Abstract
Previous studies have shown that demand for the quantity of medical services has increased since the implementation of the National Health Insurance (NHI) programme. This paper extends the investigation to the relationship between private health insurance and inpatient service utilisation under the NHI programme in Taiwan. By using nationwide population-based claim data, we utilise a two-part model to investigate whether individuals with private health insurance have higher probabilities of utilising inpatient services. We further examine the effect of those individuals with private health insurance on the inpatient length of stay for those utilising inpatient services. The results indicate that individuals with private health insurance are more likely to use inpatient services and spend more days in a hospital compared to those without private health insurance. We propose that this finding provides a good reference for government and insurance companies when formulating relevant health insurance policies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Taiwan’s National Health Insurance (NHI) programme was implemented in March 1995 with the goal of providing every citizen with equal access to comprehensiveFootnote 1 medical services regardless of their socio-economic status. Since then, the utilisation of medical services has greatly increased.Footnote 2 In Taiwan, the health-care delivery system is market-driven with a mix of publicly and privately owned hospitals. Under the NHI programme, medical institutions are categorised into four different levels—medical centre, regional hospital, district hospital and clinics—based on the management, administrative processes, volume, infrastructure, capacity, manpower and performance evaluation regardless of whether they are public or private.Footnote 3 There are no gatekeepers regulating access to health-care services and every citizen has free range to choose public or private hospitals and physicians with equal quality treatments under the NHI programme.
The NHI programme provides all necessary medical treatments to the beneficiaries and requires users to pay premiums and co-payments when utilising medical services in order to control the costs within the medical care sector and discourage moral hazard problems. However, there are also self-paid items for the insured to obtain higher quality treatments in terms of products or services. For example, the NHI only covers the costs associated with hospitalisation in non-private rooms with three or more beds and upgrading to a private room is allowed at extra cost to the patients. These types of “added value services” are primarily available through private health insurance, providing incentives for individuals to purchase supplementary private health insurance to acquire better accommodation, to access a different type or quality of care, or to avoid catastrophic health expenses. People already covered by NHI may seek supplemental private health insurance to pay for the costs of medical treatment, drugs and services not covered by the NHI. Thus, private health insurance serves as a financial buffer for potential changes and adjustments within the NHI programme.
There indeed exists an increasing demand for private health insurance in Taiwan as the purchase rate of households obtaining private health insurance increased to 72.3 per cent in 2004 compared with 63.9 per cent in 1993.Footnote 4 Private insurers often sell insurance coverage for hospitalisation and surgical care, but not outpatient visits, and most private health insurance firms only cover inpatient care with a fixed payment scheme per diem.Footnote 5 In other words, a private health insurance contract not only provides a cost reduction when the insured utilises the inpatient services, but also offers incentives for the insured to increase hospital stays to obtain more reimbursements.
The effect of health insurance on stimulating excess medical care demand is well known as a moral hazard problem.Footnote 6 A trade-off exists between the gains from risk reduction and the moral hazard in relation to health insurance.Footnote 7 Previous studies have shown that the extent of this trade-off is based on the variations in the degree of risk aversion and the price elasticity of demand for health care.Footnote 8 Presumably, the greater the aversion to risk, the greater the reduction in health insurance risk faced by the individual. Thus, the larger the price elasticity, the greater the welfare loss resulting from the more generous health insurance—which is the so-called moral hazard phenomenon.
Since the purchase of private health insurance might be an endogenous decision, examining the moral hazard issues in regard to the demand for health services while treating private health insurance as an exogenous variable, may lead to upward bias.Footnote 9 In order to reduce the uncertainty associated with examining the effect of health insurance on the demand for health services as well as holding private insurance to being perhaps an endogenous decision, RAND designed a Health Insurance Experiment in 1974.Footnote 10 This experiment randomly assigned individuals to different insurance plans with varied co-payments and deductibles. On the basis of various settings of the co-insurance rate and the price elasticity of health service demand, the welfare loss arising possibly from the trade-off was found to be small.Footnote 11 The results indicate that the experiment provides weak evidence of generous health insurance coverage and large medical expenditure.9
Since the theoretical predication of the relationship between health insurance and health service utilisation may depend on assumptions of different levels of risk aversion as well as the price elasticity, this issue remains in need of further empirical investigation. Several studies have shown that the moral hazard problem may be present as individuals tend to utilise more health services such as physician visits, admissions to hospital and hospitalisation stays when they have more generous insurance coverage.Footnote 12 While most of the above studies are mainly concerned with moral hazard issues relating to partial public and/or private health insurance under the co-existence of public and private hospitals, little is known about the relationship between private health insurance and medical service utilisation under a NHI programme. Specifically, the NHI programme in Taiwan provides every citizen with equal access to comprehensive medical services regardless of whether the hospital is public or private. This paper thus aims at investigating the relationship between private health insurance and inpatient service utilisation under this NHI programme, which would shed some light on moral hazard issues from the interaction of public and private health insurance in health-care provision.
In this paper we use population-based nationwide claim data from the 2005 Taiwan National Health Insurance Research Database (NHIRD), linked with the 2005 National Health Interview Survey (NHIS), to empirically study the moral hazard problem. We set out in this study to utilise a two-part model, because the decision to receive inpatient services and the duration of a single episode of hospitalisation are not jointly determined.Footnote 13 Therefore, we first investigate whether individuals with private health insurance have higher probabilities of utilising inpatient services. Second, we analyse the effect of those individuals with private health insurance on the inpatient length of stay for those utilising inpatient services. Previous studies have shown that the severity of illness and diagnosis-related groups are important determinants in length of stay.Footnote 14 Consequently, we control for the clusters of the ICD-9 procedure codesFootnote 15 in order to obtain more critical estimates of the moral hazard phenomenon given that each patient with a similar ICD-9 procedure code is located in a clinically meaningful category.
Because financial deficits are a primary concern within Taiwan’s NHI programme and inpatient services as a proportion of the overall medical expenditure are high,Footnote 16 investigating the relationship between private health insurance and inpatient service utilisation should be important for mitigating the financial deficits of the NHI programme in Taiwan. Buchmueller and CouffinhalFootnote 17 pointed out that when France’s government faced chronic financial deficits in the public health programme, the government was willing to reform the system by shifting coverage of certain treatments from public to private health insurance. Therefore, understanding the relationship between private health insurance and inpatient service utilisation is critical since it may affect businesses of the private health insurance industry and may eventually impact the policy scheme within the NHI programme.
The remainder of this paper is organised as follows. The next section presents a brief overview of the private health insurance market and the NHI programme in Taiwan. This is followed by a section presenting the data and the empirical methodology. The results are then provided, followed by a discussion and concluding remarks.
Health insurance in Taiwan
Private health insurance
Private health insurance was first introduced to Taiwan in 1967. From 1967 to 1985, there were at most six domestic private health insurance companies operating on the island. In 1986, Taiwan’s government allowed American health insurance companies to set up branches locally. At that time, there were six domestic and 13 foreign firms covering the local market. In 1994, the market was opened to all foreign private insurance companies, and by 1998 there were 16 domestic and 17 foreign firms doing business in Taiwan.Footnote 18 Foreign firms gradually decreased from 16 to seven firms, while the domestic firms slowly rose from 16 to 23 between 2000 and 2010.Footnote 19 When private health insurance was first introduced to the public in Taiwan, the proportion of residents who purchased private health insurance was low. The demand for private health insurance rose, as the purchase rate of households obtaining private health insurance increased to 72.3 per cent in 2004 compared with 63.9 per cent in 1993.4 Private health insurance premium incomes increased gradually as well. From Figure 1, the yearly growth rate of premium income brought in by private health insurance increased by 128.7 per cent in 1977, by 60.1 per cent in 1987 and by 49.3 per cent in 1994. After the introduction of the NHI, the yearly growth rate remained as high as or higher than 30 per cent prior to 2000, but gradually declined to 6.5 per cent in 2010.19
Life insurance companies in Taiwan often sell health insurance products, such as hospitalisation insurance that covers the inpatient expenditure with a fixed payment scheme per diem.Footnote 20 Specifically, private health insurance policy in Taiwan is usually designed with clauses in the form of unlimited coverage throughout the whole lifespan, that is individuals with private health insurance can obtain reimbursements from insurance companies with a fixed payment scheme per diem when they are hospitalised until their life ends.Footnote 21 In 2007, insurers began to provide an “account-based” health insurance policy in the insurance market.21 This type of health insurance policy automatically expires when the amount of the health account is depleted. There is also short-term health insurance whereby the duration only covers a specific period. Under this insurance coverage, individuals have to offer receipts when claiming reimbursements from insurers since payment is based on the actual expenditure.
National Health Insurance
Taiwan’s NHI was established in March 1995. The programme is administrated by the government and is a unique single-payer social insurance programme. Before the implementation of NHI, there were three major social health insurance programmes including labour insurance (covering 40.12 per cent of the population), government employees’ insurance (covering 8.06 per cent of the population) and farmers’ health insurance (covering 8.21 per cent of the population). However, there were still an estimated 8 million people in Taiwan, or about 42 per cent of the total population, who had no health insurance coverage.Footnote 22
In order to eliminate the financial barriers to medical services caused by poverty, the government thus integrated the various social health insurance programmes into an inclusive and universal public NHI programme. Since participation in NHI is compulsory, the coverage rate increased to 99.5 per cent in 2010 compared to the initial 92.34 per cent in 1995.Footnote 23
The Bureau of National Health Insurance (BNHI) operates the NHI programme. The BNHI collects premiums from the insured. In 2010 the total revenue of the NHI programme was NT$461 billion, with 95 per cent coming from premiums and the remaining 5 per cent from the health surcharge on cigarettes, contributions from public welfare lotteries and investment income. The total expenditure of the NHI programme in 2010 was NT$500 billion, which includes outpatient services at NT$336 billion (67.15 per cent) and inpatient services at NT$164 billion (32.85 per cent). The trend for total expenditures being greater than the total revenue of the NHI programme in recent years is due to the growing aged population. According to statistics from the Ministry of the Interior in Taiwan, the number of aged population (those 65 years old or above) was about 2.49 million at the end of 2010, which accounts for 10.74 per cent of the total population. With the increasing risk of chronic diseases among the elderly, higher medical expenditures are expected. In more specific terms, in 2010 the share of all medical expenditures accounted for by those aged 65 years or above was 36.59 per cent of total expenditures, despite this group accounting for just 10.74 per cent of the total population.23 Therefore, financial deficits have become the primary concern within Taiwan’s NHI programme.
The NHI programme covers certain percentages of hospitalisation expenses when the insured get hospitalised. The insured still has to pay co-payments. The inpatient co-payment depends on the type of ailment (acute or chronic) and length of stay.Footnote 24 Furthermore, the NHI programme only covers “standard beds”, that is a hospital room with three or more beds when the insured is hospitalised. In order to look for better accommodation and due to the availability of “standard beds” in each hospital, patients are able to upgrade to a partially insured room with only one or two beds and pay the difference between the actual expense and the amount covered by the NHI programme for the “standard bed”. Therefore, life insurance companies often sell hospitalisation insurance that covers the inpatient expenditure with a fixed payment scheme per diem. Hospitalisation insurance may offer incentives for the insured to increase hospital admissions and length of stay so as to obtain more reimbursements.
Empirical model
Data resources and study sample
Our data was obtained from two secondary resources. The first was the 2005 NHIS. Using face-to-face interviews and a multi-stage stratified systematic sampling design method, the NHIS was sourced from the National Health Research Institute (NHRI) and the Bureau of Health Promotion within the Department of Health in Taiwan. The 2005 NHIS provides nationwide detailed population information on a series of individual characteristics, including age, gender, marital status, educational attainment and income, as well as detailed information on personal health conditions and other types of health-related behaviour. The NHIS comprises 24,276 individuals, with the number of those aged below 12 and above 65 years old being 3,900 and 2,727, respectively.
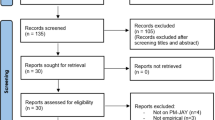
The second database used in this study was released by the NHRI directly. The NHRI created this database by drawing data from the 2005 Taiwan NHIRD and linking it with the 2005 NHIS. The NHIRD database is one of the largest and most comprehensive population-based data sources that includes registries of medical facilities contracted with the BNHI, board-certified physicians, a monthly claim summary for all inpatient/outpatient claims, details of all inpatient/outpatient orders and expenditures on prescriptions dispensed at contracted pharmacies. We select a sample of adults and elderly people aged above 20 in our analysis. After discarding all missing or incomplete observations, we take a total of 12,006 individuals from the 2005 NHIS database, of which 731 subjects were reported to have utilised inpatient services in 2005 according to the NHIRD database.
Two-part model
The main objective of this study is to investigate whether individuals with private health insurance have higher probabilities of utilising inpatient services and to examine how the length of stay is affected by those individuals with private health insurance under the NHI programme. There are quite a few models that can be utilised to estimate the demand for medical care—for example, analysis of variance (ANOVA), analysis of covariance (ANOCOVA) and one-part model or two-part model.Footnote 25
Since the decision to receive inpatient services and the duration of a single episode of hospitalisation are not jointly determined, but rather involve independent decision and outcome processes, this paper applies a two-part model. MaddalaFootnote 26 and Duan et al. 25 mentioned that if the decision is sequential, then a two-part or multipart model is appropriate. Such a model is widely implemented in analysing the demand for health insurance and medical utilisation.Footnote 27 It is recommended that a two-part model could be used when facing a skewed distribution, that is where a larger number of those surveyed reported no inpatient service utilisation.25 On the basis of the above descriptions, we take the two-part model to analyse the relationship between private health insurance and inpatient service utilisation under the NHI programme in Taiwan.
Since the likelihood function for the two-part model has a property referred to as separability, the two-part model can be easily estimated using two steps.25 The first equation of the two-part model is a probit model for the dichotomous event of the individual reports having utilised inpatient services or not. We consider that the effect of private health insurance on the demand for health services as well as holding private health insurance is perhaps an endogenous decision and thus the analysis proposes an instrumental variable (IV) approach. A valid instrument must satisfy the following main requirement: it must be highly correlated with the purchase of private health insurance, but unrelated to the utilisation of inpatient services. This study employs two instruments—“holding life insurance” and “holding endowment insurance”—in the IV estimation. However, the Wald test of exogeneity of the IV approach indicates that the test statistics of chi-square is 0.17 (p-value=0.6782). Therefore, we cannot reject the null hypothesis, which implies that holding private health insurance is not considered to be endogenous in our analysis.
Eq. (1) is described as follows:

The dependent variable, INP i , is dichotomous, which indicates whether or not the individual had utilised any acute inpatient services (INP i =1 indicates that the individual had utilised any acute inpatient services; otherwise it is 0). The key independent variable, PH i , indicates whether or not the individual had purchased private health insurance (PH i =1 indicates that the individual had purchased private health insurance; otherwise it is 0).
From the question, “Do you have private health insurance such as whole life or short-term health insurance?” of the 2005 NHIS questionnaire, we construct the PH i variable.Footnote 28 Here, X i consists of several categories of explanatory variables, comprising: (i) personal characteristics and socio-demographic characteristics, including age, age square, gender, marital status, educational attainment and monthly family income; (ii) healthy behaviour factors, including habits of current smoking, drinking and betel nut chewing; (iii) the presence of any chronic diseases, such as heart, lung and liver diseases, cancer, hypertension, diabetes and kidney disease, etc. and (iv) geographic locations, consisting of the northern, central, southern and eastern parts of Taiwan. The β 1 and δ 1 are coefficient estimations in the probit regression.
Since the inpatient length of stay is measured in days that can be counted, instead of using the Poisson model, we take the negative binomial model as the second equation of the two-part model. We adopt the negative binominal model since the count data usually exhibit the feature of over-dispersion. The likelihood-ratio test exhibits the large test statistic of chi-square at 390.58 (p-value=0.001), suggesting that the response variable is over-dispersed and is not sufficiently described by the simpler Poisson distribution, because the Poisson model has to follow the equi-dispersion assumption.
Eq. (2) is described as follows:

The dependent variable is the inpatient length of stay (DAYS) conditional on the individual who reports to have utilised inpatient services. Independent variables of PH i and X i are defined as the same in Eq. (1). Furthermore, we add extra controllers defined as clusters based on ICD-9 procedure codes (inpatients)Footnote 29 and levels of medical institution—medical centre, regional hospital, district hospital and clinics—in Eq. (2). The β 2 and δ 2 are coefficients estimated from the negative binomial regression. In sum, the questions related to inpatient service utilisation, length-of-stay, ICD-9 procedure codes and levels of hospital institutions were obtained from the NHIRD claims database, while purchases of private health insurance and other explanatory variables were included in the 2005 NHIS questionnaire. Appendix Table A1 provides definitions of variables used in this study.
Estimation results
Table 1 presents and displays the descriptive statistics for each of the variables used in this study in terms of the complete sample and two other subgroups, with and without private health insurance. The sample sizes are 12,006, 5,321 and 6,685, respectively.
The proportion of our dependent variable of interviewees who utilised inpatient service is 6.1 per cent for the complete sample, 5.4 per cent for the sample with private health insurance and 6.6 per cent for the sample without health insurance. The proportion of our key independent variable of interviewees who had private health insurance is 44.3 per cent.
Other independent variables that attract attention are those such as age, gender and educational attainments. For example, the average age of the interviewees with private health insurance is 38.37, while it is 46.65 for the interviewees without private health insurance. Males account for 48.2 per cent of the interviewees with private health insurance and 56.5 per cent of the interviewees without private health insurance. The proportion of interviewees with private health insurance who had completed senior high school or had a college degree and above is 76.9 per cent, while it is 50.1 per cent for interviewees without private health insurance.
The average age of all participants is 42.98 years and males account for 52.9 per cent of interviewees. About 63.7 per cent of the interviewees are married, while 5.4 per cent of the interviewees are living alone. A total of 61.9 per cent per cent of the interviewees had completed senior high school or had a college degree and above, and about 43.1 per cent of the interviewees have monthly family income below NT$70,000. Roughly 44 per cent of the sample live in the northern part of Taiwan and 22.5 per cent in the central part of Taiwan. A total of 28.1 per cent of the interviewees are current smokers, 38.7 per cent are current drinkers and 30.8 per cent are betel nut chewers.
With regard to their health status, 34.2 per cent of the interviewees reported that their health is not good, 31.0 per cent reported that their health is moderate and 24.7 per cent reported that their health is very good. The proportions of each chronic disease are less than 5 per cent, except that 10 per cent of the interviewees reported that they have hypertension.
Table 2 presents the descriptive statistics of the interviewees with inpatient service utilisation only. They are displayed in terms of the overall sample and two other subgroups, with and without private health insurance. The sample sizes are 731, 287 and 444, respectively.
The average mean of our dependent variable of the average number of days for acute inpatient services is 6.05 days for the overall sample, 5.15 days for the sample with private health insurance and 6.63 days for the sample without health insurance. The proportion of our key independent variable of interviewees who had private health insurance is 39.3 per cent.
Other independent variables that attract attention are those such as age, gender and educational attainments. For example, the average age of the interviewees with private health insurance is 38.99, while it is 55.64 for the interviewees without private health insurance. Males account for 34.5 per cent of the interviewees with private health insurance and 57 per cent of the interviewees without private health insurance. The proportion of interviewees with private health insurance who had completed senior high school or had a college degree and above is 73.5 per cent, while it is 33.4 per cent for the interviewees without private health insurance.
The sample of interviewees with inpatient service utilisation in Table 2 compared to that of the complete sample in Table 1 consists, in general, of a more elderly population without private health insurance. Moreover, most of the interviewees had educational attainments below junior high school. The proportion of interviewees who reported that their physical health status is very good is small, while the proportion for each chronic disease is large.
Table 3 presents the estimated results of the two-part model. Results of the first part of the estimation indicate that a significantly positive likelihood exists for individuals with private health insurance to utilise inpatient services. Other explanatory variables that significantly affect the likelihood of inpatient service utilisation are those such as age, gender, marital status, monthly family income, regional variables, health status and the individual’s chronic disease status.
Age and gender/male are associated with a significantly negative likelihood of utilising inpatient care services, while being married has a significantly positive effect on the likelihood of utilising inpatient care services. We find the monthly family income levels ranging from NT$50,000 to NT$70,000 and from NT$70,000 to NT$100,000 to have a significantly negative likelihood of utilising inpatient services in contrast to those with monthly income levels below NT$30,000. Individuals located in the northern or central regions are shown to have a significantly negative likelihood of utilising inpatient services as compared to the eastern area of Taiwan.
For the health status, apart from those reporting a “very bad” health condition, there is a negative likelihood of utilising inpatient services for those individuals reporting that their health condition is very good, moderate or not good. Moreover, individuals with chronic diseases such as heart disease, gout, liver disease, cancer and kidney disease show higher probabilities of utilising inpatient services.
In the second part, the results indicate that there exists a significant and positive effect on the inpatient length of stay for individuals with private health insurance. Other explanatory variables that significantly affect the inpatient length of stay are regional variables, health status and the individual’s chronic disease status.
Individuals located in the central or southern region of Taiwan as compared to the eastern region tend to have a short inpatient length of stay. In regards to health status, apart from those reporting a “very bad” health condition, the association between individuals reporting that their health condition is very good, moderate or not good and inpatient length of stay is negative. The results for individuals with chronic diseases such as gout, cancer, mental disorder and diabetes present a positive effect on the inpatient’s length of stay, while liver disease shows the opposite direction result.
Our main focus of this study is to examine whether individuals with private health insurance are associated with higher probabilities of inpatient service utilisation and a longer duration of a single episode of hospitalisation. Table 4 presents the marginal effect of private health insurance on the probability of utilising inpatient services and the incidence-rate ratio of private health insurance on inpatient length of stay. Results indicate that the marginal effects of private health insurance on inpatient service utilisation are 0.9 per cent and the incidence-rate ratio of private health insurance on inpatient length of stay is 1.15.
Discussion
According to statistics from the national health expenditure (NHE) report of the Department of Health, Executive Yuan in Taiwan, NHE per capita was NT$29,351 in 2004, or 1.9 times compared to that before the implementation of NHI in 1994.Footnote 30 At the same time, the purchase rate of households obtaining private health insurance increased to 72.3 per cent in 2004 compared with 63.9 per cent in 1993.4 This indicates that obtaining private health insurance as a supplementary insurance to NHI is an ongoing tendency in Taiwan, because the NHI programme requires users to pay additional fees for specific types of services or drugs. In Taiwan, the NHI programme, which covers 99.5 per cent of the population, provides every citizen with equal access to comprehensive medical services. Therefore, private health insurance in Taiwan is regarded as supplementary insurance to the public health system.
Our empirical results indicate that a moral hazard problem may exist since individuals with private health insurance tend to have a higher probability of utilising inpatient services. Furthermore, there exists a significant and positive effect on the inpatient length of stay for individuals with private health insurance after controlling for social economics status, health status, the level of medical institution and clustering ICD-9 procedure codes under the NHI programme. Issues of moral hazard are important in analysing human behaviour in the insurance market. Specifically, a private health insurance policy in Taiwan is usually designed with a clause in the form of unlimited coverage throughout the whole lifespan.21 Unlimited coverage throughout the whole life means that private health insurance not only induces a moral hazard problem, but also increases the insolvency probability of insurance companies. Thus, a reform of the private health insurance scheme could provide an alternative way to mitigate the moral hazard problem.
Insurance companies in Taiwan have gradually become aware that health insurance with unlimited coverage throughout the whole lifespan could have negative impacts on their business operations in the future.21 Therefore, more insurers have begun to provide an “account-based” health insurance policy in the insurance market,21 which could possibly reduce operational risk and mitigate the moral hazard problem, as the insured now faces the risk of exhausting the amount allowed in the health account. Therefore, an appropriate private health system could possibly allow health resources to be allocated efficiently and fairly.
The financial burden of NHI in Taiwan will inevitably increase in the future, since the rate of ageing in Taiwan is projected to be faster than that of most developed countries.Footnote 31 The way to mitigate the financial deficit of NHI is to increase the co-payment, adjust premiums upwards or limit the public coverage of medical services (additional fees-for-charge) to help ensure that the NHI programme works well. The Taiwan government should reconsider the role that public health insurance plays in the health system. For example, a policy reform plan, which is suggested by Buchmueller and Couffinhal,17 points out that when France’s government faced chronic financial deficits in its public health programme, the government showed a willingness to reform the system by shifting coverage of certain treatments from public to private health insurance. Therefore, the government could also consider reforming the NHI system by limiting the ranges of coverage. Furthermore, one study suggests that the government could enhance public education to improve health knowledge for elderly people because health-care expenditure may be reduced by their better health status and healthier lifestyles.Footnote 32 This policy could also possibly mitigate the financial burden of the NHI system.
There are still some limitations to this study. One limitation is that our data set lacks information regarding different insurance policies. Although we cannot distinguish the types of insurance policies, individuals with whole life or short-term private health insurance can still get reimbursed and have incentives to increase the utilisation of inpatient health service. Second, the quality of care may affect health outcomes and this may also affect the inpatient’s length of stay. Supply-side factors are crucial in analysing the inpatient’s length of stay.Footnote 33 Factors that impact the inpatient’s length of stay include individual characteristics, socio-demographic variables and supply-side factors such as the quality of care. Due to data limitations, we only control for the levels of medical institution in the analysis.
In sum, there are some merits to this paper. The first one is that the variable for the inpatient’s length of stay is obtained from the Taiwan NHIRD. The claims data provides more accurate health service records than those obtained through a questionnaire survey. Furthermore, by using linked claims data from the NHIRD and the NHIS, we are able to examine various personal and socio-demographic variables on the utilisation of inpatient services as well as the role of private health insurance. Second, by controlling for the clusters of the ICD-9 procedure codes, we are able to obtain more critical estimates of the moral hazard phenomenon since each patient with a similar ICD-9 procedure code is located in a clinically meaningful category.
Conclusion
The purpose of this paper is to investigate whether individuals with private health insurance are associated with higher probabilities of inpatient service utilisation and a longer duration of a single episode of hospitalisation under the NHI programme in Taiwan. By utilising nationwide population-based claims data from the NHIRD linked with the NHIS in Taiwan, we apply a two-part model in analysing the effect of private health insurance on inpatient service utilisation under the NHI programme. Our empirical results are consistent with previous studies showing that the moral hazard problem may exist under partial public and/or private health insurance with the co-existence of public and private hospitals.Footnote 34 Specifically, Savage and WrightFootnote 35 found that individuals with private health insurance tend to spend more days in hospital in Australia, while Wong et al. Footnote 36 presented that individuals with private health insurance are more likely to use inpatient services, but it does not impact their length of stay in Hong Kong. Dardanoni and DonniFootnote 37 showed that there is a positive likelihood of individuals with private supplementary insurance, named Medigap, utilising inpatient services in the U.S.
The interaction between public and private health insurance varies across countries depending on the health system.Footnote 38 For example, Australia has a mixed health system where individuals are free to use public health services, but have to pay for utilising private services. Thus, individuals may purchase private health insurance to use private health services.35 The incomplete publicly financed universal coverage in Hong Kong along with a mixed health system of public and private sectors also provides incentives for individuals to purchase private health insurance.36 However, unlike Australia or Hong Kong, the NHI programme in Taiwan provides for all necessary medical treatments and promises equal access to health care for all citizens regardless of whether the hospital is public or private. Therefore, life insurance companies in Taiwan often sell hospitalisation insurance, which may offer incentives for the insured to increase hospital admissions and length of stay so as to obtain more reimbursements. To the best of our knowledge, the literature has yet to research moral hazard issues under the interaction of public and private health insurance in health-care provisions that utilise claims data in Taiwan.
In conclusion, from the policy perspective, the findings of this study provide a good reference for policymakers and insurance companies since financial deficits and unlimited coverage throughout the whole lifespan are primary concerns for Taiwan’s NHI programme and private insurance companies, respectively. Our findings thus may lead to a greater focus on the NHI programme and the policy scheme within private health insurance. Although elevating the importance of private health insurance in the health system may be an alternative choice when the Taiwan government faces the dilemma of a financial deficit under the NHI programme, future research could place greater emphasis on analysing the demand for health services if there are public and private health insurance reforms, because Taiwan’s growing aged population is likely to have significant effects on the demand for inpatient services.
Notes
1 Comprehensive basic medical care includes preventive health, clinical care, hospitalisation, Chinese medicine, pharmaceutical care, home health care, psychiatric care and social rehabilitation.
Feldstein (1973), Link et al. (1980), McCall et al. (1991), Lillard and Rogowski (1995), Hurd and McGarry (1997), Cheng and Chiang (1998), Long et al. (1998), Sapelli and Vial (2003), Savage and Wright (2003), Buchmueller et al. (2004), Wong et al. (2006), Barros et al. (2008), Kang et al. (2009), Dardanoni and Donni (2012).
The ICD-9 is an abbreviation of “International Classification of Diseases 9th edition”. The ICD-9, comprises a six-digit number of codes that are used worldwide to classify diseases and injuries. It is a publication of the World Health Organization.
The cost of inpatient services accounted for around 32.85 per cent of overall medical expenditures in 2010, according to statistics from the Bureau of National Health Insurance in Taiwan.
The health insurance policies usually include operation fees, ambulance fees and a fixed payment scheme per diem. The amount of reimbursements depends on the insured’s policy. For example, for the whole life health insurance, the amount of reimbursements are around NT$1,000–5,000 per day. The insured could pay a higher premium to obtain higher coverage per day. Note that the exchange rate was US$1=NT$32.17 at the time of the survey in 2005.
The health insurance system covers between 70 per cent and 95 per cent of hospitalisation expenses depending on the length of stay and whether the ailment is acute or chronic. The insured will only be responsible for the co-payment of 5–30 per cent of the cost of hospitalisation.
However, we cannot distinguish whether the interviewee has whole life or the short-term insurance, which adds to the limitations of the paper.
Software for clustering ICD-9 procedure codes of patient data into a manageable number of clinically meaningful categories was developed by the Agency for Health care Research and Quality (AHRQ). ICD-9 procedure codes (inpatients) were divided into 231 groups in this case. The classifications of the ICD-9 procedure codes are obtained from the following link: www.hcupus.ahrq.gov/toolssoftware/ccs/AppendixBSinglePR.txt.
References
Annual report of life insurance (2005 and 2010) Insurance Year Book, Taipei, Taiwan: The Life Insurance Association of the Republic of China.
Arrow, K.J. (1963) ‘Uncertainty and the welfare economics of medical care’, American Economic Review 53 (5): 941–973.
Arrow, K.J. (1971) Essays in the Theory of Risk-Bearing, Chicago, IL: Markham Publishing Company.
Arrow, K.J. (1976) ‘Welfare analysis of changes in health coinsurance rates’, in R. Rossett (ed.) The Role of Health Insurance in the Health Service Sector, New York: National Bureau of Economic Research.
Barros, P.P., Machado, M.P. and Galdeano, A.S. (2008) ‘Moral hazard and the demand for health services: A matching estimator approach’, Journal of Health Economics 27 (4): 1006–1025.
Buchmueller, T.C. and Couffinhal, A. (2004) Private health insurance in France, OECD Health Working Papers, No. 12(3).
Buchmueller, T.C., Couffinhal, A., Grignon, M. and Perronnin, M. (2004) ‘Access to physician services: does supplemental insurance matter? Evidence from France’, Health Economics 13 (7): 669–687.
Bureau of National Health Insurance (1990) National Health Insurance Program Planning Report, Taipei, Taiwan: Bureau of National Health Insurance, Department of Health, Executive Yuan, Republic of China.
Bureau of National Health Insurance (2006) ‘Taipei, Taiwan’, from http://www.nhi.gov.tw/webdata/webdata.aspx?menu=6&menu_id=168&WD_ID=&webdata_id=1803, accessed 28 January 2012.
Bureau of National Health Insurance (2010) The National Health Insurance Statistics, Taipei, Taiwan: Bureau of National Health Insurance, Department of Health, Executive Yuan, Republic of China.
Cairns, J.A. and Munro, J. (1992) ‘Why does length of stay vary for orthopaedic surgery?’, Health Policy 22 (3): 297–306.
Cameron, A.C., Trivedi, P.K., Milne, F. and Piggot, J. (1988) ‘A microeconometric model of the demand for health care and health insurance in Australia’, Review of Economic Studies 55 (1): 85–106.
Chen, L.W., Yip, W., Chang, M.C., Lin, H.S., Lee, S.D., Chiu, Y.L. and Lin, Y.H. (2007) ‘The effect of Taiwan’s National Health Insurance on access and health status of the elderly’, Health Economics 16 (3): 223–242.
Cheng, S.H. and Chiang, T.L. (1998) ‘Disparity of medical care utilization among different health insurance scheme in Taiwan’, Social Science of Medicine 47 (5): 613–620.
Dardanoni, V. and Donni, P.L. (2012) ‘Incentive and selection effects of Medigap insurance on inpatient care’, Journal of Health Economics 31 (3): 457–470.
Department of Health (2010) ‘Executive Yuan Taiwan National Health Expenditure’, from http://www.doh.gov.tw/CHT2006/DM/DM2_2.aspx?now_fod_list_no=12040&class_no=440&level_no=2, accessed 28 January 2012.
Duan, N., Manning, W.G., Morris, C.N. and Newhouse, J.P. (1983) ‘A comparison of alternative models for the demand for medical care’, Journal of Business and Economic Statistics 2 (1): 283–289.
Epstein, A.M., Stern, R.S. and Weissman, J.S. (1990) ‘Do the poor cost more? A multihospital study patients’ socioeconomic status and use of hospital resources’, New England Journal of Medicine 322 (16): 1122–1128.
Feldstein, M. (1973) ‘The welfare loss of excess health insurance’, Journal of Political Economics 81 (2): 251–280.
Feldstein, M. and Friedman, B. (1977) ‘Tax subsidies, the rational demand for health insurance, and the health care crisis’, Journal of Public Economics 7 (2): 155–178.
Goldfarb, M.G., Hornbrook, M.C. and Higgins, C.S. (1983) ‘Determinants of hospital use: A cross-diagnostic analysis’, Medical Care 21 (1): 48–66.
Hurd, M.D. and McGarry, K. (1997) ‘Medical insurance and the use of health care services by the elderly’, Journal of Health Economics 16 (2): 129–154.
Kang, S., You, C.H., Kwon, Y.D. and Oh, E.H. (2009) ‘Effects of supplementary private health insurance on physician visits in Korea’, Journal of Formos Medicine Association 108 (12): 912–920.
Koc, C. (2011) ‘Disease-specific moral hazard and optimal health insurance design for physician services’, Journal of Rick and Insurance 78 (2): 413–446.
Lee, C.H., Huang, N., Chang, H.J, Hsu, Y.J., Wang, M. and Chou, Y. (2005) ‘The immediate effects of the severe acute respiratory syndrome (SARS) epidemic on childbirth in Taiwan’, BMC Public Health 5 (30): 30–36.
Life Insurance Association (1999) Annual Report of Life Insurance, Republic of China, Taipei, Taiwan: Life Insurance Association, Republic of China.
Lillard, L.A. and Rogowski, J. (1995) Does supplemental private insurance increase Medicare costs? Rand Corporation Working Paper, presented at the 1995 NBER Summer Institute, Cambridge, MA.
Link, C.R., Long, S.H. and Seltle, R.F. (1980) ‘Cost sharing, supplementary insurance, and health services utilization among the Medicare elderly’, Health Care Financing Review 2 (2): 25–31.
Liu, L.F. and Wen, M.J. (2010) ‘A longitudinal evaluation of residents’ health outcomes in nursing homes and residential care homes in Taiwan’, Quality of Life Research 19 (7): 1007–1018.
Liu, T.C. and Chen, C.S. (2002) ‘An analysis of private health insurance purchasing decisions with national health insurance in Taiwan’, Social Science and Medicine 55 (5): 755–774.
Long, S.H., Marquis, M.S. and Rodgers, J. (1998) ‘Do people shift their use of health services over time to take advantages of insurance?’, Journal of Health Economics 17 (1): 105–115.
Maddala, G. (1985) ‘A survey of the literature on selectivity bias as it pertains to health care markets’, in Scheffler, R.M. and Rossiter, L.F. (eds) Advances in Health Economics and Health Services Research, Vol. 6, Greenwich (Conn.), JAI Press, pp. 3–18.
Mangyo, E. (2004) Measuring the impact of health insurance on elderly physician visit: A natural experiment in Taiwan, working paper, University of Michigan.
Manning, W.G. and Marquis, M.S. (1996) ‘Health insurance: The trade-off between risk pooling and moral hazard’, Journal of Health Economics 15 (5): 609–639.
Manning, W.G., Newhouse, J.P., Duan, N., Keeler, E.B., Leibowitz, A. and Marquis, M.S. (1987) ‘Health insurance and the demand for Medical Care: Evidence from a randomized experiment’, The American Economic Review 77 (3): 251–277.
Martin, S. and Smith, P. (1996) ‘Explaining variations in inpatient length of stay in the national health service’, Journal of Health Economics 15 (3): 279–304.
McCall, N., Rice, T., Boismier, J. and West, R. (1991) ‘Private health insurance and medical care utilization: Evidence from the Medicare population’, Inquiry 28 (3): 276–287.
Newhouse, J.P. and the Insurance Experiment Group (1993) Free for All? Lessons from the RAND Health Insurance Experiment, Cambridge, MA: Harvard University Press.
OECD (2004) Private health insurance in OECD countries, OECD Policy Brief.
Pauly, M.V. (1986) ‘Taxation, health insurance, and market failure’, Journal of Economic Literature 24 (2): 629–675.
Sapelli, C. and Vial, B. (2003) ‘Self-selection and moral hazard in Chilean health insurance’, Journal of Health Economics 22 (3): 459–476.
Savage, E. and Wright, D.J. (2003) ‘Moral hazard and adverse selection in Australian private hospitals: 1989–1990’, Journal of Health Economics 22 (3): 331–359.
Shiu, Y.M. and Chiu, M.C. (2008) ‘Re-estimating the demographic impact on health care expenditure: Evidence from Taiwan’, The Geneva Papers on Risk and Insurance—Issues and Practice 33 (4): 728–743.
Tien, J.J. (2010) ‘The study on evaluating risk of commercial medical expense insurance policies for life insurance industry in Taiwan’, Journal of Risk Management 12 (3): 273–299 [in Chinese].
Wong, I.L., Chan, W.S., Choi, S., Lo, S.V. and Leung, G.M. (2006) ‘Moral hazard or realized access to care? Empirical observations in Hong Kong’, Health Policy 75 (3): 251–261.
Zeckhauser, R.J. (1970) ‘Medical insurance: A case study of the trade-off between risk spreading and appropriate incentives’, Journal of Economic Theory 2 (1): 10–26.
Acknowledgements
The authors thank the 2005 National Health Interview Survey Original Database provided by the Bureau of Health Promotion, Department of Health, Executive Yuan and National Health Research Institutes, Taiwan.
Author information
Authors and Affiliations
Appendix
Rights and permissions
About this article
Cite this article
Tian, WH., Tien, J., Chen, CS. et al. Private Health Insurance and Inpatient Service Utilisation among Adults and Elderly People under Taiwan’s National Insurance Programme. Geneva Pap Risk Insur Issues Pract 37, 655–677 (2012). https://doi.org/10.1057/gpp.2012.36
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1057/gpp.2012.36