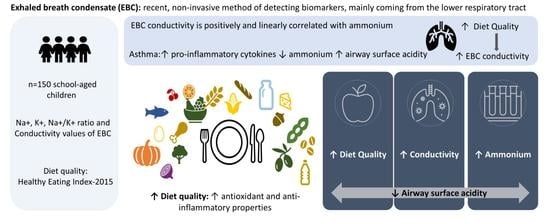
Diet Quality and Exhaled Breath Condensate Markers in a Sample of School-Aged Children
Abstract
:1. Introduction
2. Materials and Methods
2.1. Dietary and Diet Quality Assessment
Supplementation
2.2. Anthropometry
2.3. Socio-Economic Data
2.4. Collection and Analysis of the Exhaled Breath Condensate
2.5. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Konstantinidi, E.M.; Lappas, A.S.; Tzortzi, A.S.; Behrakis, P.K. Exhaled Breath Condensate: Technical and Diagnostic Aspects. Sci. World J. 2015, 2015, 435160. [Google Scholar] [CrossRef] [Green Version]
- Kharitonov, S.A.; Barnes, P.J. Exhaled markers of pulmonary disease. Am. J. Respir. Crit. Care Med. 2001, 163, 1693–1722. [Google Scholar] [CrossRef] [Green Version]
- Davis, M.D.; Montpetit, A.J. Exhaled Breath Condensate: An Update. Immunol. Allergy Clin. N. Am. 2018, 38, 667–678. [Google Scholar] [CrossRef]
- Maniscalco, M.; Fuschillo, S.; Paris, D.; Cutignano, A.; Sanduzzi, A.; Motta, A. Clinical metabolomics of exhaled breath condensate in chronic respiratory diseases. Adv. Clin. Chem. 2019, 88, 121–149. [Google Scholar] [PubMed]
- Jayaraman, S.; Song, Y.; Verkman, A.S. Airway surface liquid osmolality measured using fluorophore-encapsulated liposomes. J. Gen. Physiol. 2001, 117, 423–430. [Google Scholar] [CrossRef]
- Parent, R.A. Comparative Biology of the Normal Lung, 2nd ed.; Academic Press: Cambridge, MA, USA, 2015. [Google Scholar]
- Fischer, H.; Widdicombe, J.H. Mechanisms of acid and base secretion by the airway epithelium. J. Membr. Biol. 2006, 211, 139–150. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zajac, M.; Dreano, E.; Edwards, A.; Planelles, G.; Sermet-Gaudelus, I. Airway Surface Liquid pH Regulation in Airway Epithelium Current Understandings and Gaps in Knowledge. Int. J. Mol. Sci. 2021, 22, 3384. [Google Scholar] [CrossRef]
- Wang, W.; Ji, H.L. Epithelial Sodium and Chloride Channels and Asthma. Chin. Med. J. 2015, 128, 2242–2249. [Google Scholar] [CrossRef] [PubMed]
- Hirota, S.A.; Janssen, L.J. Sodium and asthma: Something borrowed, something new? Am. J. Physiol. Lung Cell. Mol. Physiol. 2007, 293, L1369-73. [Google Scholar] [CrossRef] [Green Version]
- Dressel, H.; Müller, F.; Fischer, R.; Römmelt, H.; Hohlfeld, J.M.; Behr, J.; Huber, R.M.; Nowak, D.; Jörres, R.A. Independent information of nonspecific biomarkers in exhaled breath condensate. Respiration 2010, 80, 401–409. [Google Scholar] [CrossRef] [PubMed]
- MacGregor, G.; Ellis, S.; Andrews, J.; Imrie, M.; Innes, A.; Greening, A.P.; Cunningham, S. Breath condensate ammonium is lower in children with chronic asthma. Eur. Respir. J. 2005, 26, 271–276. [Google Scholar] [CrossRef] [Green Version]
- Hunt, J.F.; Erwin, E.; Palmer, L.; Vaughan, J.; Malhotra, N.; Platts-Mills, T.A.; Gaston, B. Expression and activity of pH-regulatory glutaminase in the human airway epithelium. Am. J. Respir. Crit. Care Med. 2002, 165, 101–107. [Google Scholar] [CrossRef] [PubMed]
- Wallace, T.C.; Bailey, R.L.; Blumberg, J.B.; Burton-Freeman, B.; Chen, C.O.; Crowe-White, K.M.; Drewnowski, A.; Hooshmand, S.; Johnson, E.; Lewis, R.; et al. Fruits, vegetables, and health: A comprehensive narrative, umbrella review of the science and recommendations for enhanced public policy to improve intake. Crit. Rev. Food Sci. Nutr. 2020, 60, 2174–2211. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Berthon, B.S.; Macdonald-Wicks, L.K.; Gibson, P.G.; Wood, L.G. Investigation of the association between dietary intake, disease severity and airway inflammation in asthma. Respirology 2013, 18, 447–454. [Google Scholar] [CrossRef] [Green Version]
- Biagini, D.; Fusi, J.; Vezzosi, A.; Oliveri, P.; Ghimenti, S.; Lenzi, A.; Salvo, P.; Daniele, S.; Scarfò, G.; Vivaldi, F.; et al. Effects of long-term vegan diet on breath composition. J. Breath Res. 2022, 16, 026004. [Google Scholar] [CrossRef] [PubMed]
- Krilaviciute, A.; Leja, M.; Kopp-Schneider, A.; Barash, O.; Khatib, S.; Amal, H.; Broza, Y.Y.; Polaka, I.; Parshutin, S.; Rudule, A.; et al. Associations of diet and lifestyle factors with common volatile organic compounds in exhaled breath of average-risk individuals. J. Breath Res. 2019, 13, 026006. [Google Scholar] [CrossRef] [PubMed]
- Baranska, A.; Tigchelaar, E.; Smolinska, A.; Dallinga, J.W.; Moonen, E.J.; Dekens, J.A.; Wijmenga, C.; Zhernakova, A.; van Schooten, F.J. Profile of volatile organic compounds in exhaled breath changes as a result of gluten-free diet. J. Breath Res. 2013, 7, 037104. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.J.; Pahl, M.V.; Vaziri, N.D.; Blake, D.R. Effect of hemodialysis and diet on the exhaled breath methanol concentration in patients with ESRD. J. Ren. Nutr. 2012, 22, 357–364. [Google Scholar] [CrossRef] [PubMed]
- Spacek, L.A.; Mudalel, M.L.; Lewicki, R.; Tittel, F.K.; Risby, T.H.; Stoltzfus, J.; Munier, J.J.; Solga, S.F. Breath ammonia and ethanol increase in response to a high protein challenge. Biomarkers 2015, 20, 149–156. [Google Scholar] [CrossRef]
- Spacek, L.A.; Strzepka, A.; Saha, S.; Kotula, J.; Gelb, J.; Guilmain, S.; Risby, T.; Solga, S.F. Repeated Measures of Blood and Breath Ammonia in Response to Control, Moderate and High Protein Dose in Healthy Men. Sci. Rep. 2018, 8, 2554. [Google Scholar] [CrossRef]
- Raninen, K.J.; Lappi, J.E.; Mukkala, M.L.; Tuomainen, T.P.; Mykkänen, H.M.; Poutanen, K.S.; Raatikainen, O.J. Fiber content of diet affects exhaled breath volatiles in fasting and postprandial state in a pilot crossover study. Nutr. Res. 2016, 36, 612–619. [Google Scholar] [CrossRef]
- Rava, M.; Varraso, R.; Decoster, B.; Huyvaert, H.; Le Moual, N.; Jacquemin, B.; Künzli, N.; Kauffmann, F.; Zerimech, F.; Matran, R.; et al. Plasma and exhaled breath condensate nitrite-nitrate level in relation to environmental exposures in adults in the EGEA study. Nitric Oxide 2012, 27, 169–175. [Google Scholar] [CrossRef] [Green Version]
- Mendes, F.C.; Paciência, I.; Cavaleiro Rufo, J.; Silva, D.; Delgado, L.; Moreira, A.; Moreira, P. Dietary Acid Load Modulation of Asthma-Related miRNAs in the Exhaled Breath Condensate of Children. Nutrients 2022, 14, 1147. [Google Scholar] [CrossRef] [PubMed]
- Greguš, M.; Foret, F.; Kindlová, D.; Pokojová, E.; Plutinský, M.; Doubková, M.; Merta, Z.; Binková, I.; Skřičková, J.; Kubáň, P. Monitoring the ionic content of exhaled breath condensate in various respiratory diseases by capillary electrophoresis with contactless conductivity detection. J. Breath Res. 2015, 9, 027107. [Google Scholar] [CrossRef]
- Guilleminault, L.; Williams, E.J.; Scott, H.A.; Berthon, B.S.; Jensen, M.; Wood, L.G. Diet and Asthma: Is It Time to Adapt Our Message? Nutrients 2017, 9, 1227. [Google Scholar] [CrossRef] [Green Version]
- Andrianasolo, R.M.; Kesse-Guyot, E.; Adjibade, M.; Hercberg, S.; Galan, P.; Varraso, R. Associations between dietary scores with asthma symptoms and asthma control in adults. Eur. Respir. J. 2018, 52, 1702572. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reyes-Angel, J.; Han, Y.Y.; Litonjua, A.A.; Celedón, J.C. Diet and asthma: Is the sum more important than the parts? J. Allergy Clin. Immunol. 2021, 148, 706–707. [Google Scholar] [CrossRef]
- Mendes, F.C.; Paciência, I.; Cavaleiro Rufo, J.; Farraia, M.; Silva, D.; Padrão, P.; Delgado, L.; Garcia-Larsen, V.; Moreira, A.; Moreira, P. Higher diversity of vegetable consumption is associated with less airway inflammation and prevalence of asthma in school-aged children. Pediatr. Allergy Immunol. 2021, 32, 925–936. [Google Scholar] [CrossRef] [PubMed]
- Walker, J.L.; Ardouin, S.; Burrows, T. The validity of dietary assessment methods to accurately measure energy intake in children and adolescents who are overweight or obese: A systematic review. Eur. J. Clin. Nutr. 2018, 72, 185–197. [Google Scholar] [CrossRef]
- Krebs-Smith, S.M.; Pannucci, T.E.; Subar, A.F.; Kirkpatrick, S.I.; Lerman, J.L.; Tooze, J.A.; Wilson, M.M.; Reedy, J. Update of the Healthy Eating Index: HEI-2015. J. Acad. Nutr. Diet. 2018, 118, 1591–1602. [Google Scholar] [CrossRef]
- Xu, Z.; Steffen, L.M.; Selvin, E.; Rebholz, C.M. Diet quality, change in diet quality and risk of incident CVD and diabetes. Public Health Nutr. 2020, 23, 329–338. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Agriculture, Agricultural Research Service; Food Surveys Research Group Home Page. USDA Food and Nutrient Database for Dietary Studies 2017–2018. 2020. Available online: https://www.ars.usda.gov/nea/bhnrc/fsrg (accessed on 20 July 2022).
- De Castro Mendes, F.; Paciência, I.; Rufo, J.C.; Silva, D.; Cunha, P.; Farraia, M.; Delgado, L.; Moreira, P.; Moreira, A. Asthma and body mass definitions affect estimates of association: Evidence from a community-based cross-sectional survey. ERJ Open Res. 2019, 5. [Google Scholar] [CrossRef] [PubMed]
- Kuczmarski, R.J.; Ogden, C.L.; Grummer-Strawn, L.M.; Flegal, K.M.; Guo, S.S.; Wei, R.; Mei, Z.; Curtin, L.R.; Roche, A.F.; Johnson, C.L. CDC Growth Charts: United States; Advance Data; US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics: Atlanta, GA, USA, 2000; 314, pp. 1–27.
- De Castro Mendes, F.; Paciência, I.; Rufo, J.C.; Farraia, M.; Silva, D.; Padrão, P.; Delgado, L.; Garcia-Larsen, V.; Moreira, A.; Moreira, P. Increasing Vegetable Diversity Consumption Impacts the Sympathetic Nervous System Activity in School-Aged Children. Nutrients 2021, 13, 1456. [Google Scholar] [CrossRef] [PubMed]
- Cavaleiro Rufo, J.; Paciência, I.; Mendes, F.C.; Farraia, M.; Rodolfo, A.; Silva, D.; de Oliveira Fernandes, E.; Delgado, L.; Moreira, A. Exhaled breath condensate volatilome allows sensitive diagnosis of persistent asthma. Allergy 2019, 74, 527–534. [Google Scholar] [CrossRef]
- Liu, J.; Thomas, P.S. Relationship between exhaled breath condensate volume and measurements of lung volumes. Respiration 2007, 74, 142–145. [Google Scholar] [CrossRef]
- Downs, C. Chapter 2—Ion Transport and Lung Fluid Balance. In Lung Epithelial Biology in the Pathogenesis of Pulmonary Disease; Sidhaye, V.K., Koval, M., Eds.; Academic Press: Boston, MA, USA, 2017; pp. 21–31. [Google Scholar]
- Koczulla, A.R.; Noeske, S.; Herr, C.; Jörres, R.A.; Römmelt, H.; Vogelmeier, C.; Bals, R. Acute and chronic effects of smoking on inflammation markers in exhaled breath condensate in current smokers. Respiration 2010, 79, 61–67. [Google Scholar] [CrossRef] [Green Version]
- Hunt, J.F.; Fang, K.; Malik, R.; Snyder, A.; Malhotra, N.; Platts-Mills, T.A.; Gaston, B. Endogenous airway acidification. Implications for asthma pathophysiology. Am. J. Respir. Crit. Care Med. 2000, 161 Pt 1, 694–699. [Google Scholar] [CrossRef] [PubMed]
- Carraro, S.; Folesani, G.; Corradi, M.; Zanconato, S.; Gaston, B.; Baraldi, E. Acid-base equilibrium in exhaled breath condensate of allergic asthmatic children. Allergy 2005, 60, 476–481. [Google Scholar] [CrossRef]
- Hunt, J. Exhaled Breath Condensate pH. Am. J. Respir. Crit. Care Med. 2006, 173, 366–367. [Google Scholar] [CrossRef]
- Rama, T.A.; Paciência, I.; Cavaleiro Rufo, J.; Silva, D.; Cunha, P.; Severo, M.; Padrão, P.; Moreira, P.; Delgado, L.; Moreira, A. Exhaled breath condensate pH determinants in school-aged children: A population-based study. Pediatr. Allergy Immunol. 2021, 32, 1474–1481. [Google Scholar] [CrossRef]
- Hunt, J. Exhaled breath condensate: An evolving tool for noninvasive evaluation of lung disease. J. Allergy Clin. Immunol. 2002, 110, 28–34. [Google Scholar] [CrossRef] [PubMed]
- Kullmann, T.; Barta, I.; Antus, B.; Horváth, I. Drinking influences exhaled breath condensate acidity. Lung 2008, 186, 263–268. [Google Scholar] [CrossRef]
- Bikov, A.; Pako, J.; Montvai, D.; Kovacs, D.; Koller, Z.; Losonczy, G.; Horvath, I. Exhaled breath condensate pH decreases following oral glucose tolerance test. J. Breath Res. 2015, 9, 047112. [Google Scholar] [CrossRef] [PubMed]
- Lačná, J.; Ďurč, P.; Greguš, M.; Skřičková, J.; Doubková, M.; Pokojová, E.; Kindlová, D.; Dolina, J.; Konečný, Š.; Foret, F.; et al. Capillary electrophoretic analysis of ionic content in exhaled breath condensate and pH monitoring as a non-invasive method in gastroesophageal reflux disease diagnostics. J. Chromatogr. B 2019, 1134–1135, 121857. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Teague, W.G.; Erzurum, S.; Fitzpatrick, A.; Mantri, S.; Dweik, R.A.; Bleecker, E.R.; Meyers, D.; Busse, W.W.; Calhoun, W.J.; et al. Determinants of exhaled breath condensate pH in a large population with asthma. Chest 2011, 139, 328–336. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Horváth, I.; Hunt, J.; Barnes, P.J.; Alving, K.; Antczak, A.; Baraldi, E.; Becher, G.; van Beurden, W.J.; Corradi, M.; Dekhuijzen, R.; et al. Exhaled breath condensate: Methodological recommendations and unresolved questions. Eur. Respir. J. 2005, 26, 523–548. [Google Scholar] [CrossRef] [Green Version]
- Shim, J.S.; Oh, K.; Kim, H.C. Dietary assessment methods in epidemiologic studies. Epidemiol. Health 2014, 36, e2014009. [Google Scholar] [CrossRef] [Green Version]
- Ortega, R.M.; Pérez-Rodrigo, C.; López-Sobaler, A.M. Dietary assessment methods: Dietary records. Nutr. Hosp. 2015, 31 (Suppl. S3), 38–45. [Google Scholar]
- Foster, E.; Bradley, J. Methodological considerations and future insights for 24-hour dietary recall assessment in children. Nutr. Res. 2018, 51, 1–11. [Google Scholar] [CrossRef]
- Biró, G.; Hulshof, K.F.; Ovesen, L.; Amorim Cruz, J.A. Selection of methodology to assess food intake. Eur. J. Clin. Nutr. 2002, 56 (Suppl. S2), S25–S32. [Google Scholar] [CrossRef] [Green Version]
- Wolper, C.H.S.; Heymsfield, S.B. Measuring Food Intake: An Overview. In Handbook of Assessment Methods for Eating Behaviors and Weight-Related Problems: Measures, Theory, and Research; Sage Publications, Inc.: Thousand Oaks, CA, USA, 1995. [Google Scholar]
- Al-Ibrahim, A.A.; Jackson, R.T. Healthy eating index versus alternate healthy index in relation to diabetes status and health markers in U.S. adults: NHANES 2007–2010. Nutr. J. 2019, 18, 26. [Google Scholar] [CrossRef] [PubMed]
- Kirkpatrick, S.I.; Dodd, K.W.; Potischman, N.; Zimmerman, T.P.; Douglass, D.; Guenther, P.M.; Durward, C.; Atoloye, A.T.; Kahle, L.L.; Subar, A.F.; et al. Healthy Eating Index-2015 Scores Among Adults Based on Observed vs Recalled Dietary Intake. J. Acad. Nutr. Diet. 2021, 121, 2233–2241.e1. [Google Scholar] [CrossRef]
- Müller, M.J.; Lagerpusch, M.; Enderle, J.; Schautz, B.; Heller, M.; Bosy-Westphal, A. Beyond the body mass index: Tracking body composition in the pathogenesis of obesity and the metabolic syndrome. Obes. Rev. 2012, 13 (Suppl. S2), 6–13. [Google Scholar] [CrossRef]
- Papoutsakis, C.; Priftis, K.N.; Drakouli, M.; Prifti, S.; Konstantaki, E.; Chondronikola, M.; Antonogeorgos, G.; Matziou, V. Childhood Overweight/Obesity and Asthma: Is There a Link? A Systematic Review of Recent Epidemiologic Evidence. J. Acad. Nutr. Diet. 2013, 113, 77–105. [Google Scholar] [CrossRef] [PubMed]
- Lundahl, A.; Kidwell, K.M.; Nelson, T.D. Parental underestimates of child weight: A meta-analysis. Pediatrics 2014, 133, e689–e703. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Silva, D.; Severo, M.; Paciência, I.; Rufo, J.; Martins, C.; Moreira, P.; Padrão, P.; Delgado, L.; Moreira, A. Setting definitions of childhood asthma in epidemiologic studies. Pediatr. Allergy Immunol. 2019, 30, 708–715. [Google Scholar] [CrossRef]
- Barros, R.; Moreira, A.; Padrão, P.; Teixeira, V.H.; Carvalho, P.; Delgado, L.; Lopes, C.; Severo, M.; Moreira, P. Dietary patterns and asthma prevalence, incidence and control. Clin. Exp. Allergy 2015, 45, 1673–1680. [Google Scholar] [CrossRef]


| Total, n = 150 | Girls, n = 73 (48.7%) | Boys, n = 77 (51.3.%) | p Value | |
|---|---|---|---|---|
| Age (years), mean ± SD | 8.67 ± 0.75 | 8.61 ± 0.71 | 8.74 ± 0.78 | 0.283 |
| BMI | 0.540 | |||
| Non-overweight/obese (p < 85th) | 97 (64.2%) | 49 (67.1%) | 48 (62.3%) | |
| Overweight/obese (p ≥ 85th) | 53 (35.3%) | 24 (32.9%) | 29 (37.7%) | |
| HEI-2015 score, mean ± SD | 59.94 ± 11.63 | 60.01 ± 11.46 | 59.88 ± 11.87 | 0.943 |
| Carbohydrates, %VET | 50.29 ± 6.26 | 50.94 ± 5.54 | 49.67 ± 6.85 | 0.209 |
| Protein, %VET | 17.48 ± 3.51 | 17.69 ± 3.38 | 17.37 ± 3.64 | 0.481 |
| Fat %VET | 29.26 ± 5.59 | 28.48 ± 5.65 | 29.99 ± 5.48 | 0.097 |
| MONO %VET | 10.43 ± 2.81 | 10.01 ± 2.57 | 10.82 ± 2.99 | 0.075 |
| POLI %VET | 3.98 ± 1.56 | 3.80 ± 1.56 | 4.16 ± 1.55 | 0.161 |
| SATURATED %VET | 9.17 ± 2.94 | 9.18 ± 3.05 | 9.17 ± 2.85 | 0.968 |
| Fiber (g), median (25th–75th) | 18.69 (14.75–23.98) | 19.70 (15.77–24.43) | 18.45 (14.22–23.34) | 0.346 |
| Sodium (mg), median (25th–75th) | 1978.28 (1598.02–2707.48) | 1838.67 (1484.53–2551.02) | 2104.24 (1720.35–2867.94) | 0.078 |
| Total energy intake (kcal), mean ± SD | 2236.03 ± 465.03 | 2181.69 ± 488.04 | 2287.54 ± 439.09 | 0.164 |
| Nutritional Supplementation a, n (%) | 22 (16.5%) | 11 (17.7%) | 11 (15.5%) | 0.728 |
| Asthma: Medical diagnosis with asthma symptoms or +BD b | 25 (16.7%) | 16 (21.9%) | 9 (11.7%) | 0.093 |
| Parental education c, n (%) | 0.984 | |||
| <9 years | 43 (35.5%) | 20 (36.4%) | 23 (34.8%) | |
| 10–12 years | 51 (42.1%) | 23 (41.8%) | 28 (42.4%) | |
| >12 years | 27 (22.3%) | 12 (21.8%) | 15 (22.7%) | |
| Exhaled Breath Markers | ||||
| Na+, median (25th–75th) | 39.00 (28.75–47.25) | 40.00 (29.38–47.75) | 38.00 (26.50–46.50) | 0.657 |
| K+, median (25th–75th) | 11.00 (4.00–50.50) | 8.67 (4.18–49.00) | 11.00 (4.00–55.00) | 0.523 |
| Conductivity, median (25th–75th) | 0.10 (0.06–0.18) | 0.08 (0.05–0.16) | 0.12 (0.08–0.24) | 0.010 * |
| Na+/K+ ratio, median (25th–75th) | 3.15 (0.67–9.08) | 3.60 (0.63–9.80) | 2.79 (0.84–8.05) | 0.559 |
| HEI Score: CrudeModel OR (95% CI) | HEI Score Tertiles: CrudeModel OR (95% CI) | HEI Score: aOR (95% CI) | HEI Score Tertiles: aOR (95% CI) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Continuous | >54.53 and ≤65.37 | >65.37 | Continuous | p Value | Reference ≤ 54.53 | >54.53 and ≤65.37 | p Value | >65.37 | p Value | |
| Na+ | 1.01 (0.98; 1.03) | 1.24 (0.55; 2.81) | 0.88 (0.41; 1.9) | 1.01 (0.98; 1.04) | 0.640 | 1 | 1.29 (0.36, 4.63) | 0.694 | 1.26 (0.39, 4.11) | 0.702 |
| K+ | 0.99 (0.96; 1.02) | 1.31 (0.58; 2.99) | 0.54 (0.25; 1.19) | 0.998 (0.97; 1.03) | 0.885 | 1 | 1.64 (0.44, 6.05) | 0.462 | 0.78 (0.22, 2.8) | 0.704 |
| Na+/K+ ratio | 1.01 (0.98; 1.03) | 0.53 (0.23; 1.22) | 1.46 (0.67; 3.17) | 1.00 (0.97; 1.04) | 0.932 | 1 | 0.5 (0.13, 1.88) | 0.304 | 1.37 (0.38, 4.98) | 0.628 |
| Conductivity | 1.02 (1.00; 1.05) | 1.74 (0.77; 3.97) | 1.95 (0.9; 4.26) | 1.04 (1.00; 1.08) | 0.037 * | 1 | 1.66 (0.65, 4.27) | 0.742 | 4.55 (1.12, 18.45) | 0.034 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodrigues, M.; de Castro Mendes, F.; Paciência, I.; Cavaleiro Rufo, J.; Silva, D.; Delgado, L.; Moreira, A.; Moreira, P. Diet Quality and Exhaled Breath Condensate Markers in a Sample of School-Aged Children. Children 2023, 10, 263. https://doi.org/10.3390/children10020263
Rodrigues M, de Castro Mendes F, Paciência I, Cavaleiro Rufo J, Silva D, Delgado L, Moreira A, Moreira P. Diet Quality and Exhaled Breath Condensate Markers in a Sample of School-Aged Children. Children. 2023; 10(2):263. https://doi.org/10.3390/children10020263
Chicago/Turabian StyleRodrigues, Mónica, Francisca de Castro Mendes, Inês Paciência, João Cavaleiro Rufo, Diana Silva, Luís Delgado, André Moreira, and Pedro Moreira. 2023. "Diet Quality and Exhaled Breath Condensate Markers in a Sample of School-Aged Children" Children 10, no. 2: 263. https://doi.org/10.3390/children10020263