Abstract
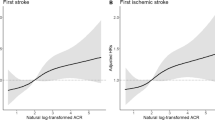
We aimed to investigate the association between neutrophil counts and first stroke and examine possible effect modifiers among treated hypertensive adults. This is a post hoc analysis of the China Stroke Primary Prevention Trial (CSPPT). A total of 11,878 hypertensive adults with data on neutrophil counts at baseline were included in the current study. The primary outcome was first stroke. During a median follow-up of 4.5 years, 414 (3.5%) participants experienced a first stroke, including 358 with ischemic stroke, 55 with hemorrhagic stroke and one with uncertain type of stroke. Compared with participants in quartile 1 (<2.9 × 109/L) of neutrophil counts, those in the upper quartiles (quartile 2–4 [≥2.9 × 109/L]) had a significantly higher risk of first stroke (HR, 1.35; 95% CI: 1.02, 1.78) or first ischemic stroke (HR, 1.38; 95% CI: 1.02, 1.86). Moreover, a strong positive association between neutrophil counts and first ischemic stroke was found in participants with total homocysteine (tHcy) levels <15 μmol/L (HR, 1.74; 95% CI: 1.17, 2.58; vs. ≥15 μmol/L; HR, 0.91; 95% CI: 0.57, 1.46, P interaction = 0.042) at baseline or time-averaged mean arterial pressure (MAP) ≥102 mmHg (median) (HR, 1.92; 95% CI: 1.27, 2.89; vs. <102 mmHg; HR, 0.89; 95% CI: 0.57, 1.41, P interaction = 0.015) during the treatment period. However, no such association between neutrophil counts and first hemorrhagic stroke was found. In summary, high baseline neutrophil counts were associated with an increased risk of first ischemic stroke among hypertensive patients, especially in those with low tHcy at baseline or high time-averaged MAP during the treatment period.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The data and study materials that support the findings will be available from the corresponding authors upon request after a request is submitted, formally reviewed, and approved by the Ethics Committee of the Institute of Biomedicine, Anhui Medical University.
References
Johnson CO, Nguyen LH, Nguyen M, Nguyen CT, Roth GA, Nichols E, et al. Global, regional, and national burden of stroke, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18:439–58.
O’Donnell MJ, Chin SL, Rangarajan S, Xavier D, Liu L, Zhang H, et al. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): a case-control study. Lancet. 2016;388:761–75.
Soehnlein O, Steffens S, Hidalgo A, Weber C. Neutrophils as protagonists and targets in chronic inflammation. Nat Rev Immunol. 2017;17:248–61.
Soehnlein O. Multiple roles for neutrophils in atherosclerosis. Circ Res. 2012;110:875–88.
Jickling GC, Liu D, Ander BP, Stamova B, Zhan X, Sharp FR. Targeting neutrophils in ischemic stroke: translational insights from experimental studies. J Cereb Blood Flow Metab. 2015;35:888–901.
Noubouossie DF, Reeves BN, Strahl BD, Key NS. Neutrophils: back in the thrombosis spotlight. Blood. 2019;133:2186–97.
Shah AD, Denaxas S, Nicholas O, Hingorani AD, Hemingway H. Neutrophil counts and initial presentation of 12 cardiovascular diseases: a CALIBER Cohort Study. J Am Coll Cardiol. 2017;69:1160–9.
Huh JY, Ross GW, Chen R, Abbott RD, Bell C, Willcox B, et al. Total and differential white blood cell counts in late life predict 8-year incident stroke: the Honolulu Heart Program. J Am Geriatr Soc. 2015;63:439–46.
Wu TH, Chien KL, Lin HJ, Hsu HC, Su TC, Chen MF, et al. Total white blood cell count or neutrophil count predict ischemic stroke events among adult Taiwanese: report from a community-based cohort study. BMC Neurol. 2013;13:7.
Zia E, Melander O, Bjorkbacka H, Hedblad B, Engstrom G. Total and differential leucocyte counts in relation to incidence of stroke subtypes and mortality: a prospective cohort study. J Intern Med. 2012;272:298–304.
Grau AJ, Boddy AW, Dukovic DA, Buggle F, Lichy C, Brandt T, et al. Leukocyte count as an independent predictor of recurrent ischemic events. Stroke. 2004;35:1147–52.
Zhu B, Pan Y, Jing J, Meng X, Zhao X, Liu L, et al. Neutrophil counts, neutrophil ratio, and new stroke in minor ischemic stroke or TIA. Neurology. 2018;90:e1870–8.
Li Y, Zhou H, Liu M, Liang M, Wang G, Wang B, et al. Association of visit-to-visit variability in blood pressure and first stroke risk in hypertensive patients with chronic kidney disease. J Hypertens. 2020;38:610–7.
Li Y, Yang L, Wang L, Zhang M, Huang Z, Deng Q, et al. Burden of hypertension in China: a nationally representative survey of 174,621 adults. Int J Cardiol. 2017;227:516–23.
Jhuang Y, Kao T, Peng T, Chen W, Li Y, Chang P, et al. Neutrophil to lymphocyte ratio as predictor for incident hypertension: a 9-year cohort study in Taiwan. Hypertens Res. 2019;42:1209–14.
Huo Y, Li J, Qin X, Huang Y, Wang X, Gottesman RF, et al. Efficacy of folic acid therapy in primary prevention of stroke among adults with hypertension in China. JAMA. 2015;313:1325–35.
Qin X, Li Y, He M, Tang G, Yin D, Liang M, et al. Folic acid therapy reduces serum uric acid in hypertensive patients: a substudy of the China Stroke Primary Prevention Trial (CSPPT). Am J Clin Nutr. 2017;105:882–9.
Qin X, Shen L, Zhang R, Li Y, Wang X, Wang B, et al. Effect of folic acid supplementation on cancer risk among adults with hypertension in China: a randomized clinical trial. Int J Cancer 2017;141:837–47.
Sesso HD, Stampfer MJ, Rosner B, Hennekens CH, Gaziano JM, Manson JE, et al. Systolic and diastolic blood pressure, pulse pressure, and mean arterial pressure as predictors of cardiovascular disease risk in men. Hypertension. 2000;36:801–7.
Lim EM, Cembrowski G, Cembrowski M, Clarke G, Race-specific WBC. and neutrophil count reference intervals. Int J Lab Hematol. 2010;32:590–7.
Sørensen OE, Borregaard N. Neutrophil extracellular traps—the dark side of neutrophils. J Clin Investig. 2016;126:1612–20.
Wantha S, Alard JE, Megens RT, van der Does AM, Doring Y, Drechsler M, et al. Neutrophil-derived cathelicidin promotes adhesion of classical monocytes. Circ Res. 2013;112:792–801.
Gaul DS, Stein S, Matter CM. Neutrophils in cardiovascular disease. Eur Heart J. 2017;38:1702–4.
Meegan JE, Yang X, Coleman DC, Jannaway M, Yuan SY. Neutrophil-mediated vascular barrier injury: Role of neutrophil extracellular traps. Microcirculation. 2017;24:e12352.
Hoyer FF, Nahrendorf M. Neutrophil contributions to ischaemic heart disease. Eur Heart J. 2017;38:465–72.
Döring Y, Soehnlein O, Weber C. Neutrophil extracellular traps in atherosclerosis and atherothrombosis. Circulation Res. 2017;120:736–43.
Laridan E, Denorme F, Desender L, Francois O, Andersson T, Deckmyn H, et al. Neutrophil extracellular traps in ischemic stroke thrombi. Ann Neurol. 2017;82:223–32.
Zhao M, Wu G, Li Y, Wang X, Hou FF, Xu X, et al. Meta-analysis of folic acid efficacy trials in stroke prevention: Insight into effect modifiers. Neurology. 2017;88:1830–8.
Wald D, Law M, Morris JK. Homocysteine and cardiovascular disease: evidence on causality from a metaanalysis. BMJ. 2002;325:1202.
Leng YP, Ma YS, Li XG, Chen RF, Zeng PY, Li XH, et al. l-Homocysteine-induced cathepsin V mediates the vascular endothelial inflammation in hyperhomocysteinaemia. Br J Pharm. 2018;175:1157–72.
Dudman NP, Temple SE, Guo XW, Fu W, Perry MA. Homocysteine enhances neutrophil-endothelial interactions in both cultured human cells and rats in vivo. Circ Res. 1999;84:409–16.
Zheng L, Sun Z, Li J, Zhang R, Zhang X, Liu S, et al. Pulse pressure and mean arterial pressure in relation to ischemic. Stroke Patients Uncontrolled Hypertension Rural Areas China Stroke. 2008;39:1932–7.
Fuhrer H, Weiller C, Niesen WD. Is mean arterial pressure the best parameter in ischemic stroke? Clin Case Rep. 2016;4:236–9.
Miura K, Nakagawa H, Ohashi Y, Harada A, Taguri M, Kushiro T, et al. Four blood pressure indexes and the risk of stroke and myocardial infarction in Japanese men and women: a meta-analysis of 16 cohort studies. Circulation. 2009;119:1892–8.
Wang Z, Chen Z, Zhang L, Wang X, Hao G, Zhang Z, et al. Status of hypertension in China: results from the China Hypertension Survey, 2012–2015. Circulation. 2018;137:2344–56.
Qin X, Li Y, Sun N, Wang H, Zhang Y, Wang J, et al. Elevated homocysteine concentrations decrease the antihypertensive effect of angiotensin-converting enzyme inhibitors in hypertensive patients. Arterioscler Thromb Vasc Bio. 2017;37:166–72.
Danesh J, Wheeler JG, Hirschfield GM, Eda S, Eiriksdottir G, Rumley A, et al. C-reactive protein and other circulating markers of inflammation in the prediction of coronary heart disease. N. Engl J Med. 2004;350:1387–97.
Funding
The study was supported by the National Natural Science Foundation of China [81973133, 81730019]; the National Key Research and Development Program [2016YFE0205400, 2018ZX09739010, 2018ZX09301034003]; the Science and Technology Planning Project of Guangzhou, China [201707020010]; the Science, Technology and Innovation Committee of Shenzhen [JSGG20170412155639040, GJHS20170314114526143, JSGG20180703155802047]; the Economic, Trade and Information Commission of Shenzhen Municipality [20170505161556110, 20170505160926390]; and the Clinical Innovation Research Program of Guangzhou Regenerative Medicine and Health Guangdong Laboratory [2018GZR0201003].
Author information
Authors and Affiliations
Contributions
XQ, XX, and ZZ contributed to the conception or design of the work. XQ, ZZ, HL, and CL contributed to the acquisition, analysis, or interpretation of data for the work. XQ, ZZ, and YZ drafted the manuscript. All critically revised the manuscript, gave final approval, and agreed to be accountable for all aspects of work ensuring integrity and accuracy.
Corresponding authors
Ethics declarations
Conflict of interest
XX reports grants from the National Key Research and Development Program [2016YFE0205400, 2018ZX09739010, 2018ZX09301034003], the Science and Technology Planning Project of Guangzhou, China [201707020010], the Science, Technology and Innovation Committee of Shenzhen [JSGG20170412155639040, GJHS20170314114526143, JSGG20180703155802047], and the Economic, Trade and Information Commission of Shenzhen Municipality [20170505161556110, 20170505160926390]. XQ reports grants from the National Natural Science Foundation of China [81973133, 81730019]. No other disclosures were reported.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Zhang, Z., Zhou, C., Liu, M. et al. Neutrophil counts and the risk of first stroke in general hypertensive adults. Hypertens Res 44, 830–839 (2021). https://doi.org/10.1038/s41440-021-00625-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-021-00625-1
Keywords
This article is cited by
-
Influencing factors on morbidity and mortality in intertrochanteric fractures
Scientific Reports (2023)