Abstract
Background
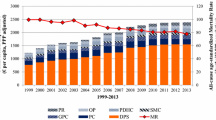
Research using local English data from 2003 to 2012 suggests that a 1% increase in healthcare expenditure causes a 0.78% reduction in mortality, and that it costs the NHS £10,000 to generate an additional quality-adjusted life year (QALY). In 2013, the existing 151 local health authorities (Primary Care Trusts) were abolished and replaced with 212 Clinical Commissioning Groups (CCGs). CCGs retained responsibility for secondary care and pharmaceuticals, but responsibility for primary care and specialised commissioning returned to central administrators.
Objectives
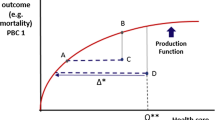
The aim was to extend and apply existing methods to more recent data using a new geography and expenditure base, while improving covariate selection and examining the responsiveness of mortality to expenditure across the mortality distribution.
Methods
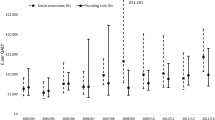
Instrumental variable regression is used to quantify the relationship between mortality and local expenditure. Backward selection and regularised regression are used to identify parsimonious specifications. These results are combined with information about survival and morbidity disease burden to calculate the marginal cost per QALY. Unconditional quantile regression (UQR) is used to examine the response of mortality to expenditure across the mortality distribution.
Results
Backward selection and regularised regression both suggest that the marginal cost per QALY in 2014/15 was about £7000 for locally commissioned services. The UQR results suggest that additional expenditure generates larger health benefits in high-mortality areas and that, if anything, the average size of this heterogeneous response is larger than the response at the mean.
Conclusions
The new healthcare geography and expenditure base can be used to update estimates of the health opportunity costs associated with additional expenditure. The variation in the mortality response across the mortality distribution suggests that the use of the response at the mean will, if anything, underestimate the health opportunity costs associated with a national policy or nationally mandated guidance on the use of new technologies. The health opportunity costs of such policies are likely to be greater (lower) in areas of higher (lower) mortality, increasing health inequalities.
Similar content being viewed by others
References
Edney LC, Afzali HHA, Cheng TC, Karnon J. Estimating the Reference Incremental Cost-Effectiveness Ratio for the Australian Health System. Pharmacoeconomics. 2018;36(2):239–52.
Van Baal P, Perry-Duxberry M, Bakx P, Versteegh M, van Doorslaer E, Brouwer W. A cost-effectiveness threshold based on the marginal returns of cardiovascular hospital spending. Health Econ. 2019;28(1):87–100. https://doi.org/10.1002/hec.3831.
Vallejo-Torres L, Garcia-Lorenzo B, Serrano-Aguilar P. Estimating a cost-effectiveness threshold for the Spanish NHS. Health Econ. 2018;27(4):746–61. https://doi.org/10.1002/hec.3633.
Siverskog J, Henriksson M. Estimating the marginal cost of a life year in Sweden’s public healthcare sector. Eur J Health Econ. 2019;20:751–62. https://doi.org/10.1007/s10198-019-01039-0.
Martin S, Lomas J, Claxton K, et al. How effective is marginal healthcare expenditure? New evidence from England for 2003/04 to 2012/13. Appl Health Econ Health Policy. 2021. https://doi.org/10.1007/s40258-021-00663-3.
Claxton K, Martin S, Soares M, Rice N, Spackman E, Hinde S, Devlin N, Smith PC, Sculpher M. Methods for the estimation of the cost-effectiveness threshold. Health Technol Assess. 2015;19(14):1–503 (v–vi).
Lomas J, Claxton K, Martin S. Estimating the marginal productivity of the English National Health Service from 2003/04 to 2012/13. Value Health. 2019;22(9):995–1002. https://doi.org/10.1016/j.jval.2019.04.1926.
Harrell F. Regression modelling strategies: with applications to linear models, logistic and ordinal regression, and survival analysis. Cham: Springer Series in Statistics; 2015.
Hernandez-Villafuerte K, Zamora B, Feng Y, Parkin D, Devlin N, Towse A. Exploring variations in the opportunity cost cost-effectiveness threshold by clinical area: results from a feasibility study in England. OHE Research Paper, London: Office of Health Economics; 2019. Available at: https://www.ohe.org/publications/exploring-variations-opportunity-cost-cost-effectiveness-threshold-clinical-area. Accessed 20 Sept 2021.
Love-Koh J, Cookson R, Claxton K, Griffin S. Estimating social variation in the health effects of changes in health care expenditure. Med Decis Mak. 2020;40(2):170–82. https://doi.org/10.1177/0272989X20904360.
Andrews M, Elamin O, Hall AR, Kyriakoulis K, Sutton M. Inference in the presence of redundant moment conditions and the impact of government health expenditure on health outcomes in England. Econom Rev. 2017;36(1–3):23–41. https://doi.org/10.1080/07474938.2016.1114205.
Claxton K, Lomas J, Martin S. The impact of NHS expenditure on health outcomes in England: alternative approaches to identification in all-cause and disease specific models of mortality. Health Econ. 2018;27(6):1017–23. https://doi.org/10.1002/hec.3650.
Department of Health/NHS England. Technical guide to the formulae for 2014–15 and 2015–16 revenue allocations to Clinical Commissioning Groups and Area Teams. Department of Health. Available at: https://www.england.nhs.uk/allocations/allocations-2014-15-and-2015-16. Accessed 20 Sept 2021.
Angrist J, Pischke J-S. Mostly harmless econometrics: an empiricist’s companion. Princeton: Princeton University Press; 2009.
Wooldridge JM. Econometric analysis of cross section and panel data. 2nd ed. Cambridge: MIT Press; 2010.
Staiger D, Stock J. Instrumental variables regression with weak instruments. Econometrica. 1997;65:557–86. https://doi.org/10.2307/2171753.
Baum CF, Schaffer ME, Stillman S. ivreg2: Stata module for extended instrumental variables/2SLS, GMM and AC/HAC, LIML and k-class regression. 2016. Available from: http://ideas.repec.org/c/boc/bocode/s425401.html. Accessed 20 Sept 2021.
Pesaran MH, Taylor LW. Diagnostics for IV regressions. Oxf Bull Econ Stat. 1999;61(2):255–65. https://doi.org/10.1111/1468-0084.00128.
Tibshirani R. Regression shrinkage and selection via the Lasso. J R Stat Soc Ser B (Methodol). 1996;58(1): 267–288. Available at http://www.jstor.org/stable/2346178. Accessed 20 Sept 2021.
Ahrens A, Hansen CB, Schaffer M. Lassopack: model selection and prediction with regularized regression in Stata. Stata J. 2020;20(1):176–235. https://doi.org/10.1177/1536867X20909697.
Drukker D, Liu D. Using the lasso for inference in high-dimensional models. The Stata Blog, 9 September. 2019. Available at https://blog.stata.com/2019/09/. Accessed 20 Sept 2021.
Belloni A, Chernozhukov V, Hansen C. Inference on treatment effects after selection among high-dimensional controls. Rev Econ Stud. 2014;81:608–50. https://doi.org/10.1093/restud/rdt044.
Ahrens A, Hansen CB, Schaffer ME. pdslasso and ivlasso: Progams for post-selection and post-regularization OLS or IV estimation and inference. 2018. Available from http://ideas.repec.org/c/boc/bocode/s458459.html. Accessed 20 Sept 2021.
Lê Cook B, Manning WG. Thinking beyond the mean: a practical guide for using quantile regression methods for health services research. Shanghai Arch Psychiatry. 2013;25(1):55–9.
Maclean J, Webber DA, Marti J. An application of unconditional quantile regression to cigarette taxes. J Policy Anal Manag. 2014;33(1):188–210. https://doi.org/10.1002/pam.21724.
Atkins R, Turner AJ, Chandola T, Sutton M. Going beyond the mean in examining relationships of adolescent non-cognitive skills with health-related quality of life and biomarkers in later-life. Econ Hum Biol. 2020;39:100923.
Koenker R, Bassett G. Regression quantiles. Econometrica. 1978;46:33–50.
Borah BJ, Basu A. Highlighting differences between conditional and unconditional quantile regression approaches through an application to assess medication adherence. Health Econ. 2013;22(9):1052–70. https://doi.org/10.1002/hec.2927.
Carrieri V, Jones AM. The income-health relationship “beyond the mean”: new evidence from biomarkers. Health Econ. 2017;26(7):937–56. https://doi.org/10.1002/hec.3372.
Firpo S, Fortin NM, Lemieux T. Unconditional quantile regressions. Econometrica. 2009;77:953–973. See: https://www.jstor.org/stable/40263848. Accessed 20 Sept 2021.
Powell D. Quantile treatment effects in the presence of covariates. RAND Labor and Population Working Paper; 2016. See: https://doi.org/10.7249/WR816. Accessed 20 Sept 2021.
Powell D. Quantile treatment effects in the presence of covariates. Rev Econ Stat. 2020;102(5):994–1005. https://doi.org/10.1162/rest_a_00858.
Baker M, Powell D, Smith TA. genqreg: Stata module for fitting the generalized quantile regression estimator developed in Powell (2016). 2019. See https://ideas.repec.org/c/boc/bocode/s458158.html. Accessed 20 Sept 2021.
Koenker R. Deracinated quantile regression: an R vinaigrette. Mimeo. 2020. Available at: http://www.econ.uiuc.edu/~roger/research/vinaigrettes/DQR.pdf. Accessed 20 Sept 2021.
Santos Silva J. Personal communication, 14 June. 2021.
Rios-Avila F. Recentered influence functions (RIFs) in Stata: RIF regression and RIF decomposition. Stata J. 2020;20(1):51–94. https://doi.org/10.1177/1536867X20909690.
Soares M, Sculpher M, Claxton K. Health opportunity costs: assessing the implications of uncertainty using elicitation methods with experts. Med Decis Mak. 2020. https://doi.org/10.1177/0272989X20916450.
Soares M, Sculpher M, Claxton K. Authors’ response to: “Health Opportunity Costs and Expert Elicitation: A Comment on Soares et al.” by Sampson, Firth, and Towse. Med Decis Mak. 2021. https://doi.org/10.1177/0272989X20987222.
Lakhani A, Olearnik H, Eayres D (eds). Compendium of clinical and health indicators: data definitions and user guide for computer files. London: National Centre for Health Outcomes Development; 2006. An updated version (December 2015) is available at: https://files.digital.nhs.uk/60/236EC2/Compendium%20User%20Guide%202015%20Dec%20Annex%203%20V1.pdf. Accessed 20 Sept 2021.
Aragón MJ, Chalkley M, Goddard M. Defining and measuring unmet need to guide healthcare funding: identifying and filling the gaps. CHE Research Paper 141, University of York; 2017. See: https://eprints.whiterose.ac.uk/135415/1/CHERP141_need_healthcare_funding.pdf. Accessed 20 Sept 2021.
ONS. Health state life expectancies by national deprivation deciles, England and Wales: 2015 to 2017. 2019. See: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthinequalities/bulletins/healthstatelifeexpectanciesbyindexofmultipledeprivationimd/2015to2017#life-expectancy-and-healthy-life-expectancy-in-england-by-the-index-of-multiple-deprivation-2015-imd15-2015-to-2017. Accessed 20 Sept 2021.
PHE/NHS England. Reducing health inequalities resources. 2021. See https://www.england.nhs.uk/about/equality/equality-hub/resources/. Accessed 20 Sept 2021.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This research is funded by the UK’s National Institute for Health Research (NIHR) Policy Research Programme, conducted through the Policy Research Unit in Economic Methods of Evaluation in Health and Social Care Interventions, PR-PRU-1217-20401. The views expressed are those of the authors and not necessarily those of the NIHR, or NHS England or the Department of Health and Social Care.
Conflict of interest
This research is funded by the UK’s NIHR Policy Research Programme, conducted through the Policy Research Unit in Economic Methods of Evaluation in Health and Social Care Interventions, PR-PRU-1217-20401. The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care. Although the results have been presented to NHS England and the Department and members have commented on the research, they had no involvement with the study design; the collection, analysis and interpretation of the data; the writing of the paper; and the decision to submit the article for publication. Stephen Martin, Karl Claxton, James Lomas and Francesco Longo declare that they have no conflict of interest.
Data availability
All of the raw data are either in the public domain or available on request from the data owner. The healthcare expenditure data are available from NHS England (email england.programmebudgeting@nhs.net). The all-cause and disease-specific mortality data are available from NHS Digital (email clinical.indicators@nhs.net). The population size and instrument data are available in Technical Guide to the formulae for 2014-15 and 2015-16 revenue allocations to Clinical Commissioning Groups and Area Teams. This is available at: https://www.england.nhs.uk/allocations/allocations-2014-15-and-2015-16 (accessed 20 September 2021). The socio-economic variables were constructed from the 2011 Population Census and are available from the Office for National Statistics at https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/datasets/2011censuskeystatisticsforlocalauthoritiesinenglandandwales (accessed 20 September, 2021). The IMD 2010 is available from https://www.gov.uk/government/statistics/english-indices-of-deprivation-2010 (accessed 20 September, 2021).
Code availability
Our estimation code is not available, but estimation was undertaken using three user-written commands—ivreg2, ivlasso and rifhdreg—within the commercially available software package Stata 16.
Author contributions
All authors (SM, KC, JL, FL) contributed to the concept and design of this paper. SM led on the analysis and drafting, and the final paper was edited and approved by all four authors. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting these criteria have been omitted.
Ethics approval
Ethical approval is not required.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Martin, S., Claxton, K., Lomas, J. et al. How Responsive is Mortality to Locally Administered Healthcare Expenditure? Estimates for England for 2014/15. Appl Health Econ Health Policy 20, 557–572 (2022). https://doi.org/10.1007/s40258-022-00723-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-022-00723-2