Abstract
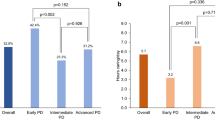
Caring for a family member with dysphagia can negatively impact caregiver wellbeing, although little is known about how dysphagia severity or specific symptoms influence this. The purpose of this study was to examine how objective measures of dysphagia in people with Parkinson’s disease influenced their caregivers’ quality of life. Fifty caregivers (mainly spouses) of people with Parkinson’s disease completed a caregiver quality of life survey. Results were compared to medical chart reviews, interviews, and instrumental evaluations of swallowing from the care recipients. Outcomes included caregiver quality of life score, ratings of airway invasion and pharyngeal residue, and Parkinson’s disease duration. Descriptive and regression analyses were completed. All caregivers reported reduced quality of life, with 28% having severely disturbed adaptation. Every care recipient with Parkinson’s disease demonstrated airway invasion and/or pharyngeal residue. Together, the combination of older care recipient age and longer disease duration was associated with poorer caregiver quality of life [adj. R2 = 0.10–0.12, p = 0.03–0.4]. Neither airway invasion nor pharyngeal residue was related to caregiver quality of life (p > 0.05). Findings confirmed that caregivers of people with Parkinson’s disease and dysphagia experience reduced quality of life; however, current methods of assessing caregivers’ quality of life may not adequately account for dysphagia-specific burden. Results highlight the urgent need for the development of dysphagia-specific assessments of caregivers’ quality of life to facilitate identification of high-risk caregivers and aid the development of support systems to improve health outcomes for caregivers and care recipients.



Similar content being viewed by others
References
National Alliance for Caregiving, AARP Public Policy Institute. Caregivers of older adults: a focused look at those caring for someone age 50+. National Alliance for Caregiving, AARP Public Policy Institute; 2015.
Elkan R, Kendrick D, Dewey M, et al. Effectiveness of home based support for older people: systematic review and meta-analysis. Br Med J. 2001;323(7315):719.
Gardner P. Natural neighborhood networks—important social networks in the lives of older adults aging in place. J Aging Stud. 2011;25(3):263–71.
Sabia J. There’s no place like home: a hazard model analysis of aging in place among older homeowners in the PSID. Res Aging. 2008;30(1):3–35.
Wiles J, Leibing A, Guberman N, Reeve J, Allen R. The meaning of “aging in place” to older people. Gerontologist. 2012;52(3):357–66.
Namasivayam-MacDonald AM, Shune SE. The influence of swallowing impairments as an independent risk factor for burden among caregivers of aging parents: a cross-sectional study. Geriatr Nurs (Minneap). 2020;41(2):81–8. https://doi.org/10.1016/j.gerinurse.2019.06.008.
World Health Organization Quality of Life (WHOQOL); 2012. https://www.who.int/tools/whoqol. Accessed 1 Sept 2020.
Goldsworthy B, Knowles S. Caregiving for Parkinson’s disease patients: an exploration of a stress-appraisal model for quality of life and burden. J Gerontol B. 2008;63(6):372–6. https://doi.org/10.1093/geronb/63.6.P372.
Chappell NL, Colin RR. Burden and well-being among caregivers: examining the distinction. Gerontologist. 2002;42(6):772–80. https://doi.org/10.1093/geront/42.6.772.
Lazarus RS, Folkman S. Stress, appraisal, and coping. New York: Springer; 1984.
Pearlin LI, Mullan JT, Semple SJ, Skaff MM. Caregiving and the stress process: an overview of concepts and their measures. Gerontologist. 1990;30(5):583–94. https://doi.org/10.1093/geront/30.5.583.
Aneshensel C, Pearlin LI, Mullan J, Zarit S, Whitlatch C. Profiles in caregiving: the unexpected carer. New York: Academic; 1995.
Pearlin LI, Skaff MM. Stressors in adaptation in late life. In: Gatz EM, editor. Emerging issues in mental health and aging. Washington, DC: APA Press; 1995.
Pearlin LI, Turner HA, Semple SJ. Coping and the mediation of caregiver stress. In: Light E, Lebowitz B, editors. Alzheimer’s disease treatment and family stress: directions for research. Washington, DC: US Government Printing Office; 1989. p. 198–217.
Martinez-Martin P, Rodriguez-Blazquez C, Forjaz MJ. Quality of life and burden in caregivers for patients with Parkinson’s disease: concepts, assessment and related factors. Expert Rev Pharmacoecon Outcomes Res. 2012;12(2):221–30. https://doi.org/10.1586/erp.11.106.
Greenwell K, Gray WK, van Wersch A, van Schaik P, Walker R. Predictors of the psychosocial impact of being a carer of people living with Parkinson’s disease: a systematic review. Parkinsonism Relat Disord. 2015;21:1–11. https://doi.org/10.1016/j.parkreldis.2014.10.013.
Schrag A, Hovris A, Morley D, Quinn N, Jahanshahi M. Caregiver-burden in Parkinson’s disease is closely associated with psychiatric symptoms, falls, and disability. Parkinsonism Relat Disord. 2006;12:35–41. https://doi.org/10.1016/j.parkreldis.2005.06.011.
Volonté MA, Porta M, Comi G. Clinical assessment of dysphagia in early phases of Parkinson’s disease. Neurol Sci. 2002;23:S121–2. https://doi.org/10.1007/s100720200099.
Leopold NA, Kagel MC. Prepharyngeal dysphagia in Parkinson’s disease. Dysphagia. 1996;11(1):14–22. https://doi.org/10.1007/BF00385794.
Suttrup I, Warnecke T. Dysphagia in Parkinson’s disease. Dysphagia. 2016;31(1):24–32. https://doi.org/10.1007/s00455-015-9671-9.
Jones CA, Ciucci MR. Multimodal swallowing evaluation with high-resolution manometry reveals subtle swallowing changes in early and mid-stage Parkinson disease. J Parkinsons Dis. 2016;6(1):197–208. https://doi.org/10.3233/JPD-150687.
Hunter PC, Crameri J, Austin S, Woodward MC, Hughes AJ. Response of Parkinsonian swallowing dysfunction to dopaminergic stimulation. J Neurol Neurosurg Psychiatry. 1997;63(5):579–83. https://doi.org/10.1136/jnnp.63.5.579.
Mamolar Andrés S, Santamarina Rabanal M, Granda Membriela C, Fernández Gutiérrez M, Sirgo Rodríguez P, Álvarez MC. Swallowing disorders in Parkinson’s disease. Acta Otorinolaryngol Esp. 2017;68:15–22. https://doi.org/10.1016/j.otoeng.2017.01.003.
Chou KL, Evatt M, Hinson V, Kompoliti K. Sialorrhea in Parkinson’s disease: a review. Mov Disord. 2007;22(16):2306–13. https://doi.org/10.1002/mds.21646.
Rodrigues B, Nóbrega AC, Sampaio M, Argolo N, Melo A. Silent saliva aspiration in Parkinson’s disease. Mov Disord. 2010;26(1):138–41. https://doi.org/10.1002/mds.23301.
Hegland KW, Okun MS, Troche MS. Sequential voluntary cough and aspiration or aspiration risk in Parkinson’s disease. Lung. 2014;192(4):601–8. https://doi.org/10.1007/s00408-014-9584-7.
Miller N, Noble E, Jones D, Burn D. Hard to swallow: dysphagia in Parkinson’s disease. Age Ageing. 2006;35(6):614–8. https://doi.org/10.1093/ageing/afl105.
Trail M, Nelson ND, Van JN, Appel SH, Lai EC. Major stressors facing patients with amyotrophic lateral sclerosis (ALS): a survey to identify their concerns and to compare with those of their caregivers. Amyotroph Lateral Scler Other Mot Neuron Disord. 2004;5(1):40–5. https://doi.org/10.1080/14660820310016075.
Diehl-Schmid J, Schmidt EM, Nunnemann S, et al. Caregiver burden and needs in frontotemporal dementia. J Geriatr Psychiatry Neurol. 2013;26(4):221–9. https://doi.org/10.1177/0891988713498467.
Choi-Kwon S, Kim HS, Kwon SU, Kim JS. Factors affecting the burden on caregivers of stroke survivors in South Korea. Arch Phys Med Rehabil. 2005;86(5):1043–8. https://doi.org/10.1016/j.apmr.2004.09.013.
Nund RL, Ward EC, Scarinci NA, Cartmill B, Kuipers P, Porceddu SV. Carers’ experiences of dysphagia in people treated for head and neck cancer: a qualitative study. Dysphagia. 2014;29(4):450–8. https://doi.org/10.1007/s00455-014-9527-8.
Penner JL, McClement S, Lobchuk M, Daeninck P. Family members’ experiences caring for patients with advanced head and neck cancer receiving tube feeding: a descriptive phenomenological study. J Pain Symptom Manag. 2012;44(4):563–71. https://doi.org/10.1016/j.jpainsymman.2011.10.016.
Shune SE, Namasivayam-MacDonald AM. Swallowing impairments increase emotional burden in spousal caregivers of older adults. J Appl Gerontol. 2020;39(2):172–80. https://doi.org/10.1177/0733464818821787.
Qutubuddin A, Baron MS. Caregiver distress in Parkinsonism. J Rehabil Res Dev. 2006;43(4–7):499.
Glozman JM. Quality of life of caregivers. Neuropsychol Rev. 2004;14(4):183–96. https://doi.org/10.1007/s11065-004-8158-5.
Curtis J, Perry SE, Troche MS. Detection of airway invasion during flexible endoscopic evaluations of swallowing: comparing barium, blue dye, and green dye. Am J Speech–Lang Pathol. 2019;28(May):1–6. https://doi.org/10.1044/2018_AJSLP-18-0119.
Cichero JAY, Lam P, Steele CM, et al. Development of international terminology and definitions for texture-modified foods and thickened fluids used in dysphagia management: the IDDSI Framework. Dysphagia. 2017;32(2):293–314. https://doi.org/10.1007/s00455-016-9758-y.
Glozman JM, Bicheva KG, Fedorova NV. Scale of quality of life of care-givers (SQLC). J Neurol Suppl. 1998;245(1):39–41. https://doi.org/10.1007/pl00007738.
Harris P, Taylor R, Thielke R, Payne J, Gonzalez N, Conde J. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81.
Harris P, Taylor R, Minor B, et al. The REDCap consortium: building an international community of software partners. J Biomed Inform. 2019;95:103208.
Pisegna JM, Kaneoka A, Coster WJ, Leonard R, Langmore SE. Residue ratings on FEES: trends for clinical application of residue measurement. Dysphagia. 2020. https://doi.org/10.1007/s00455-019-10089-8.
Rosenbek JC, Robbins J, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996;11:93–8.
Schrag A, Quinn N. Dyskinesias and motor fluctuations in Parkinson’s disease: a community-based study. Brain. 2000;123(11):2297–305. https://doi.org/10.1093/brain/123.11.2297.
Tessitore A, Marano P, Modugno N, et al. Caregiver burden and its related factors in advanced Parkinson’s disease: data from the PREDICT study. J Neurol. 2018;265(5):1124–37. https://doi.org/10.1007/s00415-018-8816-9.
Martinez-Martin P, Benito-Leon J, Alonso F, et al. Quality of life of caregivers in Parkinson’s disease. Qual Life Res. 2005;14(2):463–72.
Shune SE, Namasivayam-MacDonald AM. Caregiver burden in dysphagia: moving beyond the physiological impairment. In: American Speech-Language-Hearing Association Convention, Orlando, FL, 2019.
Kalf JG, de Swart BJM, Bloem BR, Munneke M. Prevalence of oropharyngeal dysphagia in Parkinson’s disease: a meta-analysis. Parkinsonism Relat Disord. 2012;18(4):311–5. https://doi.org/10.1016/j.parkreldis.2011.11.006.
Troche MS, Brandimore AE, Okun MS, Davenport PW, Hegland K. Decreased cough sensitivity and aspiration in Parkinson Disease. Chest. 2014;146(5):1294–9. https://doi.org/10.1378/chest.14-0066.
Ebihara S, Saito H, Kanda A, et al. Impaired efficacy of cough in patients with Parkinson disease. Chest. 2003;124(3):1009–15. https://doi.org/10.1378/chest.124.3.1009.
Miller N, Allcock L, Hildreth A, Jones D, Noble E, Burn D. Swallowing problems in Parkinson disease: frequency and clinical correlates. J Neurol Neurosurg Psychiatry. 2009;80:1047–9.
Baronet AM. The impact of family relations on caregivers’ positive and negative appraisal of their caretaking activities. Fam Relat. 2003;52(2):137–42. https://doi.org/10.1111/j.1741-3729.2003.00137.x.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors confirm that they have no relevant conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Perry, S.E., Borders, J.C., Dakin, A.E. et al. Characterizing Quality of Life in Caregivers of People with Parkinson’s Disease and Dysphagia. Dysphagia 37, 523–532 (2022). https://doi.org/10.1007/s00455-021-10299-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-021-10299-z