Abstract
Background
Simulation is becoming a more common modality in medical education. The data regarding effectiveness of simulation in critical care neurology education are limited.
Methods
We administered a three-scenario simulation course to critical care fellowship trainees at a large academic medical center as a part of their core curriculum requirement. Pre- and posttests assessing medical knowledge and trainee confidence in managing neurologic disease were completed by all trainees. Overall satisfaction and effectiveness were evaluated following the course. Change in trainee knowledge and confidence before and after the course was assessed for improvement.
Results
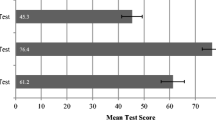
Sixteen trainees completed the simulation course. Prior to completion, medical knowledge was 5.2 ± 0.9 (of 8 possible correct answers) and following the course was 6.4 ± 1.3 (p = 0.002). Overall confidence improved from 15.4 ± 4.9 (of 30 possible points) to 20.7 ± 3.3 (p = <0.0001). Confidence was significantly improved for neurologic diseases directly assessed during the course (p = <0.0001) as well as for those not directly assessed (p = 0.004).
Conclusions
Simulation is an effective means of neurologic education for critical care trainees, with improvement in both medical knowledge and trainee confidence after completion of a three-scenario simulation experience. This course ensures the exposure of critical care trainees to neurologic diseases that are required curricular milestones to successfully complete the fellowship training program.

Similar content being viewed by others
References
Institute of Medicine (US) Committee on Quality of Health Care in America. In: Kohn LT, Corrigan JM, Donaldson MS, editors. To Err is Human: Building a Safer Health System. Washington, DC: National Academies Press; 2000.
Dagnone JD, McGraw R, Howes D, et al. How we developed a comprehensive resuscitation-based simulation curriculum in emergency medicine. Med Teach. 2014;38:1–6.
Laack TA, Dong Y, Goyal DG, Sadosty AT, Suri HS, Dunn WF. Short-term and long-term impact of the central line workshop on resident clinical performance during simulated central line placement. Simul Healthc. 2014;9:228–33.
Miyasaka KW, Martin ND, Pascual JL, Buchholz J, Aggarwal R. A Simulation curriculum for management of trauma and surgical critical care patients. J Surg Educ. 2015;72:803–10.
Murray DJ. Progress in simulation education: developing an anesthesia curriculum. Curr Opin Anaesthesiol. 2014;27:610–5.
Hocker S, Schumacher D, Mandrekar J, Wijdicks EF. Testing confounders in brain death determination: a new simulation model. Neurocrit Care. 2015;23:401–8.
Hocker S, Wijdicks EF, Feske SK, Drislane FW. Use of simulation in acute neurology training: point and counterpoint. Ann Neurol. 2015;78:337–42.
MacDougall BJ, Robinson JD, Kappus L, Sudikoff SN, Greer DM. Simulation-based training in brain death determination. Neurocrit Care. 2014;21:383–91.
Fessler HE, Addrizzo-Harris D, Beck JM, et al. Entrustable professional activities and curricular milestones for fellowship training in pulmonary and critical care medicine: executive summary from the Multi-Society Working Group. Crit Care Med. 2014;42:2290–1.
Wijdicks EF, Varelas PN, Gronseth GS, Greer DM. Evidence-based guideline update: determining brain death in adults: report of the quality standards subcommittee of the American Academy of Neurology. Neurology. 2010;74:1911–8.
Maramattom BV, Wijdicks EF. Acute neuromuscular weakness in the intensive care unit. Crit Care Med. 2006;34:2835–41.
Fugate JE, Rabinstein AA. Update on intravenous recombinant tissue plasminogen activator for acute ischemic stroke. Mayo Clin Proc. 2014;89:960–72.
Rabinstein AA, Lanzino G, Wijdicks EF. Multidisciplinary management and emerging therapeutic strategies in aneurysmal subarachnoid haemorrhage. Lancet Neurol. 2010;9:504–19.
Hocker SE. Status Epilepticus. Continuum (Minneap Minn). 2015;21:1362–83.
Acknowledgments
The authors would like to thank Jay Mandrekar for assistance in statistical analysis of the data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Braksick, S.A., Kashani, K. & Hocker, S. Neurology Education for Critical Care Fellows Using High-Fidelity Simulation. Neurocrit Care 26, 96–102 (2017). https://doi.org/10.1007/s12028-016-0293-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-016-0293-3