.; Berry, C.; Stierman, T.; et al. Optimized treatment of ST-elevation myocardial infarction. The unmet need to target coronary microvascular obstruction as primary treatment goal to further improve prognosis. Circ. Res. 2019, 125, 245–258. [Google Scholar] [CrossRef]
- Eitel, I.; de Waha, S.; Wöhrle, J.; Fuernau, G.; Lurz, P.; Pauschinger, M.; Desch, S.; Schuler, G.; Thiele, H. Comprehensive prognosis assessment by CMR imaging after ST-segment elevation myocardial infarction. J. Am. Coll. Cardiol. 2014, 64, 1217–1226. [Google Scholar] [CrossRef]
- Bodi, V.; Sanchis, J.; Nuñez, J.; Mainar, L.; Lopez-Lereu, M.P.; Monmeneu, J.; Rumiz, E.; Chaustre, F.; Trapero, I.; Husser, O.; et al. Prognostic value of a comprehensive cardiac magnetic resonance assessment soon after a first ST-segment elevation myocardial infarction. JACC Cardiovasc. Imaging 2009, 2, 835–842. [Google Scholar] [CrossRef]
- Bodi, V.; Sanchis, J.; Mainar, L.; Chorro, F.J.; Nuñez, J.; Monmeneu, J.V.; Chaustre, F.; Forteza, M.J.; Ruiz-Sauri, A.; Lopez-Lereu, M.P.; et al. Right ventricular involvement in anterior myocardial infarction: A translational approach. Cardiovasc. Res. 2010, 87, 601–608. [Google Scholar] [CrossRef]
- Tarantini, G.; Favaretto, E.; Marra, M.P.; Frigo, A.C.; Napodano, M.; Cacciavillani, L.; Goivagnoni, A.; Renda, P.; de Biasio, V.; Plebani, M.; et al. Postconditioning during coronary angioplasty in acute myocardial infarction: The POST-AMI trial. Int. J. Cardiol. 2012, 162, 33–38. [Google Scholar] [CrossRef]
- Bodi, V.; Ruiz-Nodar, J.M.; Feliu, E.; Miñana, G.; Nuñez, J.; Husser, O.; Martinez-Elvira, J.; Ruiz, A.; Bonanad, C.; Monmeneu, J.V.; et al. Effect of ischemic postconditioning on microvascular obstruction in reperfused myocardial infarction. Results of a randomized study in patients and of an experimental model in swine. Int. J. Cardiol. 2014, 175, 138–146. [Google Scholar] [CrossRef]
- Mewton, N.; Thibault, H.; Roubille, F.; Lairez, O.; Rioufol, G.; Sportouch, C.; Sanchez, I.; Bergerot, C.; Cung, T.T.; Finet, G.; et al. Postconditioning attenuates no-reflow in STEMI patients. Basic Res. Cardiol. 2013, 108, 383. [Google Scholar] [CrossRef]
- Sörensson, P.; Ryden, L.; Saleh, N.; Tornvall, P.; Arheden, H.; Pernow, J. Long-term impact of postconditioning on infarct size and left ventricular ejection fraction in patients with ST-elevation myocardial infarction. BMC Cardiovasc. Disord. 2013, 13, 22. [Google Scholar] [CrossRef]
- Freixa, X.; Ballera, N.; Ortiz-Perez, J.T.; Jimenez, M.; Pare, C.; Bosch, X.; de Caralt, T.M.; Betriu, A.; Masotti, M. Ischaemic postconditioning revisited: Lack of effects on infarct size following primary percutaneous coronary intervention. Eur. Heart. J. 2012, 33, 103–112. [Google Scholar] [CrossRef]
- Dwyer, N.B.; Mikami, Y.; Hilland, D.; Aljzeeri, A.; Friedrich, M.G.; Traboulsi, M.; Anderson, T.J. No cardioprotective benefit of ischemic postconditioning in patients with ST-segment elevation myocardial infarction. J. Interv. Cardiol. 2013, 26, 482–490. [Google Scholar] [CrossRef] [PubMed]
- Eitel, I.; Stiermaier, T.; Rommei, K.P.; Fuernau, G.; Sandri, M.; Marigner, N.; Linke, A.; Erbs, S.; Lurz, P.; Boudriot, E.; et al. Cardioprotection by combined intrahospital remote ischaemic preconditioning and postconditioning in ST-elevation myocardial infarction: The randomized LIPSIA CONDITIONING trial. Eur. Heart J. 2015, 36, 3049–3057. [Google Scholar] [CrossRef] [PubMed]
- Crimi, G.; Pica, S.; Raineri, C.; Bramucci, E.; de Ferrari, G.M.; Klersy, C.; Ferlini, M.; Marinoni, B.; Repetto, A.; Romeo, M.; et al. Remote ischemic post-conditioning of the lower limb during primary percutaneous coronary intervention safely reduces enzymatic infarct size in anterior myocardial infarction: A randomized controlled trial. J. Am. Coll. Cardiol. Interv. 2013, 6, 1055–1063. [Google Scholar] [CrossRef] [PubMed]
- White, S.K.; Frohlich, G.M.; Sado, D.M.; Maestrini, V.; Fontana, M.; Treibel, T.A.; Tehrani, S.; Flett, A.S.; Meier, P.; Ariti, C.; et al. Remote ischemic conditioning reduces myocardial infarct size and edema in patients with ST-segment elevation myocardial infarction. J. Am. Coll. Cardiol. Interv. 2015, 8, 178–188. [Google Scholar] [CrossRef]
- Gotberg, M.; Olivecrona, G.K.; Koul, S.; Carlsson, M.; Engblom, H.; Ugander, M.; van der Pals, J.; Algotsson, L.; Arheden, H.; Erlinge, D. A pilot study of rapid cooling by cold saline and endovascular cooling before reperfusion in patients with ST-elevation myocardial infarction. Circ. Cardiovasc. Interv. 2010, 3, 400–407. [Google Scholar] [CrossRef]
- Keeble, T.R.; Karamasi, G.V.; Noc, M.; Sredniawa, B.; Aradi, D.; Neskovic, A.N.; Arheden, H.; Erlinge, D.; Holzer, M. Effect of intravascular cooling on microvascular obstruction in conscious patients with ST-elevation myocardial infarction undergoing primary PCI: Results from the COOL AMI EU pilot study. Cardiovasc. Revasc. Med. 2019, 20, 799–804. [Google Scholar] [CrossRef]
- Erlinge, D.; Gotberg, M.; Lang, I.; Holzer, M.; Noc, M.; Clemmensen, P.; Jensen, U.; Metzler, B.; James, S.; Botker, H.E.; et al. Rapid endovascular catheter core cooling combined with cold saline as an adjunct to percutaneous coronary intervention for the treatment of acute myocardial infarction. The CHILL-MI Trial: A randomized controlled study of the use of central venous catheter core cooling combined with cold saline as an adjunct to percutaneous coronary intervention for the treatment of acute myocardial infarction. J. Am. Coll. Cardiol. 2014, 63, 1857–1865. [Google Scholar]
- Testori, C.; Beitzke, D.; Mangold, A.; Sterz, F.; Loewe, C.; Weiser, C.; Scherz, T.; Herkner, H.; Lang, I. Out-of-hospital initiation of hypothermia in ST-segment elevation myocardial infarction: A randomised trial. Heart 2019, 105, 531–537. [Google Scholar] [CrossRef]
- Sardella, G.; Mancone, M.; Bucciarelli-Ducci, C.; Agati, L.; Scardala, R.; Carbone, I.; Francone, M.; Di Roma, A.; Benedetti, G.; Conti, G.; et al. Thrombus aspiration during primary percutaneous coronary intervention improves myocardial reperfusion and reduces infarct size: The EXPIRA (thrombectomy with export catheter in infarct-related artery during primary percutaneous coronary intervention) prospective, randomized trial. J. Am. Coll. Cardiol. 2009, 53, 309–315. [Google Scholar]
- De Carlo, M.; Aquaro, G.D.; Palmieri, C.; Guerra, E.; Misuraca, L.; Giannini, C.; Lombardi, M.; Berti, S.; Petronio, A.S. A prospective randomized trial of thrombectomy versus no thrombectomy in patients with ST-segment elevation myocardial infarction and thrombus-rich lesions: MUSTELA (MUltidevice Thrombectomy in Acute ST-Segment ELevation Acute Myocardial Infarction) trial. J. Am. Coll. Cardiol. Interv. 2012, 5, 1223–1230. [Google Scholar] [CrossRef]
- Hoole, S.P.; Jaworski, C.; Brown, A.J.; McCornick, L.M.; Agrawal, B.; Clarke, S.C.; West, N.E. Serial assessment of the index of microcirculatory resistance during primary percutaneous coronary intervention comparing manual aspiration catheter thrombectomy with balloon angioplasty (IMPACT study): A randomised controlled pilot study. Open Heart 2015, 2, e000238. [Google Scholar] [CrossRef]
- Ahn, S.G.; Lee, S.H.; Lee, J.H.; Lee, J.W.; Youn, Y.J.; Ahn, M.S.; Kim, J.Y.; Yoo, B.S.; Yoon, J.; Choe, K.H.; et al. Efficacy of combination treatment with intracoronary abciximab and aspiration thrombectomy on myocardial perfusion in patients with ST-segment elevation myocardial infarction undergoing primary coronary stenting. Yonsei Med. J. 2014, 55, 606–616. [Google Scholar] [CrossRef]
- Carrabba, N.; Parodi, G.; Maehara, A.; Pradella, S.; Migliorini, A.; Valenti, R.; Comito, V.; Marrani, M.; Rega, L.; Colagrande, S.; et al. Rheolityc thrombectomy in acute myocardial infarction: Effect on microvascular obstruction, infarct size, and left ventricular remodeling. Catheter. Cardiovasc. Interv. 2016, 87, E1–E8. [Google Scholar] [CrossRef]
- Van Geus, R.J.; Sideris, G.; van Royen, N.; El Mahmoud, R.; Diletti, R.; Bal Dit Sollier, C.; Garot, J.; Van Der Hoeven, N.W.; Cortese, B.; Ding, L.; et al. Bivalirudin infusion to reduce ventricular infarction: The open-label, randomised Bivalirudin Infusion for Ventricular InfArction Limitation (BIVAL) study. Eurointervention 2017, 13, e540–e548. [Google Scholar] [CrossRef]
- Wohrle, J.; Merkle, N.; Kunze, M.; Cristea, E.; Mehran, R.; Rottbauer, W.; Stone, G.W. Effect of bivalirudin compared with unfractionated heparin plus abciximab on infarct size and myocardial recovery after primary percutaneous coronary intervention: The horizons-AMI CMRI substudy. Catheter. Cardiovasc. Interv. 2012, 79, 1083–1089. [Google Scholar] [CrossRef]
- McCartney, P.J.; Eteiba, H.; Maznyczka, A.M.; McEntegart, M.; Greenwood, J.P.; Muir, D.F.; Chowshary, S.; Gershlick, A.H.; Appleby, C.; Cotton, J.M.; et al. Effect of low-dose intracoronary alteplase during primary percutaneous coronary intervention on microvascular obstruction in patients with acute myocardial infarction: A randomized clinical trial. JAMA 2019, 321, 56–68. [Google Scholar] [CrossRef]
- Suh, J.W.; Chung, W.Y.; Kim, Y.S.; Kim, K.I.; Jeon, E.J.; Cho, Y.S.; Youn, T.J.; Chae, I.H.; Kim, C.H.; Choi, D.J. The effect of intravenous administration of erythropoietin on the infarct size in primary percutaneous coronary intervention. Int. J. Cardiol. 2011, 149, 216–220. [Google Scholar] [CrossRef]
- Ludman, A.J.; Yellon, D.M.; Hasleton, J.; Ariti, C.; Babu, G.G.; Boston-Griffiths, E.; Venugopal, V.; Walker, M.; Holdright, D.; Swanton, H.; et al. Effect of erythropoietin as an adjunct to primary percutaneous coronary intervention: A randomised controlled clinical trial. Heart 2011, 97, 1560–1565. [Google Scholar] [CrossRef]
- Prunier, F.; Biere, L.; Gilard, M.; Boschat, J.; Mouquet, F.; Bauchart, J.J.; Charbonnier, B.; Genee, O.; Guerin, P.; Warin-Fresse, K.; et al. Single high-dose erythropoietin administration immediately after reperfusion in patients with ST-segment elevation myocardial infarction: Results of the erythropoietin in myocardial infarction trial. Am. Heart J. 2012, 163, 200–207. [Google Scholar] [CrossRef]
- Song, Y.B.; Hahn, J.Y.; Gwon, H.C.; Chang, S.A.; Lee, S.C.; Choe, Y.H.; Choi, S.H.; Choi, J.H.; Lee, S.H.; Oh, J.K. A high loading dose of clopidogrel reduces myocardial infarct size in patients undergoing primary percutaneous coronary intervention: A magnetic resonance imaging study. Am. Heart J. 2012, 163, 500–507. [Google Scholar] [CrossRef]
- Tarantini, G.; Ramondo, A.; Corbetti, F.; Marra, M.P.; Cacciavillani, L.; Napodano, M.; Bilato, C.; Razzolini, R.; Iliceto, S. Periprocedural abciximab administration in ST elevation myocardial infarction patients. Effect on severe microvascular obstruction beyond the restoration of epicardial coronary flow by primary angioplasty. Cardiology 2008, 110, 129–134. [Google Scholar] [CrossRef]
- Maehara, A.; Mintz, G.; Brener, S.; Dambrink, J.H.; El-Omar, M.; Gershlick, A.; Fahy, M.; Mehran, R.; Gibson, C.M.; Stone, G. Effect of intracoronary abciximab and aspiration thrombectomy on microvascular obstruction in large anterior myocardial infarction: The INFUSE-AMI MRI Substudy. J. Am. Coll. Cardiol. 2012, 60, B19. [Google Scholar] [CrossRef]
- Thiele, H.; Schindler, K.; Friedenberger, J.; Eitel, I.; Furnau, G.; Grebe, E.; Erbs, S.; Linke, A.; Mobius-Winkler, S.; Kivelitz, D.; et al. Intracoronary compared with intravenous bolus abciximab application in patients with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention. The randomized Leipzig immediate percutaneous coronary intervention abciximab IV versus IC in ST-elevation myocardial infarction trial. Circulation 2008, 118, 49–57. [Google Scholar]
- Patel, M.R.; Worthley, S.G.; Stebbins, A.; Dill, T.; Rademakers, F.E.; Valeti, U.S.; Barsness, G.W.; Van de Werf, F.; Hamm, C.W.; Armstrong, P.W. Pexelizumab and infarct size in patients with acute myocardial infarction undergoing primary percutaneous coronary intervention: A delayed enhancement cardiac magnetic resonance substudy from the APEX-AMI trial. JACC Cardiovasc. Imaging 2010, 3, 52–60. [Google Scholar] [CrossRef]
- Vanini, L.; Muro, A.; Sanchis, J.; Ortiz-Perez, J.T.; Flores-Umanzor, E.; Lopez-Lereu, M.P.; Badimon, L.; Sabate, M.; Brugaletta, S. Can new generation P2Y12 inhibitors play a role in microvascular obstruction in STEMI? Int. J. Cardiol. 2016, 223, 226–227. [Google Scholar] [CrossRef]
- Khan, J.N.; Greenwood, J.P.; Nazir, S.A.; Lai, F.Y.; Dalby, M.; Curzen, N.; Hetherington, S.; Kelly, D.J.; Blackman, D.; Peebles, C.; et al. Infarct size following treatment with second- versus third-generation P2Y12 antagonists in patients with multivessel coronary disease at ST-segment elevation myocardial infarction in the CvLPRIT study. J. Am. Heart Assoc. 2016, 5, e003403. [Google Scholar] [CrossRef]
- Nazir, S.A.; McCann, G.P.; Greenwood, J.P.; Kunadian, V.; Khan, J.N.; Mahmoud, I.Z.; Blackman, D.J.; Been, M.; Abrams, K.R.; Shipley, L.; et al. Strategies to attenuate micro-vascular obstruction during P-PCI: The randomized reperfusion facilitated by local adjunctive therapy in ST-elevation myocardial infarction trial. Eur. Heart J. 2016, 37, 1910–1919. [Google Scholar] [CrossRef]
- Garcia-Dorado, D.; Garcia-del-Blanco, B.; Otaegui, J.; Rodriguez-Palomares, J.; Pineda, V.; Gimeno, F.; Ruiz-Salmeron, R.; Elizaga, J.; Evangelista, A.; Fernandez-Aviles, F.; et al. Intracoronary injection of adenosine before reperfusion in patients with ST-segment elevation myocardial infarction: A randomized controlled clinical trial. Int. J. Cardiol. 2014, 177, 935–941. [Google Scholar] [CrossRef]
- Desmet, W.; Bogaert, J.; Dubois, C.; Sinnaeve, P.; Adriaenssens, T.; Pappas, C.; Ganame, J.; Dymarkowski, S.; Janssens, S.; Belmans, A.; et al. High-dose intracoronary adenosine for myocardial salvage in patients with acute ST-segment elevation myocardial infarction. Eur. Heart J. 2011, 32, 867–877. [Google Scholar] [CrossRef]
- Yamada, K.; Isobe, S.; Ishii, H.; Yokouchi, K.; Iwata, H.; Sawada, K.; Murohara, T. Impacts of nicorandil on infarct myocardium in comparison with nitrate: Assessed by cardiac magnetic resonance imaging. Heart Vessels 2016, 31, 1430–1437. [Google Scholar] [CrossRef]
- Kim, E.K.; Hahn, J.Y.; Song, Y.B.; Chang, S.A.; Choi, J.H.; Choi, S.H.; Lee, S.C.; Choe, Y.H.; Lee, S.H.; Gwon, H.C. Effects of high-dose atorvastatin pretreatment in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention: A cardiac magnetic resonance study. J. Korean Med. Sci. 2015, 30, 435–441. [Google Scholar] [CrossRef]
- Marenzi, G.; Cosentino, N.; Cortinovis, S.; Milazzo, V.; Rubino, M.; Cabiati, A.; De Metrio, M.; Moltrasio, M.; Lauri, G.; Campodonico, J.; et al. Myocardial infarct size in patients on long-term statin therapy undergoing primary percutaneous coronary intervention for ST-elevation myocardial infarction. Am. J. Cardiol. 2015, 116, 1791–1797. [Google Scholar] [CrossRef]
- García-Prieto, J.; Villena-Gutiérrez, R.; Gómez, M.; Bernardo, E.; Pun-Garcia, A.; Garcia-Lunar, I.; Crainiciuc, G.; Fernandez-Jimenez, R.; Sreeramkumar, V.; Bourio-Martinez, R.; et al. Neutrophil stunning by metoprolol reduces infarct size. Nat. Commun. 2017, 8, 14780. [Google Scholar] [CrossRef]
- Atar, D.; Petzelbauer, P.; Schwitter, J.; Huber, K.; Rensing, B.; Kasprzak, J.D.; Butter, C.; Grip, L.; Hansen, P.R.; Suselbeck, T.; et al. Effect of intravenous FX06 as an adjunct to primary percutaneous coronary intervention for acute ST-segment elevation myocardial infarction: Results of the F.I.R.E. (Efficacy of FX06 in the Prevention of Myocardial Reperfusion Injury) trial. J. Am. Coll. Cardiol. 2009, 53, 720–729. [Google Scholar] [CrossRef]
- Janssens, S.; Dubois, C.; Bogaert, J.; Theunissen, K.; Deroose, C.; Desmet, W.; Kalantzi, M.; Herbots, L.; Sinnaeve, P.; Dens, J.; et al. Autologous bone marrow-derived stem-cell transfer in patients with ST-segment elevation myocardial infarction: Double-blind, randomised controlled trial. Lancet 2006, 367, 113–121. [Google Scholar] [CrossRef]
- Dill, T.; Schachinger, V.; Rolf, A.; Mollmann, S.; Thiele, H.; Tillmanns, H.; Assmus, B.; Dimmeler, S.; Zeiher, A.M.; Hamm, C. Intracoronary administration of bone marrow-derived progenitor cells improves left ventricular function in patients at risk for adverse remodeling after acute ST-segment elevation myocardial infarction: Results of the Reinfusion of Enriched Progenitor cells And Infarct Remodeling in Acute Myocardial Infarction study (REPAIR-AMI) cardiac magnetic resonance imaging substudy. Am. Heart J. 2009, 157, 541–547. [Google Scholar]
- Roncalli, J.; Mouquet, F.; Piot, C.; Trochu, J.N.; Le Corvoisier, P.; Neuder, Y.; Le Tourneau, T.; Agostini, D.; Gaxotte, V.; Sportouch, C.; et al. Intracoronary autologous mononucleated bone marrow cell infusion for acute myocardial infarction: Results of the randomized multicenter BONAMI trial. Eur. Heart J. 2011, 32, 1748–1757. [Google Scholar] [CrossRef]
- Hirsch, A.; Nijveldt, R.; van der Vleuten, P.A.; Tijssen, J.G.; van der Glessen, W.J.; Tio, R.A.; Waltenberger, J.; ten Berg, J.M.; Doevendans, P.A.; Aengevaeren, W.E.; et al. Intracoronary infusion of mononuclear cells from bone marrow or peripheral blood compared with standard therapy in patients after acute myocardial infarction treated by primary percutaneous coronary intervention: Results of the randomized controlled HEBE trial. Eur. Heart J. 2011, 32, 1736–1747. [Google Scholar]
- Surder, D.; Manka, R.; Lo Cicero, V.L.; Moccetti, T.; Rufiback, K.; Soncin, S.; Turchetto, L.; Radrizzani, M.; Astori, G.; Schwitter, J.; et al. Intracoronary injection of bone marrow-derived mononuclear cells early or late after acute myocardial infarction: Effects on global left ventricular function. Circulation 2013, 127, 1968–1979. [Google Scholar] [CrossRef]
- San Roman, J.A.; Sanchez, P.L.; Villa, A.; Sanz-Ruiz, R.; Fernandez-Santos, M.E.; Gimeno, F.; Ramos, B.; Arnold, R.; Serrador, A.; Gutierrez, H. Comparison of different bone marrow-derived stem cell approaches in reperfused STEMI: A multicenter, prospective, randomized, open-labeled TECAM trial. J. Am. Coll. Cardiol. 2015, 65, 2372–2382. [Google Scholar] [CrossRef]
- Wohrle, J.; von Scheidt, F.; Schauwecker, P.; Weisneth, M.; Markovic, S.; Schrezenmeier, H.; Hombach, V.; Rottbauer, W.; Bernhardt, P. Impact of cell number and microvascular obstruction in patients with bone-marrow derived cell therapy: Final results from the randomized, double-blind, placebo controlled intracoronary Stem Cell therapy in patients with Acute Myocardial Infarction (SCAMI) trial. Clin. Res. Cardiol. 2013, 102, 765–770. [Google Scholar] [PubMed]
- Heusch, G. Cardioprotection research must leave its comfort zone. Eur. Heart J. 2018, 39, 3393–3395. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rezkalla, S.H.; Stankowski, R.V.; Janna, J.; Kloner, R.A. Management of no-reflow phenomenon in the catheterization laboratory. J. Am. Coll. Cardiol. Interv. 2017, 10, 215–223. [Google Scholar] [CrossRef]
- Barton, P.; Andronis, L.; Briggs, A.; McPherson, K.; Capewell, S. Effectiveness and cost effectiveness of cardiovascular disease prevention in whole populations: Modelling study. BMJ 2011, 343, d4044. [Google Scholar] [CrossRef]
- Bodi, V.; Sanchis, J.; Morales, J.M.; Marrachelli, V.G.; Nuñez, J.; Forteza, M.J.; Chaustre, F.; Gomez, C.; Mainar, L.; Miñana, G.; et al. Metabolomic profile of human myocardial ischemia by nuclear magnetic resonance spectroscopy of peripheral blood serum: A translational study based on transient coronary occlusion models. J. Am. Coll. Cardiol. 2012, 59, 1629–1641. [Google Scholar] [CrossRef]
- Zalewski, J.; Claus, P.; Bogaert, J.; Driessche, N.V.; Driesen, R.B.; Galan, D.T.; Sipido, K.R.; Buszman, P.; Milewski, K.; van de Werf, F. Cyclosporine A reduces microvascular obstruction and preserves left ventricular function deterioration following myocardial ischemia and reperfusion. Basic Res. Cardiol. 2015, 110, 18. [Google Scholar] [CrossRef]
- Cung, T.T.; Morel, O.; Cayla, G.; Rioufol, G.; Garcia-Dorado, D.; Angoulvant, D.; Bonnefoy-Cudraz, E.; Guerin, P.; Elbaz, M.; Delarche, N.; et al. Cyclosporine before PCI in Patients with Acute Myocardial Infarction. N. Eng. J. Med. 2015, 373, 1021–1031. [Google Scholar] [CrossRef]
- Rahman, F.A.; Abdullah, S.S.; Manan, W.Z.W.A.; Tan, L.T.; Neoh, C.; Ming, L.C.; Chan, K.; Kee, L.; Goh, B.; Salmasi, S.; et al. Efficacy and safety of cyclosporine A in acute myocardial infarction: A systemic review and meta-analysis. Front. Pharmacol. 2018, 9, 238. [Google Scholar] [CrossRef]
- Bodi, V.; Sanchis, J.; Lopez-Lereu, M.P.; Nunez, J.; Mainar, L.; Pellicer, M.; Sanz, R.; Gomez, C.; Bosch, M.J.; Husser, O.; et al. Evolution of 5 cardiovascular magnetic resonance-derived viability indexes after reperfused myocardial infarction. Am. Heart J. 2007, 153, 649–655. [Google Scholar] [CrossRef]
- Niccoli, G.; Burzotta, F.; Galiuto, L.; Crea, F. Myocardial no-reflow in humans. J. Am. Coll. Cardiol. 2009, 54, 281–292. [Google Scholar] [CrossRef]
- Hervas, A.; de Dios, E.; Forteza, M.J.; Miñana, G.; Nuñez, J.; Ruiz-Sauri, A.; Bonanad, C.; Perez-Sole, N.; Chorro, F.J.; Bodi, V. Intracoronary infusion of thioflavin-S to study microvascular obstruction in a model of myocardial infarction. Rev. Esp. Cardiol. 2015, 68, 928–934. [Google Scholar] [CrossRef] [PubMed]
- Ferraro, B.; Leoni, G.; Hinkel, R.; Ormanns, S.; Paulin, N.; Ortega-Gomez, A.; Viola, J.R.; de Jong, R.; Bongiovanni, D.; Bozoglu, T.; et al. Pro-angiogenic macrophage phenotype to promote myocardial repair. J. Am. Coll. Cardiol. 2019, 73, 2990–3002. [Google Scholar] [CrossRef] [PubMed]
- Hueso, L.; Rios-Navarro, C.; Ruiz-Sauri, A.; Chorro, F.J.; Nuñez, J.; Sanz, M.J.; Bodi, V.; Piqueras, L. Dynamics and implications of circulating anti-angiogenic VEGF-A165b isoform in patients with ST-segment elevation myocardial infarction. Sci. Rep. 2017, 7, 9962. [Google Scholar] [CrossRef] [PubMed]







| Design | n | CMR-Derived MVO | Major Events | First Author | |
|---|---|---|---|---|---|
| [Reference] | |||||
| 1. Patient factors * | |||||
| 2. Endothelial abnormalities † | |||||
| 3. Decrease in capillary density † | |||||
| 4. Ischemia-reperfusion injury | |||||
| Post-conditioning | R, OL, PC | 78 | 0 | 0 | Tarantini [26] |
| R, OL, PC | 101 | 0 | Bodi [27] | ||
| R, OL, PC | 50 | + | Mewton [28] | ||
| R, OL, PC | 68 | 0 | Sörensson [29] | ||
| R, OL, PC | 79 | 0 | 0 | Freixa [30] | |
| R, OL, PC | 102 | 0 | Dwyer [31] | ||
| R, OL, PC | 464 | 0 | 0 | Eitel [32] | |
| Remote ischemic conditioning | R, OL, PC | 464 | 0 | 0 | Eitel [32] |
| R, OL, PC | 77 | 0 | 0 | Crimi [33] | |
| R, OL, PC | 83 | 0 | White [34] | ||
| Hypothermia | R, OL, PC | 18 | 0 | Gotberg [35] | |
| R, OL, PC | 50 | 0 | 0 | Keeble [36] | |
| R, OL, PC | 120 | 0 | 0 | Erlinge [37] | |
| R, OL, PC | 101 | 0 | Testori [38] | ||
| 5. Embolization | |||||
| Thrombus aspiration | R, OL, PC | 175 | + | + | Sardella [39] |
| R, SB, PC | 154 | + | 0 | De Carlo [40] | |
| R, OL, PC | 40 | 0 | 0 | Hoole [41] | |
| R, SB, PC | 30 | + | 0 | Ahn [42] | |
| R, SB, PC | 37 | 0 | Carrabba [43] | ||
| Bivalirudin | R, OL, PC | 78 | 0 | van Geus [44] | |
| R, OL, PC | 51 | 0 | Wohrle [45] | ||
| Alteplase | R, DB, PC | 440 | 0 | 0 | McCartney [46] |
| Erythropoietin | R, OL, PC | 50 | 0 | 0 | Suh [47] |
| R, DB, PC | 41 | 0 | 0 | Ludman [48] | |
| R, OL, PC | 102 | + | 0 | Prunier [49] | |
| Clopidogrel | R, OL, PC | 198 | + | 0 | Song [50] |
| Abciximab | R, DB, PC | 85 | 0 | Tarantini [51] | |
| R, SB, PC | 169 | 0 | Maehara [52] | ||
| R, SB, Non-PC | 138 | + | Thiele [53] | ||
| Pexelizumab | R, DB, PC | 99 | 0 | Patel [54] | |
| Ticagrelor/ | Observational | 108 | 0 | Vanini [55] | |
| Prasugrel | R, OL, PC | 203 | 0 | 0 | Khan [56] |
| 6. Vasoconstriction | |||||
| Adenosine | R, OL, PC | 247 | 0 | 0 | Nazir [57] |
| R, DB, PC | 201 | 0 | Garcia-Dorado [58] | ||
| R, SB, PC | 110 | 0 | Desmet [59] | ||
| Nitroprusside | R, OL, PC | 247 | 0 | 0 | Nazir [57] |
| Nicorandil | R, OL, PC | 52 | + | Yamada [60] | |
| 7. Increase in endothelial permeability † | |||||
| 8. External compression † | |||||
| 9. Inflammation | |||||
| Atorvastatin | R, OL, PC | 37 | 0 | 0 | Kim [61] |
| Non-R, OL, PC | 230 | 0 | Marenzi [62] | ||
| Metoprolol | R, SB, PC | 220 | + | Garcia-Prieto [63] | |
| FX06 | R, DB, PC | 232 | 0 | 0 | Atar [64] |
| 10. Dynamics and repair | |||||
| Stem cell tranfer | R, DB, PC | 67 | 0 | Janssens [65] | |
| R, DB, PC | 54 | 0 | Dill [66] | ||
| R, OL, PC | 101 | 0 | 0 | Roncalli [67] | |
| R, OL, PC | 200 | 0 | 0 | Hirsch [68] | |
| R, OL, PC | 200 | 0 | 0 | Surder [69] | |
| R, OL, PC | 120 | 0 | 0 | San Roman [70] | |
| R, DB, PC | 42 | 0 | 0 | Wohrle [71] | |
| Angiogenesis modulation † | |||||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rios-Navarro, C.; Marcos-Garces, V.; Bayes-Genis, A.; Husser, O.; Nuñez, J.; Bodi, V. Microvascular Obstruction in ST-Segment Elevation Myocardial Infarction: Looking Back to Move Forward. Focus on CMR. J. Clin. Med. 2019, 8, 1805. https://doi.org/10.3390/jcm8111805
Rios-Navarro C, Marcos-Garces V, Bayes-Genis A, Husser O, Nuñez J, Bodi V. Microvascular Obstruction in ST-Segment Elevation Myocardial Infarction: Looking Back to Move Forward. Focus on CMR. Journal of Clinical Medicine. 2019; 8(11):1805. https://doi.org/10.3390/jcm8111805
Chicago/Turabian StyleRios-Navarro, Cesar, Victor Marcos-Garces, Antoni Bayes-Genis, Oliver Husser, Julio Nuñez, and Vicente Bodi. 2019. "Microvascular Obstruction in ST-Segment Elevation Myocardial Infarction: Looking Back to Move Forward. Focus on CMR" Journal of Clinical Medicine 8, no. 11: 1805. https://doi.org/10.3390/jcm8111805