Abstract
Introduction
The purpose of this study was to compare the surgical outcomes between ab interno trabeculotomy (LOT) and iStent inject W implantation (iStent) both combined with cataract surgery, matching the background factors including age, intraocular pressure (IOP), medication score, central corneal thickness (CCT), and axial length.
Methods
A total of 100 eyes from 75/79 patients with primary open-angle glaucoma were included in the LOT/iStent groups. The background factors were matched between the two groups using the propensity score.
Results
There were no significant differences in age, IOP, medication score, CCT, and axial length, preoperatively. The postoperative medication scores were 1.3 ± 1.2 and 1.2 ± 1.2 in the LOT and iStent groups. The postoperative IOPs were 12.8 ± 2.8 and 13.1 ± 2.4 mmHg in the LOT and iStent groups, respectively. The changes in the medication score were − 0.64 ± 1.4 and − 0.44 ± 1.6 in the LOT and iStent groups, respectively. The changes in the IOP were − 2.1 ± 3.3 and − 1.5 ± 3.0 mmHg in the LOT and iStent groups, respectively. These values were not significantly different between the two groups. The postoperative IOP and changes in the IOP were significantly associated with preoperative IOP and CCT. There was no significant difference in the occurrence of postoperative complications (hyphema, 11.0% and 6.0%, and transient ocular hypertension, 8.0% and 5.0%, in the LOT and iStent groups, respectively).
Conclusion
LOT and iStent have similar surgical outcomes with sufficient safety. Postoperative IOP was significantly associated with preoperative IOP and CCT in both groups.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
It is not known whether microhook ab interno trabeculotomy or iStent inject is more effective. |
What was learned from the study? |
The changes in the medication score and the changes in the intraocular pressure were not significantly different between the two groups. |
There was no significant difference in the occurrence of postoperative complications. |
Both surgeries have similar surgical outcomes with sufficient safety. |
Introduction
Glaucoma is one of the leading causes of blindness worldwide [1]. In glaucoma, intraocular pressure (IOP) is the only modifiable established factor to halt the progression of glaucoma, and it should be adequately controlled to avoid visual field (VF) deterioration [2,3,4,5,6,7,8,9,10]. The prevalence of glaucoma also increases with age [11, 12]. Nowadays, minimally invasive glaucoma surgery (MIGS) has greatly expanded the surgical treatment options in glaucoma particularly combined with cataract surgery.
Ab interno trabeculotomy and iStent inject W trabecular micro-bypass (iStent; Glaukos Corp., San Clemente, CA, USA) implantation are two representative examples of MIGS. Both techniques facilitate aqueous outflow, resulting in reduction in IOP; trabeculotomy incises the trabecular meshwork, whereas iStent is inserted into the trabecular meshwork. Both techniques are often used in clinical settings because of their safety and effectiveness [13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35]; however, no study has directly compared the outcomes of the two procedures. As surgical outcomes would be affected by the preoperative conditions, such as and IOP and medications, it is of critical importance that these are matched in the compared groups. This is particularly true in Japan because the application criteria for iStent implantation are that the preoperative IOP is < 25 mmHg with antiglaucoma eye drops and open angle (at least Shaffer grade III), according to the guidelines from the Japanese Ophthalmological Society [36]. In addition, the surgery should be performed in combination with cataract surgery [36]. To overcome these possible problems, we used propensity score analysis in the current study. The propensity score is a conditional probability of being exposed given a set of covariates. We can calculate a propensity score for each subject in an observational study regardless of the actual exposure. Once we have a propensity score for each subject, we then return to the real world of exposed and unexposed. We can match the two groups with the same or very similar propensity score. Thus, the probability of belonging to one group is the same as the probability of belonging to the another. That is, the group selection can be considered as “random” and a direct comparison of the outcomes of the two procedures can be made in a quasi-randomised fashion.
In the current study, surgical outcomes were compared between ab interno trabeculotomy and iStent implantation both combined with cataract surgery, matching the background factors including age, IOP, medication score, central corneal thickness (CCT), and axial length.
Methods
This retrospective multicenter study was approved by the Research Ethics Committees of Seirei Hamamatsu General Hospital (#3835). This study was conducted in accordance with the tenets of the Declaration of Helsinki. All participants signed a written informed consent form for their clinical information to be stored in the hospital database and used for research.
Participants
The study initially included 130 eyes of 94 patients and 100 eyes of 79 patients with primary open-angle glaucoma (POAG) who underwent ab interno trabeculotomy (LOT group) and iStent implantation (iStent group) combined with cataract surgery either at the Department of Ophthalmology in Seirei Hamamatsu General Hospital, Hiroshima University Hospital, Shimane University Hospital, or Saneikai Tsukazaki Hospital between July 2019 and March 2022. All patients were followed up for 12 months. Propensity score matching was performed in the two groups by applying logistic regression analysis, and each patient was 1:1 matched for age, IOP, medication score, CCT, and axial length preoperatively.
The inclusion criteria for the LOT and iStent groups were as follows: typical glaucomatous changes in the optic nerve head (e.g., rim notch with a rim width ≤ 0.1 disk diameters, a vertical cup-to-disk ratio of > 0.7, or a retinal nerve fiber layer defect); glaucomatous VF defects compatible with the optic nerve head changes meeting the Anderson–Patella criteria [37] on two consecutive examinations; wide open angle with gonioscopy; and no abnormal eye-related findings except for POAG and cataract on biomicroscopy, gonioscopy, and funduscopy. The choice of operation method was based on the surgeon’s preference; however, LOT was selected when the IOP was > 25 mmHg with antiglaucoma eye drops, following the guideline from the Japanese Ophthalmological Society [36].
The exclusion criteria for the two groups were as follows: contact lens wearers; patients aged < 20 years; eyes with a history of other ocular diseases, such as any abnormality of the cornea and age-related macular degeneration; and experience of any other ocular surgery, including corneal refractive surgery.
Surgical Technique
In all cases, phacoemulsification with intraocular lens implantation in the posterior chamber in the bag was performed through a clear corneal incision. After successful lens implantation, for the LOT group, trabecular meshwork was incised through (between one and three quadrants) using small trabecular hooks, such as Tanito ab interno microhook® (Inami & Co., Ltd., Tokyo, Japan). For the iStent group, two shots of the second-generation iStent inject W® (Glaukos Corporation, San Clemente, CA, USA) were injected under direct visualization into Schlemm’s canal (SC). Postoperatively, patients could receive topical anti-inflammatory medication for up to 3 months, topical steroid medication for up to 6 weeks, topical antibiotic for up to 6 weeks, topical pilocarpine for up to 6 months, and orally administered acetazolamide for up to 5 days, at the surgeons’ preference. All antiglaucoma medications prescribed preoperatively in patients with glaucoma could be discontinued after the surgery but may be resumed at the discretion of the attending physician in the postoperative follow-up.
Clinical Data Acquisition
The baseline demographic data, such as age, axial length, IOP, and CCT, were collected from the medical charts. The axial length was measured preoperatively using the IOL Master ver. 5.02 (Carl Zeiss Meditec, CA, USA) or OA-2000 (Tomey, Aichi, Japan). The Goldmann applanation tonometer (GAT)-IOP measurements were performed preoperatively and at 12 months postoperatively.
Statistical Analysis
Logistic regression analysis was conducted to calculate a propensity score for each patient to create a 1:1 match. The treatment-related preoperative covariates were age, IOP, medication score, CCT, and axial length.
The baseline numerical clinical factors and postoperative numerical values were compared between the LOT and iStent groups using a linear mixed model in which the random effect was each patient. The linear mixed model is similar to usual linear regression, because it analyzes the association between the predictor variables and a single outcome variable; however, ordinal linear regression analysis is valid when all observations are independent of each other, unlike in the linear mixed model. In the current study, measured eyes were nested within patients and hence they are dependent on each other. The standard errors of regression coefficients will be underestimated when this grouping of the measurements is ignored. The linear mixed model adjusts for this hierarchical structure of the data (measurements are grouped within subjects) and hence bias due to the nested structure of data is avoided.
Subsequently, the association between postoperative IOP and preoperative age, axial length, IOP, CCT, and medication score was investigated using the linear mixed model, in each of the LOT and iStent groups. Similar analysis was conducted between the change in the IOP (calculated as postoperative IOP minus preoperative IOP) and preoperative age, axial length, IOP, CCT, and medication score.
Finally, the changes in the IOP and changes in the medication score (calculated as postoperative medication score minus preoperative medication score) were compared between LOT and iStent, in each of the three subgroups according to the preoperative IOP (< 14, 14–18, and > 18 mmHg).
All data processing and analyses were performed using the statistical programming language R (The R Foundation for Statistical Computing, Vienna, Austria).
Results
A total of 100 eyes from 75 patients with POAG who had undergone LOT combined with cataract surgery and 100 eyes from 79 patients with POAG who had undergone iStent combined with cataract surgery were included in the final analysis. The baseline characteristics of each group are shown in Table 1. The preoperative ages were 72.8 ± 8.1 (mean ± standard deviation) and 74.5 ± 8.8 years in the LOT and iStent groups, respectively, which were not significantly different (p = 0.98, linear mixed model). The preoperative axial lengths were 24.8 ± 1.9 and 24.7 ± 1.7 mm in the LOT and iStent groups, respectively, which were not significantly different (p = 0.93). The preoperative medication scores were 2.0 ± 1.4 and 1.6 ± 1.5 in the LOT and iStent groups, respectively, which were not significantly different (p = 0.093). The preoperative IOPs were 14.9 ± 3.3 and 14.6 ± 3.3 mmHg in the LOT and iStent groups, respectively, which were not significantly different (p = 0.42). The preoperative CCTs were 525.9 ± 47.6 and 530.5 ± 41.5 μm in the LOT and iStent groups, respectively, which were not significantly different (p = 0.93). The preoperative IOP was not significantly associated with any of age, axial length, medication score, and CCT, in both groups (p > 0.05, Table 2), except for age in the iStent group (p = 0.043). Medication score and IOP were significantly lower postoperatively than preoperatively in both groups (p < 0.001).
The comparisons of the postoperative medication score and IOP are shown in Table 3. The postoperative medication scores were 1.3 ± 1.2 and 1.2 ± 1.2 in the LOT and iStent groups, respectively, which were not significantly different (p = 0.90, linear mixed model). The postoperative IOPs were 12.8 ± 2.8 and 13.1 ± 2.4 mmHg in the LOT and iStent groups, respectively, which were not significantly different (p = 0.95). Similarly, as shown in Table 3, the changes in the medication score were − 0.64 ± 1.4 and − 0.44 ± 1.6 in the LOT and iStent groups, respectively, which were not significantly different (p = 0.18). The changes in the IOP were − 0.64 ± 1.4 and − 0.44 ± 1.6 mmHg in the LOT and iStent groups, respectively, which were not significantly different (p = 0.37).
As shown in Table 4, both in the LOT and iStent groups, the preoperative IOP (the coefficients were 0.27 and 0.30 with p = 0.0012 and p < 0.001 in the LOT and iStent groups, respectively; linear mixed model) and CCT (the coefficients were 0.018 and 0.017 with p = 0.0041 and p = 0.0022 in the LOT and iStent groups, respectively) were significantly associated with postoperative GAT-IOP. Similarly, both in the LOT and iStent groups, the preoperative IOP (the coefficients were − 0.77 and − 0.70 with p < 0.001 and p < 0.001 in the LOT and iStent groups, respectively; linear mixed model) and CCT (the coefficients were 0.019 and 0.017 with p = 0.0036 and p = 0.0023 in the LOT and iStent groups, respectively) were significantly associated with the change in the IOP (Table 5).
In the LOT and iStent groups, 11 and 6 eyes had postoperative hyphema (with niveau formation), whereas 9 and 5 eyes had postoperative ocular hypertension of > 29 mmHg, respectively (Table 6). No association was noted between the occurrence of these complications and operation method (p = 0.21 and p = 0.89, generalized linear mixed model). All of these conditions improved without additional surgical interventions.
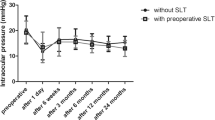
As shown in Fig. 1, the changes in the IOP were not significantly different between the LOT and iStent groups in all three subgroups according to the preoperative IOP (< 14, 14–18, and > 18 mmHg) (p > 0.05, linear mixed model). These values were significantly smaller than 0 in two subgroups (14–18 and > 18 mmHg) within both the LOT and iStent groups (p < 0.001). As shown in Fig. 2, the changes in the medication score were significantly different between the LOT and iStent groups in the subgroup with preoperative IOP 14–18 mmHg (p = 0.045, linear mixed model) but not in the other subgroups (preoperative IOP, < 14 or > 18 mmHg) (p > 0.05, linear mixed model). These values were significantly smaller than 0 in three of the five subgroups (p < 0.05).
Comparison of the changes in the intraocular pressure (IOP) according to the preoperative IOP. The changes in the IOP are not significantly different between the trabeculotomy and iStent groups in all three subgroups according to the preoperative IOP. The gray color suggests no significant difference from zero. The red color suggests a significant difference from zero (p < 0.01). N.S. not significant
Comparison of the changes in the medication score according to preoperative intraocular pressure (IOP). The changes in the medication score were not significantly different between the trabeculotomy and iStent groups in all three subgroups according to the preoperative IOP. The gray color suggests no significant difference from zero. The pink color suggests a significant difference from zero (p < 0.05). The red color suggests a significant difference from zero (p < 0.01). N.S. not significant. *p < 0.05
Discussion
In the current study, surgical outcomes were compared between LOT and iStent both combined with cataract surgery (both 100 eyes). These eyes were matched for the background factors, including age, IOP, medication score, CCT, and axial length, using the propensity score. The results showed that all postoperative IOPs, postoperative medication scores, changes in the IOP, and changes in the medication score were not significantly different between the two groups. Both preoperative IOP and the change in the IOP were significantly associated with preoperative IOP and CCT in the LOT and iStent groups. A decrease in either the IOP or medication score can be expected even with a very low (< 14 mmHg) preoperative IOP.
Most previous studies investigated the outcome of LOT during a postoperative follow-up period of < 1 year; however, a recent study reported a postoperative IOP at 1 year of 15–16 mmHg (the median medication score was 5) [21]. The postoperative IOP values in the current study were relatively lower (12.7 mmHg with a medication score of 1.3) than those in the previous study (Table 2) [21]. This may be because of the difference in the studied samples. For instance, there was a significant difference in the preoperative IOP: 27–28.5 mmHg (the median medication scores were 3.5–4) in the previous study [21] and 14.9 or 14.6 mmHg (the mean medication score was 2.0 or 1.6) in the current study. In addition, only patients with POAG were included in the current study, whereas there was a mixture of POAG, exfoliation glaucoma, steroid-induced glaucoma, and other secondary glaucomas in the previous study [21]. Another previous study with a lower preoperative IOP (between 16.9 and 18.6 mmHg with medication scores of 2.8 and 3.1) reported a 1-year postoperative IOP between 10.9 and 13.7 mmHg (the medication scores were 0.9 and 1.4) [23, 24], which is similar to the current result; however, it is not appropriate to directly compare this with the result of the current study because exfoliation glaucoma was also included. With iStent (two iStent inject® implantations), a similar 1-year postoperative IOP has been reported with LOT described earlier between 11.4 and 16.9 mmHg (the medication scores were between 0.30 and 1.28) from a preoperative IOP between 15.8 and 21.3 mmHg (the medication scores were between 0.8 and 2.2) [26, 27, 29, 30, 33]. These values were 13.1 mmHg (the medication score was 1.2) postoperatively (Table 3) and 14.6 mmHg (the medication score was 1.6) preoperatively in the iStent group, in the current study (Table 1).
From their observations in enucleated human eyes, Rosenquist et al. reported that aqueous outflow resistance incrementally decreased with increasing degree of incision: 30%, 60%, and 71% reductions in the IOP with 30°, 120°, and 360° incisions, respectively [38]. In contrast, it has remained debatable whether IOP incrementally decreases with increasing degree of incision. For instance, Manabe et al. [39] examined the effect of the extent of incision (between 150° and 360°) on postoperative IOP, and no significant association was observed [39]. No significant difference was observed in the IOP reduction between 180° and 360° incisions [24] and between the 1- and 2-quadrant incisions [21]. Both iStent and LOT are glaucoma surgeries facilitating the aqueous outflow by decreasing the resistance of the trabecular meshwork; however, iStent removes this resistance at two locations with an 80-μm-diameter circle, whereas it is at a wider angle in LOT. Nonetheless, in the current study, there was no significant difference in the postoperative IOP and change in the IOP between these two groups. This may imply that the decrease in the extent of the incision does not affect postoperative IOP, even < 150°. However, a previous study has suggested that second-generation iStent inject (two stent implantations) resulted in a lower postoperative IOP than first-generation iStent (one stent implantation) [29]. One of the possible reasons for the contradictory results may be the difference of the studied samples; these were a mixture of POAG and other open-angle glaucomas (35.9% or 16.3%), and the medication score was significantly different between the first- and second-generation groups.
In the current study, a higher preoperative IOP was significantly associated with a higher postoperative IOP, in both the LOT and iStent groups (Tables 4 and 5). This is in agreement with several previous studies with LOT [22, 23, 40] and iStent [30, 33]. Of note, in the current study, a larger reduction in the IOP was also significantly associated with a higher postoperative IOP, in both the LOT and iStent groups. In brief, the current results suggest that a larger magnitude of IOP reduction can be expected in the eyes with a higher preoperative IOP; however, the value of postoperative IOP itself tends to remain at a higher level in such eyes. The current results also suggested that a thicker CCT was also significantly associated with a higher postoperative IOP and larger magnitude of IOP reduction (Tables 4 and 5). One of the reasons for this finding would be that the IOP tended to be overestimated in the eyes with a thick cornea. It has been reported that the IOP reading with the Goldmann applanation tonometry increased approximately 0.032 or 0.012 mmHg per 1-μm increase in the CCT [41, 42]. This would affect not only the postoperative IOP reading but also the change in the IOP. In contrast to the postoperative IOP reading and the change in the IOP, no significant association was observed between the CCT and preoperative IOP (Table 2). Further investigation may be needed to shed light on the association between the CCT and outcome of LOT and iStent.
In the current study, both surgical groups had sufficient safety. The occurrences of hyphema have been reported to be between 17% and 50% with LOT [19, 21,22,23] and between 0% and 6% with iStent [27, 29, 30, 33]. In addition, a previous study has reported a positive correlation between the extent of the incision in SC (between 150° and 320°) and the hyphema score [39]. Another study has reported a significant difference between the 180° and 360° SC incisions for the frequency of postoperative hyphema [24]. These results could imply a higher occurrence of hyphema in the LOT group than in the iStent group; however, these values were 11.0% and 6.0% in the LOT and iStent groups, respectively, without a significant difference (Table 6). This may be because the occurrence of hyphema increases probably when the incision extent is beyond 180° [21, 23]. Another possible reason may be the relatively low occurrence rate in the LOT group in the current study that all LOT procedures were performed by well-experienced surgeons, and it was unlikely that tissues other than the trabecular meshwork, such as collector channels, were damaged during surgery.
The current study has some limitations. First, this was a retrospective study of patients followed up for 12 months. Hence, those who failed and had additional surgical interventions were not included. Because iStent is often performed in the eyes at a relatively early stage, it is clinically rare that such an additional surgical procedure is performed within 12 months after iStent. The current study suggested that the surgical outcomes are similar between LOT and iStent in such cases. A further study should be conducted to compare the outcomes of these surgeries in the eyes needing more aggressive treatments. In addition, LOT and iStent implantation facilitate aqueous outflow by decreasing the resistance of trabecular meshwork; however, it is not possible to separate the effects of LOT and iStent implantation themselves from that associated with cataract surgery because these LOT and iStent implantations were performed in combination with cataract surgery in the current study; indeed, solo iStent surgery is not allowed in Japan [43]. Future research should be conducted to compare the effects of solo LOT and iStent surgeries preparing such cases in the future. In addition, the status of VF damage could not be collected from all patients preoperatively, to be compared between the two groups.
Conclusions
The current study compared surgical outcomes between LOT and iStent both combined with cataract surgery, matching the background factors including age, IOP, medication score, CCT, and axial length, using the propensity score. The results showed that both the postoperative IOP and change in the IOP and change in the medication score were not significantly different between the two groups. Both preoperative IOP and change in the IOP were significantly associated with the preoperative IOP and CCT in the LOT and iStent groups. A decrease in either the IOP or medication score can be expected even with a very low (< 14 mmHg) preoperative IOP.
References
Quigley HA. Glaucoma. Lancet. 2011;377:1367–77.
Heij A, Leske MC, Bengtsson B, Hyman L, Bengtsson B, Hussein M. Reduction of intraocular pressure and glaucoma progression: results from the Early Manifest Glaucoma Trial. Arch Ophthalmol (Chicago, Ill: 1960) 2002;120:1268–79.
Garway-Heath DF, Crabb DP, Bunce C, et al. Latanoprost for open-angle glaucoma (UKGTS): a randomised, multicentre, placebo-controlled trial. Lancet. 2015;385:1295–304.
Leske MC, Heijl A, Hyman L, Bengtsson B, Dong L, Yang Z. Predictors of long-term progression in the early manifest glaucoma trial. Ophthalmology. 2007;114:1965–72.
Holmin C, Thorburn W, Krakau CE. Treatment versus no treatment in chronic open angle glaucoma. Acta Ophthalmol. 1988;66:170–3.
Pajic B, Pajic-Eggspuehler B, Hafliger IO. Comparison of the effects of dorzolamide/timolol and latanoprost/timolol fixed combinations upon intraocular pressure and progression of visual field damage in primary open-angle glaucoma. Curr Med Res Opin. 2010;26:2213–9.
Migdal C, Gregory W, Hitchings R. Long-term functional outcome after early surgery compared with laser and medicine in open-angle glaucoma. Ophthalmology 1994;101:1651–6; discussion 7.
Jay JL, Murray SB. Early trabeculectomy versus conventional management in primary open angle glaucoma. Br J Ophthalmol. 1988;72:881–9.
Musch DC, Gillespie BW, Lichter PR, Niziol LM, Janz NK, Investigators CS. Visual field progression in the Collaborative Initial Glaucoma Treatment Study the impact of treatment and other baseline factors. Ophthalmology. 2009;116:200–7.
The AGIS Investigators. The Advanced Glaucoma Intervention Study (AGIS): 7. The relationship between control of intraocular pressure and visual field deterioration.Am J Ophthalmol 2000;130:429–40.
Miglior S, Pfeiffer N, Torri V, Zeyen T, Cunha-Vaz J, Adamsons I. Predictive factors for open-angle glaucoma among patients with ocular hypertension in the European glaucoma prevention study. Ophthalmology. 2007;114:3–9.
Gordon MO, Beiser JA, Brandt JD, et al. The ocular hypertension treatment study: baseline factors that predict the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002;120:714–20.
Salinas L, Chaudhary A, Berdahl JP, et al. Goniotomy using the Kahook dual blade in severe and refractory glaucoma: 6-month outcomes. J Glaucoma. 2018;27:849–55.
Berdahl JP, Gallardo MJ, ElMallah MK, et al. Six-month outcomes of goniotomy performed with the Kahook dual blade as a stand-alone glaucoma procedure. Adv Ther. 2018;35:2093–102.
Greenwood MD, Seibold LK, Radcliffe NM, et al. Goniotomy with a single-use dual blade: short-term results. J Cataract Refract Surg. 2017;43:1197–201.
SooHoo JR, Seibold LK, Kahook MY. Ab interno trabeculectomy in the adult patient. Middle East Afr J Ophthalmol. 2015;22:25–9.
Omoto T, Fujishiro T, Asano-Shimizu K, et al. Comparison of the short-term effectiveness and safety profile of ab interno combined trabeculotomy using 2 types of trabecular hooks. Jpn J Ophthalmol. 2020;64:407–13.
Tanito M, Ikeda Y, Fujihara E. Effectiveness and safety of combined cataract surgery and microhook ab interno trabeculotomy in Japanese eyes with glaucoma: report of an initial case series. Jpn J Ophthalmol. 2017;61:457–64.
Tanito M, Sano I, Ikeda Y, Fujihara E. Short-term results of microhook ab interno trabeculotomy, a novel minimally invasive glaucoma surgery in Japanese eyes: initial case series. Acta Ophthalmol. 2017;95:e354–60.
Tanito M, Sano I, Ikeda Y, Fujihara E. Microhook ab interno trabeculotomy, a novel minimally invasive glaucoma surgery, in eyes with open-angle glaucoma with scleral thinning. Acta Ophthalmol. 2016;94:e371–2.
Mori S, Murai Y, Ueda K, et al. Comparison of efficacy and early surgery-related complications between one-quadrant and two-quadrant microhook ab interno trabeculotomy: a propensity score matched study. Acta Ophthalmol. 2021;99:898–903.
Sato T, Kawaji T, Hirata A, Mizoguchi T. 360-degree suture trabeculotomy ab interno with phacoemulsification in open-angle glaucoma and coexisting cataract: a pilot study. BMJ Open Ophthalmol. 2018;3: e000159.
Okada N, Hirooka K, Onoe H, Murakami Y, Okumichi H, Kiuchi Y. Comparison of efficacy between 120 degrees and 180 degrees Schlemm’s canal incision microhook ab interno trabeculotomy. J Clin Med. 2021;10:318.
Sato T, Kawaji T. 12-month randomised trial of 360 degrees and 180 degrees Schlemm’s canal incisions in suture trabeculotomy ab interno for open-angle glaucoma. Br J Ophthalmol. 2021;105:1094–8.
Dorairaj SK, Kahook MY, Williamson BK, Seibold LK, ElMallah MK, Singh IP. A multicenter retrospective comparison of goniotomy versus trabecular bypass device implantation in glaucoma patients undergoing cataract extraction. Clin Ophthalmol. 2018;12:791–7.
Gillmann K, Mansouri K, Ambresin A, Bravetti GE, Mermoud A. A prospective analysis of iStent inject microstent implantation: surgical outcomes, endothelial cell density, and device position at 12 months. J Glaucoma. 2020;29:639–47.
Gonnermann J, Bertelmann E, Pahlitzsch M, Maier-Wenzel AB, Torun N, Klamann MK. Contralateral eye comparison study in MICS & MIGS: Trabectome® vs. iStent inject®. Graefes Arch Clin Exp Ophthalmol. 2017;255:359–65.
Guedes RAP, Gravina DM, Lake JC, Guedes VMP, Chaoubah A. Intermediate results of iStent or iStent inject implantation combined with cataract surgery in a real-world setting: a longitudinal retrospective study. Ophthalmol Ther. 2019;8:87–100.
Paletta Guedes RA, Gravina DM, Paletta Guedes VM, Chaoubah A. Two-year comparative outcomes of first- and second-generation trabecular micro-bypass stents with cataract surgery. Clin Ophthalmol. 2021;15:1861–73.
Hooshmand J, Rothschild P, Allen P, Kerr NM, Vote BJ, Toh T. Minimally invasive glaucoma surgery: comparison of iStent with iStent inject in primary open angle glaucoma. Clin Exp Ophthalmol. 2019;47:898–903.
Klamann MK, Gonnermann J, Pahlitzsch M, et al. iStent inject in phakic open angle glaucoma. Graefes Arch Clin Exp Ophthalmol. 2015;253:941–7.
Salby AM, Skalicky SE. Combined iStent(®) inject trabecular micro-bypass and phacoemulsification in Australian patients with open-angle glaucoma. Clin Ophthalmol. 2020;14:985–93.
Salimi A, Clement C, Shiu M, Harasymowycz P. Second-generation trabecular micro-bypass (iStent inject) with cataract surgery in eyes with normal-tension glaucoma: one-year outcomes of a multi-centre study. Ophthalmol Ther. 2020;9:585–96.
Salimi A, Watt H, Harasymowycz P. Three-year outcomes of second-generation trabecular micro-bypass stents (iStent inject) with phacoemulsification in various glaucoma subtypes and severities. J Glaucoma. 2021;30:266–75.
Silveira Seixas RC, Balbino M, Basile Neto A, de Alcantara Almeida Costa A, Jordao M, Russ HHA. Mid-term evaluation of iStent Inject(®) trabecular micro-bypass stent implantation with or without phacoemulsification: a retrospective study. Clin Ophthalmol 2020;14:4403–13.
Japanese Guidelines for Use of iStent® Trabecular micro bypass in combination with cataract surgery. Nippon Ganka Gakkai Zasshi. 2016;120:494–7.
Anderson DR, Patella VM. Automated static perimetry. 2nd ed. St.Louis: Mosby; 1999.
Rosenquist R, Epstein D, Melamed S, Johnson M, Grant WM. Outflow resistance of enucleated human eyes at two different perfusion pressures and different extents of trabeculotomy. Curr Eye Res. 1989;8:1233–40.
Manabe SI, Sawaguchi S, Hayashi K. The effect of the extent of the incision in the Schlemm canal on the surgical outcomes of suture trabeculotomy for open-angle glaucoma. Jpn J Ophthalmol. 2017;61:99–104.
Tanito M, Sugihara K, Tsutsui A, Hara K, Manabe K, Matsuoka Y. Effects of preoperative intraocular pressure level on surgical results of microhook ab interno trabeculotomy. J Clin Med. 2021;10:3327.
Wei W, Fan Z, Wang L, Li Z, Jiao W, Li Y. Correlation analysis between central corneal thickness and intraocular pressure in juveniles in Northern China: the Jinan city eye study. PLoS ONE. 2014;9: e104842.
Suzuki S, Suzuki Y, Iwase A, Araie M. Corneal thickness in an ophthalmologically normal Japanese population. Ophthalmology. 2005;112:1327–36.
Japanese guidelines for use of iStent trabecular micro bypass in combination with cataract surgery. Nippon Ganka Gakkai Zasshi 2016;120(7):494–7.
Acknowledgements
Author Contributions
Conceptualization: Ryo Asaoka, Methodology: Ryo Asaoka, Formal analysis: Ryo Asaoka, investigation: Ryo Asaoka, Writing—original draft preparation: Ryo Asaoka; Writing—review and editing: Ryo Asaoka, Shunsuke Nakakura, Tsukasa Mochizuki, Akiko Ishida, Yuri Fujino, Kaori Ishii, Akira Obana, Masaki Tanito and Yoshiaki Kiuchi, Funding acquisition: Ryo Asaoka and Yuri Fujino, Resources: Ryo Asaoka, Shunsuke Nakakura, Tsukasa Mochizuki, Akiko Ishida, Yuri Fujino, Kaori Ishii, Akira Obana, and Masaki Tanito, Supervision: Shunsuke Nakakura, Masaki Tanito, and Yoshiaki Kiuchi.
Funding
This study was supported by grants (numbers 19H01114, 18KK0253, 20K09784 and 20K18337) from the Ministry of Education, Culture, Sports, Science, and Technology of Japan; the Translational Research program and Japan Glaucoma Society Research Project Support Program. The Rapid Service Fee was funded by the authors.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethical Approval
This retrospective multicenter study was approved by the Research Ethics Committees of Seirei Hamamatsu General Hospital (#3835). This study was conducted in accordance with the tenets of the Declaration of Helsinki. All participants signed a written informed consent form for their clinical information to be stored in the hospital database and used for research.
Conflict of Interest
Ryo Asaoka, Shunsuke Nakakura, Tsukasa Mochizuki, Akiko Ishida, Yuri Fujino, Kaori Ishii, Akira Obana, Masaki Tanito, Yoshiaki Kiuchi have nothing to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Asaoka, R., Nakakura, S., Mochizuki, T. et al. Which is More Effective and Safer? Comparison of Propensity Score-Matched Microhook Ab Interno Trabeculotomy and iStent Inject. Ophthalmol Ther 12, 2757–2768 (2023). https://doi.org/10.1007/s40123-023-00777-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-023-00777-y