Abstract
Objective
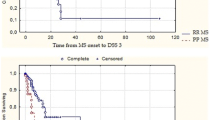
To investigate the prevalence and clinical relevance regarding disability progression in multiple sclerosis patients with a dissociation in clinical and radiological disease expression.
Methods
We prospectively selected patients with early relapsing–remitting multiple sclerosis (MS) or a clinically isolated syndrome (CIS) from the Amsterdam MS cohort. Patients underwent clinical examination at baseline, after 2 years, 6 years and a subset also after 11 years, including the Expanded Disability Status Scale (EDSS), 25-foot walk test (25-FWT) and 9-hole peg test (9-HPT). Brain and spinal cord MRI scans were obtained at baseline and after 2 years. Two years after baseline, patients with dissociation in their clinical and radiological disease progression were identified as: (1) patients with high clinical disease activity (defined by relapses) and low radiological disease activity (defined by white-matter lesions on T2-weighted imaging); or (2) patients with low clinical disease activity and high radiological disease activity. Binary logistic regression analyses were performed to predict disability progression after 6 and 11 years of follow-up. Patients with low clinical and low radiological disease activity were used as the reference group.
Results
The prevalence of clinico-radiological dissociation was low (6.4% had high clinical and low radiological disease activity and 5.1% had a combination of low clinical and high radiological disease activity) compared to 88.5% of patients without a dissociation. Patients with a dissociation of clinical and radiological disease activity did not show a statistically significant difference in risk of disability progression after 6 and 11 years.
Conclusions
A clinico-radiological dissociation is rather a rare phenomenon in MS patients. The clinical relevance of such a dissociation regarding the prediction of disability progression is questionable.

Similar content being viewed by others
Data availability
Data were transparent for all authors.
Code availability
Software application.
References
Wattjes MP, Steenwijk MD, Stangel M (2015) MRI in the diagnosis and monitoring of multiple sclerosis: an update. Clin Neuroradiol 25(Suppl 2):157–165
Barkhof F (2002) The clinico-radiological paradox in multiple sclerosis revisited. Curr Opin Neurol 15:239–245
Reich DS, Lucchinetti CF, Calabresi PA (2018) Multiple sclerosis. N Engl J Med 378:169–180
Polman CH, Reingold SC, Edan G, Filippi M, Hartung HP, Kappos L et al (2005) Diagnostic criteria for multiple sclerosis: 2005 revisions to the "McDonald Criteria". Ann Neurol 58:840–846
Sombekke MH, Wattjes MP, Balk LJ, Nielsen JM, Vrenken H, Uitdehaag BM et al (2013) Spinal cord lesions in patients with clinically isolated syndrome: a powerful tool in diagnosis and prognosis. Neurology 80:69–75
Uitdehaag BMJ (2018) Disability outcome measures in phase III Clinical trials in multiple sclerosis. CNS Drugs 32:543–558
Cadavid D, Cohen JA, Freedman MS, Goldman MD, Hartung HP, Havrdova E et al (2017) The EDSS-Plus, an improved endpoint for disability progression in secondary progressive multiple sclerosis. Mult Scler 23:94–105
Healy BC, Buckle GJ, Ali EN, Egorova S, Khalid F, Tauhid S et al (2017) Characterizing clinical and mri dissociation in patients with multiple sclerosis. J Neuroimaging 27:481–485
Jokubaitis VG, Spelman T, Kalincik T, Lorscheider J, Havrdova E, Horakova D et al (2016) Predictors of long-term disability accrual in relapse-onset multiple sclerosis. Ann Neurol 80:89–100
Gajofatto A, Calabrese M, Benedetti MD, Monaco S (2013) Clinical, MRI, and CSF markers of disability progression in multiple sclerosis. Dis Markers 35:687–699
Fisniku LK, Brex PA, Altmann DR, Miszkiel KA, Benton CE, Lanyon R et al (2008) Disability and T2 MRI lesions: a 20-year follow-up of patients with relapse onset of multiple sclerosis. Brain 131:808–817
Wattjes MP, Rovira À, Miller D et al (2015) Evidence-based guidelines: MAGNIMS consensus guidelines on the use of MRI in multiple sclerosis–establishing disease prognosis and monitoring patients. Nat Rev Neurol 11:597–606
Funding
The MS Center Amsterdam is funded by a program grant (14-358e) from the Stichting voor MS Research (Voorschoten, The Netherlands). None of the funders had any role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
Conceptualization and design of the study: NLF, ID, MPW. Acquisition and analysis of data: NLF, ID, MPW, BM, FB. Statistical analysis: ID, LJB. Drafting of a significant portion of the manuscript and table: all authors.
Corresponding author
Ethics declarations
Conflicts of interest
N.L. van Faals, L.J. Balk, B. Moraal have nothing to disclose. I. Dekker received speaking honoraria from Roche. F. Barkhof serves as editorial board member of Brain, Neuroradiology, Neurology, Multiple Sclerosis Journal and Radiology. He has accepted personal fees from Springer, Bayer, Biogen, Roche, Apitope Ltd, IXICO ltd, Novartis, GeNEuro. Grants from Novartis, TEVA, Merck, Biogen, IMI-EU, GE Healthcare, UK MS Society, Dutch MS research foundation, NWO, NIHR. FB is supported by the NIHR UCLH biomedical research centre. B.M.J. Uitdehaag has received consultancy fees and/or research support from Biogen Idec, Sanofi Genzyme, Merck Serono, Roche and Teva. J. Killestein reports grants and personal fees from Biogen Idec, Novartis, Merck Serono, TEVA, Genzyme, Roche, outside the submitted work. M.P. Wattjes reports personal consultancy and speaking fees from Biogen, Novartis, Janssen, Roche, Celgene, IXICO, Sanofi Genzyme, Bayer Healthcare, Biologix, Genilac, Merck Serono and Teva.
Ethical approval
The study was approved by the Institutional review board of the VU University Medical Center, Amsterdam, The Netherlands.
Consent to participate
Written informed consent was obtained from all participants for the use of the clinical, laboratory and imaging data for research and teaching purposes.
Consent for publication
Written informed consent was obtained from all participants for publishing the data.
Rights and permissions
About this article
Cite this article
van Faals, N.L., Dekker, I., Balk, L.J. et al. Clinico-radiological dissociation of disease activity in MS patients: frequency and clinical relevance. J Neurol 267, 3287–3291 (2020). https://doi.org/10.1007/s00415-020-09991-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-020-09991-1