Abstract
Introduction
The purpose of this study was to investigate the effects of alcohol intoxication in trauma patients in regard to its impact on application of computed tomography (CT) and associated radiation exposure.
Methods
We conducted a retrospective study from a continuous patient cohort. Inclusion criteria: admission to the emergency room of an urban Level 1 trauma center with trauma team activation during a 12-month period (Jan 1st–Dec 31st 2012). Patients with incomplete data, age ≤ 12 years and with neurological diseases were excluded. Demographics, mechanisms, severity and patterns of injury (Abbreviated Injury Scale, Injury Severity Score, Glasgow Coma Scale), blood alcohol concentration (BAC, in permille, ‰), imaging studies (head/whole body CT), radiation exposure, and hospital length of stay, surgical procedures and mortality were evaluated with SPSS statistics (Version 25, IBM Inc., Armonk, New York).
Results
A positive BAC (mean 1.80 ± 0.767) was reported in 19.2% (n = 41/214) of the cohort. Alcohol intoxication was associated with higher utilization of head CT (65.9 vs. 46.8%, p = 0.017) and radiation exposure (231.75 vs. 151.25 mAS, p = 0.045; dose-length product, 583.03 vs. 391.04, p = 0.006). In general, the presence of alcohol was associated with over-triage (p = 0.001), despite minor injury severity (ISS < 9) and a comparable rate of head injuries (p = 0.275). Head injury (AIS ≥ 3) and positive BAC (OR 2.34, 95% CI 1.096–5.001) were identified as strongest independent predictors for head CT.
Conclusion
Alcohol intoxication is a common finding in trauma patients, and the rate of moderate and serious head injuries seems to be comparable to a more severely injured control group. Furthermore, head CT utilization in intoxicated patients is associated with significant radiation exposure, despite poor image quality, due to motion artifacts (27%). Future strategies are required to exclude head injuries safely, while reducing the rate of head CT and associated radiation exposure in intoxicated patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Traumatic brain injury (TBI) has been described as major risk factor for mortality and permanent disability in trauma patients [6]. The symptoms of significant head injury involve disorientation, confusion, and impairment of memory functions or even loss of consciousness, among others. Furthermore, nausea and vomiting are common presentations, impeding the clinical differentiation over alcohol intoxication [9, 18, 24, 30]. Recent studies also suggest that there is a rising number of “found down” patients in emergency departments, who present with an impaired level of consciousness after traumatic and/or nontraumatic illness, therefore, requiring resource and cost-intensive clinical and diagnostic workup by medical and trauma services [11, 14, 15].
The blood alcohol concentration (BAC) is a common parameter used to assess the recent alcohol exposure in emergency patients, and elevated BAC values have been described for a significant proportion of acutely admitted trauma patients [2, 4, 20, 21, 24, 31]. Rau et al. evaluated alcohol-related hospital admissions of trauma patients in Southern Taiwan and identified less severe injuries in patients who consumed alcohol. Furthermore, the authors describe a low percentage of positive findings in head CT [21].
While the classical objective in trauma care is to establish rapid and accurate diagnosis of all injuries [1], this paradigm is especially challenging in intoxicated trauma patients, because of the underlying nontraumatic and traumatic causes of the neurological impairment.
The intoxicated trauma patient represents a unique clinical dilemma, because immediate CT imaging would be required to rule out structural brain damage; however, it exposes especially young patients to significant harmful radiation, with an increased long-term burden for malignancies [8, 12, 13, 16, 17].
Inaba et al. evaluated a continuous series of patients admitted to a Level 1 trauma center during 2002 and 2007 and reported a significant increase in the use of both CT and plain radiographs in the management of trauma patients. While the authors found a significantly higher radiation exposure, there were no demonstrable improvements in the diagnosis of missed injuries, mortality, or length of stay [12].
The increased radiation exposure without clinical benefits represents a threat to patient safety and implies a further evaluation of the dilemma, to reduce the avoidable burden of radiation exposure and potentially associated malignant diseases. We hypothesized that many admissions to the trauma service in an urban environment feature positive BAC values, and that increased CT utilization is associated with an increased radiation exposure. Furthermore, we evaluated the impact of head trauma and alcohol intoxication as independent predictors for head CT utilization.
Patients and methods
A retrospective review of a continuous patient cohort was conducted. Inclusion criteria: admission to the emergency room of an urban Level 1 trauma center with trauma team activation during a 12-month period (Jan–Dec 2012). The following mechanisms of injury were defined: (1) motor vehicle accident, (2) motorcycle accident, (3) bicycle accident, (4) high fall (> 3 m), (5) low fall (< 3 m), (6) penetrating trauma, (7) other mechanisms. Patients with incomplete data, age ≤ 12 years, delayed transfers (incorrect BAC values) and patients with neurological diseases (e.g., seizures, n = 3) were excluded. Demographic data, injury severity and patterns of injury were analyzed using objective score systems (Abbreviated Injury Scale, Injury Severity Score, Glasgow Coma Scale). The blood alcohol concentration (BAC, in permille, ‰), radiologic imaging studies (head/whole body CT), associated radiation exposure [milliampere seconds (mAS); dose length product (DLP)] were documented. The CT imaging studies were performed with a SOMATOM Definition Flash (Siemens, Forchheim, Germany). The dose length product (DLP, in mGy*cm) was recorded for each CT scan. The DLP value was used to estimate the effective radiation dose. Furthermore, the hospital length of stay (LOS) and mortality rate were evaluated.
Statistical analysis
Categorical data were presented as frequencies and percentages. Metric variables were reported as means and standard deviation (SD). The Chi-square or Fisher’s exact test was used for comparison of categorical variables, and Student’s t or Mann–Whitney U test was applied for metric variables. Logistic regression analysis was performed to elucidate the possible impact of various risk factors for obtaining a head CT. Differences were considered statistically significant at p < 0.05. The analyses were performed with SPSS for Windows (Version 25, IBM Inc., NY, USA).
Results
This study includes 214 consecutive trauma patients, in whom a positive BAC (mean 1.80 ± 0.767) was reported in 19.2% (n = 41/214). The mean age of patients with positive BAC was 40.5 years and 45 years for patients with negative BAC. However, the higher incidence of younger individuals in the intoxicated group was not found statistically significant (Table 1). The majority of both patients groups were male, and positive BAC was significantly associated with male patients. In patients without alcohol intoxication, the mean ISS was increased, and the GCS decreased significantly. The leading mechanisms of injury (Table 2) in alcohol-intoxicated patients were low falls (46.3%) and penetrating injuries (19.5%), both tested statistically significant. Positive BAC was less frequently detected in motor vehicle drivers and motorcycle riders. There were no significant differences in the rate of bicycle accidents, struck pedestrians and high falls. In summary, intoxicated patients were involved in fall-related mechanisms in more than 60%, and BAC-negative patients were involved in traffic-related accidents in over 70%.
Except for abdominal and lower extremity injuries, no statistically significant differences were found in the anatomic distribution of injuries (Table 3). Both body regions were more often affected in non-intoxicated individuals.
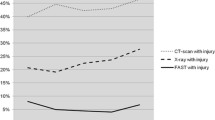
In total, 91 head CT and 84 whole body CT studies were evaluated radiographically and with respect to the associated radiation dose (Table 4). Despite a comparable rate of head injuries, cranial CT was more often performed in alcohol-intoxicated patients (65.9 vs. 46.8%, p = 0.017). Head CT studies without any pathologic findings were with observed comparable frequency in both main groups (9.8 vs. 8.7%, p = 0.513).
When effective radiation doses were calculated, we identified an increased exposure in BAC-positive patients (250.54 vs. 165 DLP, p = 0.035). Whole body CT was less frequently performed in BAC-positive patients (22.0 vs. 43.4%, p = 0.013).
In the intoxicated patient cohort, a significant proportion of head CT scans (n = 10) was of limited diagnostic value due to motion artifacts (27%). Furthermore, 27 scans had no therapeutic consequences or identified injuries, which would have been potentially detectable also by an accurate and thorough physical exam (7 external hematomas, 1 nasal bone fracture; 2 orbital fractures, 1 zygomatic arch fracture, and 1 unstable mandibula fracture, 1 complex midface injury). There were five cases with TBI in the intoxicated patient cohort, including one mild subarachoidal bleeding requiring no surgical treatment, three epidural hematomas (8%) requiring immediate surgical evacuation and one TBI with brain swelling and skull fracture requiring emergent craniotomy. Patients requiring emergency neurosurgical interventions all presented either with aphasia, recurrent vomiting, anisocoria or presented with a loss of consciousness at admission. The CT scans that included the spine also identified one odontoid fracture (2.7%), one C3 fracture (2.7%) with vertebral artery injury (VAI), and two thoracic spine fractures, including one unstable Th-7 Chance type fracture.
No significant differences were found in terms of surgical treatment or in-hospital mortality (Table 5). Finally, a logistic regression analysis was performed to identify predictors for head CT imaging (Table 6). Statistically significant predictors include the following: (1) head injury (AIS ≥ 3): OR 3.44, 95% CI 1.363–8.675, p = 0.009; (2) positive BAC: OR 2.34, 95% CI 1.096–5.001, p = 0.028; (3) age (per year): OR 0.98; 95% CI 0.969–0.997; p = 0.021.
Discussion
A robust association between alcohol use and injury has been reported by multiple studies [19, 22, 29, 32]. We hypothesized that both head injury and alcohol consumption are independent risk factors for head CT and increased associated radiation exposure, resulting in a significant public health and socioeconomic impact.
We conducted a single-center retrospective cohort study investigating the relationship between alcohol intoxication in trauma patients, advanced imaging studies and associated radiation burden. In our setting of an urban trauma center, 19.2% of the study cohort had a positive BAC identified during laboratory examination.
This finding is comparable to previous studies; Vardy et al. performed a cross-sectional study in Glasgow, United Kingdom, and reported that 21% of emergency admissions were implicated by alcohol [31]. Schneiders et al. evaluated injuries under the influence of alcohol in Germany and reported a positive BAC in 19% of all male admissions, compared to a lower rate among female patients [23].
Sperry et al. analyzed the effects of alcohol intoxication in trauma patients in Texas, since 35–50% of TBI patients are under the influence of alcohol. The authors found only little effects of positive BAC values on GCS score [26]. This finding is consistent with other studies, suggesting that the GCS is not effected significantly in patients with an ISS under 25 points [27].
In terms of injury mechanisms, low falls and penetrating trauma were very common in patients with positive BAC. In the univariate analysis of our data, alcohol consumption was associated with male sex, higher GCS and lower general injury severity measured by NISS. These results are in line with the findings reported by Rau et al., who described that patients who consumed alcohol had less severe injuries, but an overuse of CT imaging with a low likelihood of positive findings on brain CT.
This link is also supported by Godout et al., who evaluated the yield of head CT in alcohol-intoxicated patients in the ED [7]. The authors report that only 1.9% of all alcohol-intoxicated patients had evidence of any type of intracranial hemorrhage, but reported a higher rate (2.7, 95% CI = 1.4–4.1%) of positive CT scans in elderly patients (≥ 60 years). In our study, the majority of intoxicated patients (65.9%) received a head CT scan, compared to 46.8% of the control group (p = 0.0017). We identified five intoxicated patients with TBI (12.2%), including one mild SAH. Especially in the context of minor injuries (ISS < 9), intoxicated patients appear to be a significant cause of over-triage. Our data suggest that alcohol-intoxicated patients cause intensive resource utilization due to admission to the emergency room of a Level 1 trauma center with trauma team activation; however, the cohort presented with comparable rates of head injury and lower general injury severity.
The combination of over-triage despite minor injuries and a high rate of resource utilization indicate that this patient group is a major but modifiable cost driver in the health care system [28].
Brenner et al. reported a dramatically increased use of CT in the United States and an attributable radiation-induced cancer burden, estimated at 1.5–2% of all tumors [5]. In this context, a more judicious use of advanced imaging may control risks and costs without compromising care [3]. Although the use of computed tomographic (CT) scanning in severe head trauma is an accepted practice, the indications for its use in minor injury remain ill defined and often subjective [25].
Harr et al. studied patients with head injuries in Oslo, Norway, and found that 35.8% of the patient population had consumed alcohol at the time of admission [10]. Despite an established guideline, a positive BAC resulted in reduced guideline compliance and that over-triage was the main violation. Over-triage and routine CT scanning may result in significant radiation exposure and costs.
Our study confirms that a positive BAC is an independent predictor for head CT utilization and is associated with an increased radiation burden. However, the rate of 65.9% for immediate CT imaging appears to be very high and possibly imposes avoidable radiation exposure and resource utilization.
While we cannot draw these conclusions from our data, Granata et al. suggested that deferred CT imaging of intoxicated patients appears to be a safe practice because routine CT scanning of alcohol-intoxicated patients with altered mental status seems to be of low clinical value. However, deferring CT imaging requires monitoring of the clinical status and is also associated with resource utilization and costs, but it may reduce radiation exposure effectively. Furthermore, prevention strategies targeting young male individuals are required to reduce the prevalence of alcohol-related TBI.
There are several limitations to this study, including its retrospective nature, the single-center perspective, and the fact that patients respond differently on head injury and the effects of alcohol. However, the main findings are supported by the recent literature and our data confirm that positive BAC is a common clinical problem especially in male trauma patients, resulting in significant resource utilization and radiation exposure related to head CT imaging. Further studies are required to develop effective strategies for prevention, enhancing guideline adherence, safety of deferred imaging, reducing the burden of radiation and improving safety in trauma patients.
Conclusion
Alcohol intoxication is a common finding in trauma patients, and the rate of moderate and serious head injuries seems to be comparable to a more severely injured control group. Furthermore, head CT utilization in intoxicated patients is associated with significant radiation exposure, despite poor image quality, due to motion artifacts (27%). Future strategies are required to exclude head injuries safely, while reducing the rate of head CT and associated radiation exposure in intoxicated patients.
Abbreviations
- AIS:
-
Abbreviated Injury Scale
- BAC:
-
Blood alcohol concentration/content
- CCT:
-
Cranial computed tomography
- CT:
-
Computed tomography
- CI:
-
Confidence interval
- DLP:
-
Dose length product
- ER:
-
Emergency room
- GCS:
-
Glasgow Coma Score
- ICU:
-
Intensive care unit
- ISS:
-
Injury severity score
- LOS:
-
Length of stay
- mAS:
-
Milliampere second
- MCA:
-
Motorcycle accident
- MVA:
-
Motor vehicle accident
- NISS:
-
New injury severity score
- OR:
-
Odds ratio
- SBP:
-
Systolic blood pressure
- SD:
-
Standard deviation
- TBI:
-
Traumatic brain injury
- WBCT:
-
Whole body computed tomography
References
Aaland MO, Smith K. Delayed diagnosis in a rural trauma center. Surgery. 1996;120(4):774–8 (discussion 778–779).
Afshar M, Netzer G, Salisbury-Afshar E, Murthi S, Smith GS. Injured patients with very high blood alcohol concentrations. Injury. 2016;47(1):83–8.
Ahmadinia K, Smucker JB, Nash CL, Vallier HA. Radiation exposure has increased in trauma patients over time. J Trauma Acute Care Surg. 2012;72(2):410–5.
Bertholet N, Adam A, Faouzi M, et al. Admissions of patients with alcohol intoxication in the emergency department: a growing phenomenon. Swiss Med Wkly. 2014;144:w13982.
Brenner DJ, Hall EJ. Computed tomography—an increasing source of radiation exposure. N Engl J Med. 2007;357(22):2277–84.
Ghajar J. Traumatic brain injury. Lancet. 2000;356(9233):923–9.
Godbout BJ, Lee J, Newman DH, Bodle EE, Shah K. Yield of head CT in the alcohol-intoxicated patient in the emergency department. Emerg Radiol. 2011;18(5):381–4.
Gottschalk MB, Bellaire LL, Moore T. Radiation exposure in the young level 1 trauma patient: a retrospective review. J Surg Orthop Adv. 2015;24(1):57–63.
Granata RT, Castillo EM, Vilke GM. Safety of deferred CT imaging of intoxicated patients presenting with possible traumatic brain injury. Am J Emerg Med. 2017;35(1):51–4.
Harr ME, Heskestad B, Ingebrigtsen T, Romner B, Ronning P, Helseth E. Alcohol consumption, blood alcohol concentration level and guideline compliance in hospital referred patients with minimal, mild and moderate head injuries. Scand J Trauma Resusc Emerg Med. 2011;19:25.
Howard BM, Kornblith LZ, Conroy AS, et al. The found down patient: a western trauma association multicenter study. J Trauma Acute Care Surg. 2015;79(6):976–82 (discussion 982).
Inaba K, Branco BC, Lim G, et al. The increasing burden of radiation exposure in the management of trauma patients. J Trauma. 2011;70(6):1366–70.
Jones AC, Woldemikael D, Fisher T, Hobbs GR, Prud’homme BJ, Bal GK. Repeated computed tomographic scans in transferred trauma patients: Indications, costs, and radiation exposure. J Trauma Acute Care Surg. 2012;73(6):1564–9.
Ko A, Zaw AA, Barmparas G, et al. Abdominal Injuries in the “Found Down”: is imaging indicated? J Am Coll Surg. 2015;221(1):17–24.
Kornblith LZ, Kutcher ME, Evans AE, et al. The “found down” patient: a diagnostic dilemma. J Trauma Acute Care Surg. 2013;74(6):1548–52.
Kritsaneepaiboon S, Jutiyon A, Krisanachinda A. Cumulative radiation exposure and estimated lifetime cancer risk in multiple-injury adult patients undergoing repeated or multiple CTs. Eur J Trauma Emerg Surg. 2016;44:19–27
Linder F, Mani K, Juhlin C, Eklof H. Routine whole body CT of high energy trauma patients leads to excessive radiation exposure. Scand J Trauma Resusc Emerg Med. 2016;24:7.
McHugo GJ, Krassenbaum S, Donley S, Corrigan JD, Bogner J, Drake RE. The Prevalence of traumatic brain injury among people with co-occurring mental health and substance use disorders. J Head Trauma Rehabil. 2016;32:E65–74
O’Farrell A, Allwright S, Downey J, Bedford D, Howell F. The burden of alcohol misuse on emergency in-patient hospital admissions among residents from a health board region in Ireland. Addiction. 2004;99(10):1279–85.
Raj R, Skrifvars MB, Kivisaari R, Hernesniemi J, Lappalainen J, Siironen J. Acute alcohol intoxication and long-term outcome in patients with traumatic brain injury. J Neurotrauma. 2015;32(2):95–100.
Rau CS, Liu HT, Hsu SY, Cho TY, Hsieh CH. Alcohol-related hospitalisations of trauma patients in Southern Taiwan: a cross-sectional study based on a trauma registry system. BMJ Open. 2014;4(10):e005947.
Salim A, Teixeira P, Ley EJ, DuBose J, Inaba K, Margulies DR. Serum ethanol levels: predictor of survival after severe traumatic brain injury. J Trauma. 2009;67(4):697–703.
Schneiders W, Niemann G, Rammelt S, Meyner T, Rehberg S. Injuries under the influence of alcohol. Unfallchirurg. 2016;120(7):585–9. https://doi.org/10.1007/s00113-016-0164-6.
Sethi M, Heyer JH, Wall S, et al. Alcohol use by urban bicyclists is associated with more severe injury, greater hospital resource use, and higher mortality. Alcohol. 2016;53:1–7.
Simon B, Letourneau P, Vitorino E, McCall J. Pediatric minor head trauma: indications for computed tomographic scanning revisited. J Trauma. 2001;51(2):231–7 (discussion 237–238).
Sperry JL, Gentilello LM, Minei JP, Diaz-Arrastia RR, Friese RS, Shafi S. Waiting for the patient to “sober up”: effect of alcohol intoxication on Glasgow coma scale score of brain injured patients. J Trauma. 2006;61(6):1305–11.
Stuke L, Diaz-Arrastia R, Gentilello LM, Shafi S. Effect of alcohol on Glasgow coma scale in head-injured patients. Ann Surg. 2007;245(4):651–5.
Swearingen A, Ghaemmaghami V, Loftus T, et al. Extreme blood alcohol level is associated with increased resource use in trauma patients. Am Surg. 2010;76(1):20–4.
Talving P, Plurad D, Barmparas G, et al. Isolated severe traumatic brain injuries: association of blood alcohol levels with the severity of injuries and outcomes. J Trauma. 2010;68(2):357–62.
Valdez C, Radomski M, Renne C, Amdur R, Dunne J, Sarani B. Alcohol level and injury severity: is the floppy patient myth true? J Surg Res. 2016;200(2):664–8.
Vardy J, Keliher T, Fisher J, et al. Quantifying alcohol-related emergency admissions in a UK tertiary referral hospital: a cross-sectional study of chronic alcohol dependency and acute alcohol intoxication. BMJ Open. 2016;6(6):e010005.
Yoonhee C, Jung K, Eo E, et al. The relationship between alcohol consumption and injury in ED trauma patients. Am J Emerg Med. 2009;27(8):956–60.
Acknowledgements
This paper has been presented at the 16th European Congress of Trauma and Emergency Surgery in Amsterdam, The Netherlands, and was nominated for the Best Oral Paper Presentation.
Funding
No financial support was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Christian David Weber, Jana Kristina Schmitz, Christina Garving, Klemens Horst, Hans-Christoph Pape, Frank Hildebrand and Philipp Kobbe have no conflicts of interest to disclose.
Rights and permissions
About this article
Cite this article
Weber, C.D., Schmitz, J.K., Garving, C. et al. The alcohol-intoxicated trauma patient: impact on imaging and radiation exposure. Eur J Trauma Emerg Surg 45, 871–876 (2019). https://doi.org/10.1007/s00068-018-0945-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-018-0945-4