Abstract
Introduction
Older adults and patients with underlying conditions such as immunocompromised (IC) populations (e.g., due to medical conditions or immunosuppressive medication) are at increased risk for herpes zoster (HZ). The first HZ recombinant vaccine for IC patients was approved in 2020. Limited evidence exists to inform decision-makers on HZ incidence in high-risk patients in Europe. This systematic literature review (SLR) assessed HZ incidence across 14 high-risk populations in the European Union/European Economic Area, Switzerland, and the United Kingdom.
Methods
An SLR (Embase, Medline, 2002–2022, observational studies) was performed to identify HZ incidence (i.e., primary outcomes: rate or cumulative; secondary: relative incidence) in type 1 and 2 diabetes mellitus (DM); chronic obstructive pulmonary disease and asthma; depression; rheumatic disorders (RD); multiple sclerosis (MS); inflammatory bowel diseases (IBD); psoriasis; lupus; human immunodeficiency virus (HIV); solid organ transplantation (SOT); solid organ malignancy (SOM); hematologic malignancy (HM); and stem cell transplantation (SCT).
Results
Of 776 unique records screened, 59 studies were included (24 reported incidence rate per 1000 person-years; two, cumulative incidence per 1000 persons; and 33, relative incidence). The highest incidence rates were reported for SOT (12.1–78.8) and SCT (37.2–56.1); HM (2.9–32.0); RD (0.41–21.5); lupus (11.0–16.5); IC mixed population (11.3–15.5); HIV/AIDS (11.8–13.0); chronic respiratory diseases (4.7–11.4); SOM (8.8–11.0); IBD (7.0–10.8); DM (4.3–9.4); depression (7.2–7.6); MS (5.7–6.3); and psoriasis (5.3–6.1). In many high-risk populations, HZ incidence was higher for older age groups, women, and some treatments.
Conclusions
The HZ incidence rate in Europe increased with age and varied across high-risk populations, with high rates for solid organ and stem cell transplants, cancer, and rheumatoid arthritis. Most studies were retrospective with methodological differences affecting generalizability and comparability. Future studies should stratify data by IC population, age, sex, severity, medication, and study timeframe.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
The incidence of herpes zoster (HZ) in Europe is 2.0–4.6 in the general population, however, age and immunosuppression are known important risk factors for HZ. |
A recent systematic review of HZ incidence in immunocompromised (IC) patients was performed for the United States, however, limited data are available in IC patients in Europe. |
This systematic review (SLR) in Europe included Medline and Embase searches for observational studies, published from January 2002 to January 2022 in multiple languages, reporting HZ incidence across 14 IC populations. |
What was learned from the study? |
This SLR characterizes HZ incidence in a broad range of patients at increased risk of HZ in Europe. HZ incidence was significantly increased in multiple IC patients, in older IC age groups, in women, and for some treatments. |
The first HZ vaccine for IC populations was approved in the EU in 2020. The evidence, showing HZ incidence is increased in multiple IC conditions, age and treatment groups, could help inform decision-making on vaccination. |
Introduction
Primary infection by the varicella-zoster virus leads to childhood varicella (chickenpox) in the majority of the population. The virus remains dormant in the dorsal root ganglia, and can be reactivated later in life, causing herpes zoster (HZ) [1]. The main factors causing virus-specific cellular immunity to wane are ageing and immunosuppression, due to immune-compromising conditions or immunosuppressive medication [2].
Currently, two herpes zoster vaccines are licensed (a live-attenuated vaccine and an adjuvanted recombinant vaccine to prevent HZ and postherpetic neuralgia (PHN) in healthy older adults [3]. Since 2020, the recombinant vaccine was also approved for adults aged ≥ 18 years at increased risk of HZ in the EU [4]. HZ vaccination is the standard of care in the United States (US), and European countries are increasingly offering HZ vaccination to certain populations as part of adult immunization programs [5, 6].
Without vaccination, around 30% of people develop HZ during their lifetime [7]. The incidence rate of HZ (per 1000 person-years) in the general population in Europe is between 2 and 4 in adults aged < 50 years, increasing to 7–8 in people over 50 years old, and up to 10 in those over 80 years old [8, 9]. HZ is a frequent medical condition that is expected to increase due to an ageing population, with a severe impact on patients’ health-related quality of life [1] and an important burden to the healthcare system [10].
HZ clinical symptoms typically begin with pain in the affected dermatome for at least 2 days prior to skin eruptions; an acute phase lasting up to 30 days with a painful rash that does not respond to non-steroidal pain medication; and severe chronic pain for 30–90 days after the rash has healed. PHN is a frequent complication of HZ that is difficult to treat and involves pain for more than 90 days post-rash. PHN incidence and severity also increase with age [1, 11]. Ophthalmic HZ is also associated with significant complications and the risk of blindness [1].
In immunocompromised (IC) populations, such as those with cancer, human immunodeficiency virus (HIV), hemopathies, solid organ or bone marrow transplants or patients on immunosuppressive therapies, HZ can be more severe. For example, there is a higher risk of severe disease (e.g., cutaneous and/or systemic disseminated HZ [1]), of complications [12, 13], of disease recurrence [14] (e.g., HZ recurs in around 6.2% overall, increasing to 30% in IC patients [1]) and of mortality [15]. Central nervous system manifestations associated with HZ (e.g., encephalitis, myelitis, cerebrovascular disease, radiculitis and Guillain–Barré syndrome) are also predominantly reported in IC patients [1].
The most important risk factors for HZ are increasing age and immunosuppression [2]. While age-related risks are well documented in the literature, the incidence of HZ in IC populations is less well described. A recent systematic review was the first to assess overall HZ risk in IC populations: this study focused on the US adult population and five IC conditions i.e., hematopoietic stem cell transplant (HSCT), hematologic malignancies, solid organ transplant, solid tumor malignancies and HIV [2]. There has also been a systematic review of HZ epidemiology and burden in Latin American countries, which found a higher risk of HZ and complications in IC versus immunocompetent populations [12]. Other systematic reviews have focused on non-IC populations. A systematic review of global HZ incidence focused on the general population (and immunocompetent populations) in adults over 50 years old, and found that HZ incidence is increasing in countries over time, as well as due to ageing [16]. Temporal studies have shown that the incidence of HZ has been increasing worldwide across all age groups, pre-dating the introduction of vaccination programs [14]. In Europe, a systematic review of HZ incidence, focused on immunocompetent populations, identified comparable incidence rates across the region, increasing with age [8].
As HZ burden may increase with growing numbers of aging population and co-morbidities, better estimates of HZ incidence in populations at increased risk are needed to inform vaccine policy decision makers. The aim of this study was to perform a systematic literature review of the incidence of HZ in high-risk populations in the European Union/European Economic Area (EU/EEA), Switzerland and the United Kingdom (UK), across 14 high-risk populations including: type 1 and 2 diabetes mellitus (DM); chronic respiratory diseases (chronic obstructive pulmonary disease [COPD] and asthma); depression; rheumatic disorders; multiple sclerosis (MS); inflammatory bowel disease (IBD); psoriasis; lupus; HIV; solid organ transplantation; solid organ malignancy; hematologic malignancy; and stem cell transplantation.
Methods
Search Strategy and Selection Criteria
A systematic review of the literature was performed, following Cochrane Collaboration [17] and Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines [18] for performing and reporting systematic reviews. The search was performed in Medline (via PubMed) and Embase, for publications in English, German, Dutch, French, Spanish, and Italian, from January 1, 2002 to January 1, 2022, and combined search terms for HZ, incidence, high-risk populations, and countries of interest (see Supplemental file 1). Study designs of interest were prospective and retrospective observational studies e.g., cohort studies, passive surveillance studies and other controlled/uncontrolled studies.
The grey literature was also searched using disease search terms (e.g., zoster, shingles), in international health websites [19,20,21,22,23,24] and websites of the Ministries of health, national statistics and national public health institutes of six key countries for which limited data were published i.e., France, Portugal, Norway, Switzerland, Denmark, and Finland.
During the abstract and title screening (selection step 1), studies were included based on relevant outcomes (i.e., HZ incidence in the high-risk population) and excluded based on population (i.e., not IC patients); study design (i.e., models, sample size smaller than 30, phase I, II and III trials); geography (i.e., country out of scope); and type of publication (i.e., letters, editorials, comments). Two researchers independently performed this step and discussed any discrepancies (N.V., H.V.). Fewer than 5% of the abstracts required review and discussion.
During full-text screening of articles selected in step 1, studies that answered the review question were included. Exclusion criteria related to populations (i.e., non-relevant high-risk populations, combined relevant and non-relevant high-risk populations without stratified data, unclear if secondary VZV infection only); country (i.e., combined relevant and non-relevant countries without country-specific data, country not stated); methods (i.e., no quantitative data or only data in figures, insufficient methodological details, insufficient methodological quality); and reporting (i.e., narrative review, no methods section). Two researchers independently checked the first 10% of full-text articles for relevancy (N.V., H.V.). There was agreement on all selections.
To ensure reproducibility, the study selection process was documented in an EndNote Library with the reasons for exclusion of full-text publications in an MS Excel table.
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Data Analysis
Data were extracted into an Excel database by one researcher (N.V.) and reviewed by another (H.V.). Standard evidence tables were used to extract data on: First author, publication year, journal; Country; Study design; Study period and setting; Study population (inclusion and exclusion criteria, sample size, age groups, gender, ethnicity, underlying high-risk conditions; Methodology (IC definition, HZ case detection, HZ case definition, type of patients and incidence denominator); HZ incidence (defined as incidence rate [incidence per 1000 person-years], cumulative incidence [incidence per 1000 persons], or relative incidence [number of cases as a percentage of study population]) by year, gender, age, ethnicity, high-risk population, and treatment option; Comments or quality issues from authors; and Quality assessment tool. The primary outcomes were HZ incidence rate and cumulative incidence, while the relative incidence was a secondary outcome.
The methodological quality of studies was assessed based on representativeness of the target population, validity of the HZ case definition, and use of a properly defined incidence denominator. Most of the included studies were surveillance studies, non-comparative studies, or comparative studies that are not cohort or case–control studies. As there are no formal validated checklists available for these study types, a previously-developed quality assessment tool was used to critically appraise and describe the methodological quality of incidence and prevalence studies. This tool was adapted further, in collaboration with an HZ expert, to focus specifically on HZ incidence studies [16] (see Supplemental file 2).
Feasibility of conducting a meta-analysis was assessed according to Cochrane criteria [17]. From an overview of studies that reported on the same outcome measure with a corresponding 95% confidence interval (95% CI), the comparability of the studies and similarity of the results was discussed to decide on the feasibility of a meta-analysis. As many included studies were non-comparative observational studies, the assessment mainly focused on comparability of study characteristics (i.e., setting, period, definition of HZ and high-risk disease) and of population characteristics (i.e., type of high-risk disease, age, gender, antiviral prophylaxis; or other medications).
Role of the Funding Source
GlaxoSmithKline Biologicals S.A. (VEO-000054) funded this literature review and all costs related to the development of the publication, including the journal’s Rapid Service Fee.
Results
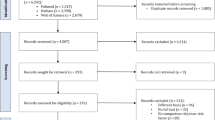
The database searches identified 1045 records (776 unique records after removing duplicates) for screening with an additional 79 references from the reference lists of systematic reviews identified. A total of 652 abstracts and 137 full-text reports (65 from database searches and 72 from additional references) were not eligible and were excluded, and it was not possible to retrieve seven full-text publications. Reasons for exclusion of full-text reports from the searches are described in Supplemental file 3. Overall, 59 studies were selected for inclusion in the systematic review (Fig. 1), from ten countries in Europe (Austria, France, Germany, Greece, Italy, the Netherlands, Spain, Sweden, Switzerland, and the United Kingdom). Baseline characteristics of the included studies can be found in Table S1 (Supplemental file 4). There were 26 studies reporting the primary outcomes of interest i.e., 24 reported HZ incidence rate [25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48], and two studies reported HZ cumulative incidence [49, 50] (Table 1). The remaining 33 studies reported secondary outcomes i.e., HZ relative incidence [51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83]. These mostly focused on the occurrence of different types of infection, including HZ, after a specific treatment or a transplant. Therefore, these secondary outcomes were not the main focus of this review and are reported in Table S2 (Supplemental file 4).
PRISMA flowchart. *Full-text article checked if eligibility not clear from abstract. **Includes studies combining relevant and non-relevant countries/IC populations without stratified data. HZ herpes zoster, IC immunocompromised, PRISMA Preferred Reporting Items for Systematic Reviews and Meta-analyses, SLR systematic literature review, VZV varicella zoster virus
Within the categories of high-risk populations presented in Table 1, there was variability in the reported HZ incidence across studies, partly due to different subgroups of patients or different immunosuppressive medication. The study findings are described in more detail by population and subgroup below, starting with the populations with the highest reported HZ incidence rates (per 1000 person-years). Subgroup comparisons within these populations were not statistically compared unless otherwise indicated. Some studies provided comparisons between IC and non-IC populations, and while the focus of this research was only on IC populations, comparative results are presented when available.
Solid Organ Transplantation
Seven studies [30, 34, 37, 38, 41, 47, 48] reported HZ incidence rates in the subgroup of solid organ transplant recipients, all studies focused on adult patients (≥ 18 years). The HZ incidence rate per 1000 person-years ranged from 12.1 in a mixed group of solid organ transplant patients [48] to 78.8 in kidney transplant patients [30].
A retrospective study (N = 1033) reported incidence rates by type of solid organ transplantation [34]. The highest incidence was found in patients with a lung transplant (38.8), followed by heart transplant (30.7), liver transplant (22.7), and kidney transplantation patients (14.5) [34]. Another retrospective study in lung transplant patients (N = 119) reported similar incidence rates (38.2 [47] vs. 38.8 [34]). A prospective study (N = 444) [30] and a retrospective study (N = 450) [38] in kidney transplant patients reported higher incidence rates (20.6 [38] and 78.8 [95% CI 54–104] [30]). All three studies in kidney transplant patients [30, 34, 38] included adult outpatients with HZ diagnosed based on clinical signs. In one of these studies, incidence was found to be higher in patients ≥ 60 years (43) versus < 60 years of age (16.7) [38]. Three studies [37, 41, 48] reported incidence rates in a group of combined solid organ transplant patients (i.e., ranging from 12.1 [48] to 14.5 [41] in transplant patients versus, for non-IC patients, 4.6 [95% CI 4.6–4.7] in Spain [37], 5.9 [95% CI 5.8–5.9] in Germany [41], and 6.2 [95% CI 6.1–6.3] in England [48]). Higher incidence rates were found in the older age categories (e.g., 17.0 in 60–69 years and 17.3 in ≥ 80 years versus 6.0 in 18–29 years of age in Spain [37], and 16.9 in ≥ 80 years versus 11.0 in 18–49 years of age in England [48]).
Stem Cell Transplantation
Three studies [37, 41, 48] reported HZ incidence rates in stem cell transplantation patients aged ≥ 18 years, ranging from 37.2 (95% CI 32.0–43.0) [41] in in- and outpatients in Germany receiving stem cell transplantation (including HSCT) to 56.1 (95% CI 48.9–64.0) [37] in HSCT patients in Spain. Incidence rates were significantly lower in non-IC patients (e.g., 5.9 [95% CI 5.8–5.9] in Germany [41], 4.6 [95% CI 4.6–4.7] in Spain [37], and 6.2 [95% CI 6.1–6.3] in England [48].)
Incidence rates reported peaked in 50–59 year-olds (69.2 vs. 5.5 in non-IC patients) in Spain [37] and 60–64 year-olds (60.3 vs. 6.9 in non-IC patients) in England [48]. Lower rates were reported in younger age groups (42.4 in 18–29 year-olds [37] and 34.1 in 18–49 year-olds [48], vs. 2.1–2.3 in non-IC patients [37, 48]), as well as in older age groups (52.0 in 70–79 year-olds [37] and 47.0 in 65–69 year-olds [48], vs. 8.6–9.3 in non-IC patients [37, 48]).
Hematologic Malignancy
Four studies [25, 37, 43, 48] reported HZ incidence rates in a mixed group of hematological malignancies [37, 48], in myelofibrosis (MF) [25], and chronic lymphocytic leukemia (CLL) [43].
The lowest incidence rate was reported in the Swedish Cancer Registry for CLL in- and outpatients (N = 8989), who had an 11.3 (95% CI 8.4–15.3) times greater risk of HZ versus controls (2.94 vs. 0.26) [43]. In a multinational study in MF patients (N = 462), HZ incidence was increased in ruxolitinib users versus non-ruxolitinib users (3) i.e., incidence varied in long-term (37), short-term (29), new (59) users and patients who switched to ruxolitinib during the study (43) [25]. In the mixed group of hematological malignancy patients in Spain [37] and England [48], the incidence rate in adults ≥ 18 years was 12.0 (95% CI 11.5–12.5) versus 4.6 (95% CI 4.6–4.7) in non-IC controls [37] and 15.2 (95% CI 14.5–16.0) [48] versus 6.2 (95% CI 6.1–6.3) in non-IC controls, and increased with age to 18.4 (95% CI 16.1–21.0) vs. 6.9 (95% CI 6.6–7.2) [48] in 60–64 year-olds, and to 20.1 (95% CI 18.4–21.9) vs. 9.3 (95% CI 9.2–9.4) [37] in 70–79 year-olds.
Rheumatic Disorders
Ten studies [26, 31, 37, 39,40,41,42, 44, 46, 48] reported the HZ incidence rates in patients with rheumatoid arthritis (RA), ranging from 0.41 in adult UK in- and outpatients using rituximab [40] to 21.5 in German outpatients of all ages treated with Janus kinase-inhibitors (JAK-inhibitors) [39]. There was heterogeneity across HZ case definitions used (clinical diagnosis versus MedDRA), study populations, and medication types. This heterogeneity might explain the broad range of HZ incidence rates.
Four studies reported the HZ incidence rate by type of medication (Table 2), with the high rates in patients treated with JAK-inhibitors (21.5) [39], infliximab (20.0) [31], etanercept and anti-TNF agents (both 16.0) [31], adalimumab (13.0) [31], B-cell-targeted therapies (10.3) [39] and infliximab/adalimumab (11.1) [44]. A second UK study [40] focusing on serious opportunistic infections (OIs) in RA patients starting on biologic therapies (mean age 56.7 years [SD 12.3]) reported that HZ was the most common OI with an overall incidence rate of 0.59 (based on 61 HZ cases, from 2001 to 2016) [40]. The considerably lower incidence rate in this study may be due to the inclusion of severe cases only, as the other UK study [31] identified 320 HZ cases using the same database (British Society for Rheumatology’s Biologics Register) over a shorter duration (2001–2009).
HZ incidence was compared in males versus females with RA, and found to be comparable (7.7 vs. 7.9) [44]. In a retrospective matched cohort study in Germany, HZ incidence in RA patients followed over 10 years appeared to be stable over time (2008: 10.0; 2018: 10.5) [26]. In a passive surveillance study in Germany, HZ incidence in RA versus polymyalgia rheumatica patients was comparable (16.2 vs. 15.8) [41].
Lupus
Three studies reported HZ incidence rates in adults aged ≥ 18 years with systemic lupus erythematosus (SLE) [37, 41, 48] and one with lupus erythematosus [41].
Incidence rates in SLE patients were 11.0 (95% CI 9.8–12.3) vs. 6.2 (95% CI 6.1–6.3) in non-IC patients in a matched cohort study in England [48], and 13.4 vs. 4.6 in non-IC patients in a retrospective study in Spain [37]. Higher rates were reported in older age groups (7.9–12.8 in < 70 years vs. 17.2–18.1 in ≥ 70 years (compared with non-IC patients, 2.1–8.6 in < 70 years and 11.0 in ≥ 70 years) [48]; and 8.4–9.8 in < 50 years vs. 17.2–21.8 in ≥ 50 years (compared with non-IC patients, 2.3–2.8 in < 50 years and 5.5–9.5 in ≥ 50 years) [37]. Comparable incidence rates were reported from a passive surveillance study in Germany, in patients with SLE versus lupus erythematosus (SLE 16.5 [95% CI 14.4–18.9] vs. lupus erythematosus 16.2 [95% CI 14.6–17.9]), compared with non-IC patients (5.9 [95% CI 5.8–5.9]) [41].
HIV/AIDS
Five studies in HIV patients [32, 33, 37, 41, 48] reported HZ incidence rates, ranging from 11.8 [48] in England to 13.0[41] in Germany among adults (≥ 18 years), compared with 5.9 (95% CI 5.8–5.9) in non-IC patients in Germany [41].
Three studies reported incidence by age groups [33, 37, 48]. A higher incidence rate was reported among patients ≥ 40 years (13.4–13.5) versus younger age groups (4.8–12.0) in a prospective comparative study in Germany, with the risk of HZ remaining significantly higher than in the general population (incidence of 1.5–3.3 reported in Western countries) [33]. Incidence rates were 12.9 (95% CI 12.0–14.0) versus 4.6 (95% CI 4.6–4.7) in non-IC patients in a retrospective study in Spain [37], and 11.8 (95% CI 9.5–14.4) vs. 6.2 (95% CI 6.1–6.3) in non-IC patients in a matched cohort study in England [48]. In a passive surveillance study in France [32], the incidence rate was found to be lower in the period 2009–2011 versus 1992–1996 (6.3 vs. 29.5), while remaining significantly higher than incidence in the general population (2.7 [95% CI 2.6–2.9]) [32].
In a passive surveillance study in HIV and AIDS patients in Spain, incidence was higher in females versus males (15.2 vs. 11.6) [29].
Chronic Respiratory Diseases (COPD and Asthma)
Five studies [26,27,28,29, 36] reported HZ incidence rates in asthma and COPD patients, ranging from 4.7 in adult asthma patients treated with inhaled corticosteroids [27] to 11.2 (95% CI 9.9–12.5) in elderly asthma patients [28] and from 7.4 in COPD patients aged 50–59 years using no inhaled corticosteroids to 14.2 in COPD patients ≥ 80 years on inhaled corticosteroids [36]. In studies reporting HZ incidence rates in both asthma and COPD patients, rates were higher in COPD patients i.e., 6.9 vs. 11.4 (passive surveillance study in Spain) [29] and 5.9–7.2 vs. 8.2–8.7 (range of annual rates from German retrospective matched cohort study over 10 years [26]).
In adult asthma patients, the HZ incidence rate was 1.2–1.4 times higher than in controls [26, 28, 29], and up to 1.5 times higher in asthma patients on oral versus inhaled corticosteroids [27]. The HZ incidence rate in Spain (N = 4476, passive surveillance, primary care data 2009–2012) was 6.9 for asthma patients (adjusted incidence rate ratio [IRR] 1.3 [95% CI 1.3–1.4] versus controls) and was higher in women versus men (8.1 vs. 4.9) [29]. A similar incidence rate of 7.2 was reported in Germany (retrospective matched cohort, hospital data 2018) versus 5.3 in matched controls (adjusted odds ratio [aOR] 1.2 [95% CI 1.2–1.3]) [26]. The incidence rate was higher in elderly asthma patients in England (primary care and hospital data 2013–2016): 11.2 (95% CI 9.9–12.5) versus 9.3 (95% CI 8.8–9.9) in general population controls [28]. A study in the UK (N = 4432, primary care and hospital data 2000–2015) found that HZ incidence rates were higher for asthma patients who have used oral corticosteroids (6.1, adjusted IRR 1.3 [95% CI 1.2–1.4]) or are using oral corticosteroids (7.2, adjusted IRR 1.5 [95% CI 1.4–1.7]) versus those on inhaled corticosteroids alone (4.7) [27].
In adult COPD patients, the HZ incidence rate was 1.1–1.5 times higher [26, 29, 36], and up to 1.6 times higher for COPD patients on inhaled corticosteroids [36], versus controls without COPD. The HZ incidence rate in Spain (N = 2894, passive surveillance, primary care data 2009–2012) was 11.4 for COPD patients (adjusted IRR 1.3 [95% CI 1.2–1.3] in men and 1.2 [95% CI 1.2–1.3] in women versus controls) and was higher in women versus men (12.9 vs. 10.8) [29]. HZ incidence rate was also higher for COPD patients in Germany versus controls (8.7 vs. 7.3, OR 1.1 [95% CI 1.0–1.1] based on hospital data for 2018 (retrospective matched cohort) [26]. In Spain (N = 5793, passive surveillance, primary care and hospital data 2009–2014), HZ incidence rates were higher for COPD patients aged ≥ 50 years (adjusted relative risk [aRR] 1.5 [95% CI 1.4–1.5], and even higher for COPD patients on inhaled corticosteroids (aRR 1.6 [95% CI 1.5–1.7]) versus patients without COPD [36]. Incidence rates for non-COPD controls, COPD patients not on inhaled corticosteroids, and COPD patients on corticosteroids, respectively, increased with age from 5.3, 7.4 and 10.6 (aged 50–59 years) to 8.6, 12.8 and 14.2 (aged ≥ 80 years), respectively [36].
One Italian study (N = 1553, hospital data 2013–2015) reported 2-year HZ cumulative incidence per 1000 persons (6.8) in COPD patients aged ≥ 50 years versus 4.7 in patients not at risk of HZ (p < 0.01) [50]. In this study, patients at risk of HZ were defined according to the Italian National Vaccine Prevention Plan (2017–2019) i.e., cardiovascular disease, COPD, diabetes, immunosuppression [50].
Solid Organ Malignancy
Three studies [29, 37, 48] reported HZ incidence rates, ranging from 8.8 [48] to 11.0 [37], in patients aged ≥ 18 years with various solid organ malignancies versus 4.6–6.2 in non-IC controls. Higher incidence rates [95% CI] were reported in older age groups versus non-IC controls (among patients aged 50–59 years: 10.2 [9.7–10.9] vs. 5.5 [5.4–5.6] in Spain [37] and 6.8 [6.4–7.3] vs. 4.9 [4.7–5.1] in England [48]; among patients aged ≥ 80 years: 12.0 [11.4–12.6] vs. 9.5 [9.4–9.7] in Spain [37] and 11.6 [11.1–12.2] vs. 11.0 [10.6–11.4] in England [48]), and in females versus males (10.8 vs. 9.0) [29].
Inflammatory Bowel Diseases
Three studies [37, 41, 48] reported HZ incidence rates in adults ≥ 18 years with IBD [37, 48], Crohn’s disease [41] and ulcerative colitis (UC) [41] that were 1.1–1.8 times higher than in non-IC patients.
In Spain, IBD patients ≥ 18 years (N = 28,700, hospital and primary care data 2009–2014) had significantly higher HZ incidence rates versus non-IC patients (8.3 [95% CI 7.8–8.8] vs. 4.6 [95% CI 4.6–4.7]). Incidence rates increased with age from 4.8 (95% CI 3.7–6.3) versus controls 2.3 (95% CI 2.2–2.3) in younger adults aged 18–29 years, to 16.2 (95% CI 13.2–19.7) versus controls 9.5 (95% CI 9.4–9.7) in older adults aged ≥ 80 years [37].
In a matched cohort study in England (N = 31,884, hospital and primary care data 2000–2012), HZ incidence rate was 7.0 (95% CI 6.6–7.4) in IBD patients ≥ 18 years versus 6.21 (95% CI 6.1–6.3) in controls. Incidence rates increased with age from 4.0 (95% CI 3.6–4.5) versus controls 2.1 (95% CI 2.0–2.2) in patients aged 18–49 years, to 13.9 (95% CI 11.6–16.4) versus controls 11.0 (95% CI 10.6–11.4) in older adults aged ≥ 80 years [48].
From German claims data (hospital data 2012), HZ incidence rates in adults ≥ 18 years were 10.8 (95% CI 10.2–11.4) for UC and 10.7 (95% CI 9.9–11.4) for Crohn’s disease versus 5.9 (95% CI 5.8–5.9) for non-IC patients [41].
Type 1 and Type 2 Diabetes Mellitus (T1DM, T2DM)
Three studies [26, 29, 35, 37] reported HZ incidence rates in patients with DM, ranging from 4.3–6.3 in T1DM to 7.0–7.9 in T2DM (between 2008 and 2018) [26], and ranging from 6.7 in DM patients (type not specified) aged 50–59 years old to 10.6 in those aged ≥ 80 years [35].
A retrospective matched cohort study in Germany [26] reported HZ incidence rates in T1DM and T2DM per year from hospital data between 2008 and 2018: incidence rates ranged from 4.3 to 6.3 in patients with T1DM versus 4.4 to 5.0 in controls, and from 7.0 to 7.9 in patients with T2DM versus 6.7–7.5 in controls. In 2018, HZ incidence was higher in T1DM (5.8 vs. 4.6, adjusted OR 1.01 [95% CI 0.98–1.04]) and T2DM (7.9 vs. 7.5, adjusted OR 0.99 [95% CI 0.91–1.08]) versus controls [26].
Two passive surveillance studies in DM patients in Spain included primary care data and reported significantly higher HZ incidence in DM patients versus controls (from hospital and primary care data in Valencia [N = 397,940 aged ≥ 50 years[35], and N = 491,210 aged ≥ 18 years [37]] and from primary care data in Madrid [N = 284,895] [29]). Incidence rates in DM adults ≥ 18 years were significantly higher than controls without DM (i.e., 9.4, adjusted IRR 1.13 [95% CI 1.09–1.17] in men and 1.04 [95% CI 1.01–1.08] in women [29]). Similarly, in DM adults ≥ 50 years, incidence rates were 9.3 (95% CI 9.1–9.4) versus 6.8 (95% CI 6.8–6.9) in controls (aRR 1.20 [95% CI 1.17–1.22]), and increased with age from 6.7 (50–59 years), to 9.1 (60–69 years), to 10.1 (70–79 years) and to 10.6 (≥ 80 years) [35]. HZ incidence was significantly higher in women versus men (aRR 1.36 [95% CI 1.33–1.38] [35]), and in older age groups versus patients aged 50–59 years (aRR for 60–69 years 1.38 [95% CI 1.35–1.41], 70–79 years 1.53 [95% CI 1.49–1.57] and ≥ 80 years 1.50 [95% CI 1.46–1.54]) [35].
Two studies [49, 50] reported HZ cumulative incidence per 1000 persons in DM patients (type not specified). Two-year HZ incidence in DM patients ≥ 50 years (N = 591,765, hospital data 2013–2015) was 5.6 versus 4.7 (p < 0.01) in controls not at risk of HZ, in Italy (at risk of HZ based on Italian National Vaccine Prevention Plan) [50]. In Spain (N = 26,793, primary care data 2006), HZ incidence in DM patients ≥ 30 years was also significantly higher versus controls i.e., overall incidence 15.3 (aRR 2.1 [95% CI 1.9–2.4]). Incidence increased significantly with age versus patients aged 30–44 years (7.0); 45–59 years (9.0, aRR 2.3 [95% CI 2.0–2.7]); 60–74 years (14.7, aRR 4.0 [95% CI 3.5–4.6]; ≥ 75 years (21.3, aRR 4.6 [95% CI 4.0–5.4]) and in women versus men (18.7 vs. 12.4, aRR 1.3 [95% CI 1.2–1.4]) [49].
Depression
A retrospective matched cohort study reported the HZ incidence rate in adults in Germany with depression over a 10-year timeframe versus non-IC controls; incidence was 7.2 vs. 5.5 [2008] and 7.6 vs. 6.2 [2018]) [26]. The adjusted OR (all ages) was 1.3 (95% CI 1.2–1.3) in 2008 and 1.2 (95% CI 1.1–1.2) in 2018; with higher ORs seen in adults aged 50–59 years (i.e., 1.4 [1.3–1.5] in 2008 and 1.3 [1.2–1.4] in 2018) [26].
Multiple Sclerosis
Two studies [37, 48] reported HZ incidence rates in MS patients aged ≥ 18 years i.e., 5.7 (95% CI 5.1–6.4) in a matched cohort study in England [48], and 6.3 (95% CI 5.3–7.5) in a passive surveillance study in Valencia, Spain [37]. Incidence rates increased with age from 4.1–7.2 in < 60 years (vs. 2.2–5.5 in non-IC patients) to 11.0–12.3 in ≥ 60 years (vs. 8.1–9.5 in non-IC patients) in Spain[37]; and from 3.7–6.0 in < 60 years (vs. 2.1–4.9 in non-IC patients) to 6.9–10.2 in ≥ 60 years (vs. 6.9–11.0 in non-IC patients) in England [48].
Psoriasis
Four studies [37, 41, 45, 48] reported HZ incidence rates in adults ≥ 18 years with psoriasis, ranging from 5.3 (95% CI 5.2–5.5) in a matched cohort study in England [48] to 6.1 (95% CI 5.9–6.3) in a passive surveillance study in Valencia, Spain [37]. In these two studies, incidence rates increased with age from 3.0–3.7 in < 50 years to 7.6–12.4 in ≥ 50 years (compared with non-IC patients, from 2.3–2.8 to 5.5–9.5) in Spain[37], and from 2.6–5.5 in < 60 years to 7.4–12.2 in ≥ 60 years (compared with non-IC patients, from 2.1–4.9 to 6.9–11.0) in England [48]).
The incidence rate was higher in patients with moderate to severe psoriasis (6.5 [95% CI 5.9–7.1]) versus mild psoriasis (5.4 [95% CI 5.2–5.5]) in a UK prospective matched cohort study (N = 199,700) [45].
Group of IC Patients
Two studies [28, 41] reported HZ incidence rates in grouped IC populations.
In a passive surveillance study in Germany [41], the grouped HZ incidence rate was 11.3 (95% CI 11.1–11.5) in 2006 and 11.5 (95% CI 11.4–11.6) in 2012, among IC patients with HIV, malignant neoplasms, organ transplantation, stem cell transplantation, SLE, UC, Crohn’s disease, lupus erythematous, and RA. HZ incidence in non-IC patients was 5.9 (95% CI 5.8–5.9) [41].
In a UK retrospective comparative study, the HZ incidence rate in older IC patients (born in 1934–1946) with immunocompromising conditions was 15.5 (12.2–18.8) versus 14.2 (10.9–17.6) in patients immunosuppressed due to medication [28]. HZ incidence was 9.3 (95% CI 8.8–9.9) in the general population. Conditions included hematological malignancy, HIV/AIDS, cellular immune deficiencies or HSCT. Immunosuppressive or immunomodulating therapies included chemotherapy, radiotherapy, solid organ transplantation, immunosuppressive therapy, biological therapy, short-term high-dose corticosteroids, long-term lower-dose corticosteroids, and non-biological oral immune-modulating drugs.
One study [50] reported an HZ cumulative incidence of 3.5, in patients immunosuppressed due to medication and/or IC conditions.
Meta-analysis Feasibility
The feasibility of conducting a meta-analysis was explored for the 11 studies that reported incidence rates with 95% CIs. These studies included 11 different subgroup populations (i.e., chronic respiratory diseases, hematological malignancy, HIV/AIDS, IBD, SLE, RA, MS, psoriasis, solid organ malignancy, solid organ transplant, and stem cell transplantation). However, data across different subgroups could not be meaningfully pooled. There were at least two studies with data for each subgroup population, however, the number of studies was considered too few for the meta-analysis to add value. Moreover, for subgroups with a somewhat larger number of studies, the criterium of comparability of study/population characteristics was not met (see Appendix Table 3).
There was great variability in the incidence rates reported across populations at increased risk of HZ and across subgroups, due to heterogeneity in study designs, populations and HZ case definitions, or as shown for RA, due to different immunosuppressive medications (Table 3). For study quality, 13/26 studies were of sufficient quality regarding representativeness of the target population, 14/26 regarding validity of HZ case definition, and 17/26 had a properly defined denominator. Overall, 19% of studies met all three quality criteria, 39% met two criteria and 65% met one criterion.
Discussion
This systematic review of HZ incidence in populations at increased risk of HZ, in the EU/EEA, Switzerland and the UK, included a broad range of conditions. The review included 24 studies reporting incidence rates (per 1000 person-years) and two studies reporting cumulative incidence (per 1000 persons), across 14 populations. Thirty-three studies were also identified reporting relative incidence (percentage of HZ cases in the study population) (see Supplemental file).
The highest incidence rate was reported for solid organ transplantation (12.1–78.8) and stem cell transplantation (37.2–56.1); then hematological malignancies (2.9–32.0); rheumatic disorders (0.41–21.5); lupus (11.0–16.5); IC mixed population (11.3–15.5); HIV/AIDS (11.8–13.0); chronic respiratory diseases (4.7–11.4); solid organ malignancies (8.8–11.0); inflammatory bowel diseases (7.0–10.8); diabetes mellitus (4.3–9.4); depression (7.2–7.6); multiple sclerosis (5.7–6.3); and psoriasis (5.3–6.1).
The subgroups with the highest reported incidence rates (of 20.0 or higher), were kidney transplant (14.5–78.8); HSCT (41.7–56.1); lung transplant (38.2–38.8); myelofibrosis (12.0–32.0); heart transplant (30.7); liver transplant (22.7) and RA (0.41–21.5).
In many populations at increased risk of HZ, a higher incidence of HZ was reported in older versus younger age groups (e.g., solid organ transplantation, hematological malignancy, lupus, solid organ malignancy, IBD, DM, MS, and psoriasis). In HSCT patients, however, the incidence was highest between 50 and 64 years of age and lower in younger and older age groups. Mixed results were reported across studies for HIV and risk of HZ by age group.
Reported HZ incidence rates were higher for females versus males with asthma, COPD and DM; for patients with T2DM versus T1DM; and for moderate to severe psoriasis versus mild psoriasis. Reported HZ incidence rates were also higher in 2018 versus 2008 for asthma and COPD patients, for DM and depression patients, but remained stable for RA patients. Only one study reported HZ incidence rates in populations with an IC condition (15.5) versus immunosuppressed due to medication (14.2).
The recent systematic review focusing on IC populations in the US [2] also found that the majority of studies reported HZ incidence as a percentage of cases out of the study population, with a minority reporting incidence rates. Reported incidence rates in this review also varied widely across and within populations, with the highest rates (based on figure) seen for hematopoietic cell transplants (HCT) (40–90) followed by hematological malignancies (30–70), solid organ transplantation (20–30), solid tumor malignancies (15–25) and HIV (10–20). The lack of, or a short duration of, antiviral prophylaxis was associated with higher HZ incidence in this review, following HCT. Higher incidence rates were also reported for 60–64 year-olds versus 18–49 year-olds with HCT, SOT and cancer [2]. Similarly, the recent systematic review of HZ incidence in Latin America reported rates varying from 6.4 to 36.5 in immunosuppressed populations, with age over 50 years old presenting an important risk factor [12].
The review had some limitations. Most studies used a retrospective design, which could be limited by incomplete or low-quality data. Databases do not capture individuals who do not seek care, are uninsured, or in some cases, institutionalized, potentially underestimating HZ incidence in the oldest age groups. Studies did not always clearly specify how HZ cases or IC disease was defined or whether antiviral prophylaxis was used. Some studies used antiviral prescriptions to define HZ. Mild cases may not receive treatment, resulting in underestimation of the HZ incidence, while antivirals prescribed for another disease than HZ may result in overestimation of HZ incidence. Methodological variations across studies made comparisons difficult e.g., settings ranged from single center to national surveillance (with sample sizes ranging from 33 to 1,481,095) affecting generalizability and comparability of results; and study periods ranged from 1987 to 1998 for the oldest data to the year 2020. Statistical comparisons were often lacking, and only 11 studies reported incidence rates with 95% CI. Data were limited for some countries (e.g., Eastern European countries) and for some conditions (e.g., depression).
Conclusions
In conclusion, the results demonstrate that HZ incidence rates in Europe vary across populations at increased risk of HZ, with high rates (over 20 per 1000 person-years) reported for patients with solid organ transplants, stem cell transplants, cancer and rheumatoid arthritis, and older age is an important risk factor. To better inform vaccine policy decision makers, it is important for future studies to stratify data according to population and subgroup, age group, sex, severity of disease, type of medication, and timeframe of the study, and to provide statistical comparisons of these stratifications. This will allow for meaningful comparisons to be made across studies, and for data to be pooled in a meta-analysis.
Data Availability
All of the data used for the systematic review is either publicly available (published studies) or provided in the manuscript and Supplementary materials.
References
Werner RN, Nikkels AF, Marinović B, et al. European consensus-based (S2k) guideline on the management of herpes zoster – guided by the European dermatology forum (EDF) in cooperation with the European academy of dermatology and venereology (EADV), part 1: diagnosis. J Eur Acad Dermatol Venereol. 2017;31(1):9–19. https://doi.org/10.1111/jdv.13995.
McKay SL, Guo A, Pergam SA, Dooling K. Herpes zoster risk in immunocompromised adults in the United States: a systematic review. Clin Infect Dis. 2020;71(7):e125–34. https://doi.org/10.1093/cid/ciz1090.
Harbecke R, Cohen JI, Oxman MN. Herpes zoster vaccines. J Infect Dis. 2021;224(12 Suppl 2):S429–42. https://doi.org/10.1093/infdis/jiab387.
Parikh R, Singer D, Chmielewski-Yee E, Dessart C. Effectiveness and safety of recombinant zoster vaccine: a review of real-world evidence. Hum Vaccin Immunother. 2023;19(3):2263979. https://doi.org/10.1080/21645515.2023.2263979.
Volpi A, Boccalini S, Dari S, et al. The potential public health impact of herpes zoster vaccination in the 65 years of age cohort in Italy. Hum Vaccin Immunother. 2020;16(2):327–34. https://doi.org/10.1080/21645515.2019.1657753.
European Centre for Disease Prevention and Control (ECDC). Vaccine Scheduler. https://vaccine-schedule.ecdc.europa.eu/Scheduler/ByDisease?SelectedDiseaseId=51&SelectedCountryIdByDisease=-1. Accessed Oct 10 2022.
CDC. Shingles overview. https://www.cdc.gov/shingles/about/index.html. Accessed Sept 10 2022.
Pinchinat S, Cebrián-Cuenca AM, Bricout H, Johnson RW. Similar herpes zoster incidence across Europe: results from a systematic literature review. BMC Infect Dis. 2013;13:170. https://doi.org/10.1186/1471-2334-13-170.
Curran D, Callegaro A, Fahrbach K, et al. Meta-regression of herpes zoster incidence worldwide. Infect Dis Ther. 2022;11(1):389–403. https://doi.org/10.1007/s40121-021-00567-8.
Varghese L, Standaert B, Olivieri A, Curran D. The temporal impact of aging on the burden of herpes zoster. BMC Geriatr. 2017;17(1):1–7.
Patil A, Goldust M, Wollina U. Herpes zoster: a review of clinical manifestations and management. Viruses. 2022;14(2):192. https://doi.org/10.3390/v14020192.
Bardach AE, Palermo C, Alconada T, et al. Herpes zoster epidemiology in Latin America: a systematic review and meta-analysis. PLoS ONE. 2021;16(8): e0255877. https://doi.org/10.1371/journal.pone.0255877.
Forbes HJ, Thomas SL, Smeeth L, et al. A systematic review and meta-analysis of risk factors for postherpetic neuralgia. Pain. 2016;157(1):30–54. https://doi.org/10.1097/j.pain.0000000000000307.
Kawai K, Gebremeskel BG, Acosta CJ. Systematic review of incidence and complications of herpes zoster: towards a global perspective. BMJ Open. 2014;4(6): e004833. https://doi.org/10.1136/bmjopen-2014-004833.
Bricout H, Haugh M, Olatunde O, Prieto RG. Herpes zoster-associated mortality in Europe: a systematic review. BMC Public Health. 2015;15:466. https://doi.org/10.1186/s12889-015-1753-y.
van Oorschot D, Vroling H, Bunge E, Diaz-Decaro J, Curran D, Yawn B. A systematic literature review of herpes zoster incidence worldwide. Hum Vaccin Immunother. 2021;17(6):1714–32.
Higgins JP, Thomas J, Chandler J, et al. Cochrane handbook for systematic reviews of interventions v6.3. https://training.cochrane.org/handbook/current. Accessed Apr 19 2023.
Preferred reporting items for systematic reviews and meta-analyses (PRISMA). http://prisma-statement.org/. Accessed Apr 19 2023.
European Centre for Disease Prevention and Control (ECDC). https://ecdc.europa.eu/en/home. Accessed Oct 4 2022.
European Commission (EC). https://ec.europa.eu/commission/index_en. Accessed Oct 4 2022.
EuroSurveillance. https://www.eurosurveillance.org/. Accessed Oct 4 2022.
World Health Organization (WHO). https://www.who.int/. Accessed Oct 4 2022.
EuroStat. https://ec.europa.eu/eurostat. Accessed Oct 4 2022.
United Nations Statistics Division. https://unstats.un.org/home/. Accessed Oct 4 2022.
Barraco F, Greil R, Herbrecht R, et al. Real-world non-interventional long-term post-authorisation safety study of ruxolitinib in myelofibrosis. Br J Haematol. 2020;191(5):764–74. https://doi.org/10.1111/bjh.16729.
Batram M, Witte J, Schwarz M, et al. Burden of herpes zoster in adult patients with underlying conditions: analysis of German claims data, 2007–2018. Dermatol Ther (Heidelb). 2021;11(3):1009–26. https://doi.org/10.1007/s13555-021-00535-7.
Bloechliger M, Reinau D, Spoendlin J, et al. Adverse events profile of oral corticosteroids among asthma patients in the UK: cohort study with a nested case-control analysis. Respir Res. 2018;19(1):75. https://doi.org/10.1186/s12931-018-0742-y.
Bollaerts K, Alexandridou M, Verstraeten T. Risk factors for modified vaccine effectiveness of the live attenuated zoster vaccine among the elderly in England. Vaccine X. 2019;1: 100007. https://doi.org/10.1016/j.jvacx.2019.100007.
Esteban-Vasallo MD, Domínguez-Berjón MF, Gil-Prieto R, Astray-Mochales J, Gil de Miguel A. Sociodemographic characteristics and chronic medical conditions as risk factors for herpes zoster: a population-based study from primary care in Madrid (Spain). Hum Vaccin Immunother. 2014;10(6):1650–60. https://doi.org/10.4161/hv.28620.
Fernández-Ruiz M, Origüen J, Lora D, et al. Herpes zoster in kidney transplant recipients: protective effect of anti-cytomegalovirus prophylaxis and natural killer cell count: a single-center cohort study. Transpl Int. 2018;31(2):187–97. https://doi.org/10.1111/tri.13076.
Galloway JB, Mercer LK, Moseley A, et al. Risk of skin and soft tissue infections (including shingles) in patients exposed to anti-tumour necrosis factor therapy: results from the British Society for rheumatology biologics register. Ann Rheum Dis. 2013;72(2):229–34. https://doi.org/10.1136/annrheumdis-2011-201108.
Grabar S, Tattevin P, Selinger-Leneman H, et al. Incidence of herpes zoster in HIV-infected adults in the combined antiretroviral therapy era: results from the FHDH-ANRS CO4 cohort. Clin Infect Dis. 2015;60(8):1269–77. https://doi.org/10.1093/cid/ciu1161.
Jansen K, Haastert B, Michalik C, et al. Incidence and risk factors of herpes zoster among HIV-positive patients in the German competence network for HIV/AIDS (KompNet): a cohort study analysis. BMC Infect Dis. 2013;13:372. https://doi.org/10.1186/1471-2334-13-372.
Kho MML, Roest S, Bovée DM, et al. Herpes zoster in solid organ transplantation: incidence and risk factors. Front Immunol. 2021;12: 645718. https://doi.org/10.3389/fimmu.2021.645718.
Muñoz-Quiles C, López-Lacort M, Ampudia-Blasco FJ, Díez-Domingo J. Risk and impact of herpes zoster on patients with diabetes: a population-based study, 2009–2014. Hum Vaccin Immunother. 2017;13(11):2606–11. https://doi.org/10.1080/21645515.2017.1368600.
Muñoz-Quiles C, López-Lacort M, Díez-Domingo J. Risk and impact of herpes zoster among COPD patients: a population-based study, 2009–2014. BMC Infect Dis. 2018;18(1):203. https://doi.org/10.1186/s12879-018-3121-x.
Muñoz-Quiles C, López-Lacort M, Díez-Domingo J, Orrico-Sánchez A. Herpes zoster risk and burden of disease in immunocompromised populations: a population-based study using health system integrated databases, 2009–2014. BMC Infect Dis. 2020;20(1):905. https://doi.org/10.1186/s12879-020-05648-6.
Pavlopoulou ID, Poulopoulou S, Melexopoulou C, Papazaharia I, Zavos G, Boletis IN. Incidence and risk factors of herpes zoster among adult renal transplant recipients receiving universal antiviral prophylaxis. BMC Infect Dis. 2015;15:285. https://doi.org/10.1186/s12879-015-1038-1.
Redeker I, Albrecht K, Kekow J, et al. Risk of herpes zoster (shingles) in patients with rheumatoid arthritis under biologic, targeted synthetic and conventional synthetic DMARD treatment: data from the German RABBIT register. Ann Rheum Dis. 2021;81(1):41–7. https://doi.org/10.1136/annrheumdis-2021-220651.
Rutherford AI, Patarata E, Subesinghe S, Hyrich KL, Galloway JB. Opportunistic infections in rheumatoid arthritis patients exposed to biologic therapy: results from the British society for rheumatology biologics register for rheumatoid arthritis. Rheumatology (UK). 2018;57(6):997–1001. https://doi.org/10.1093/rheumatology/key023.
Schröder C, Enders D, Schink T, Riedel O. Incidence of herpes zoster amongst adults varies by severity of immunosuppression. J Infect. 2017;75(3):207–15. https://doi.org/10.1016/j.jinf.2017.06.010.
Smitten AL, Choi HK, Hochberg MC, et al. The risk of herpes zoster in patients with rheumatoid arthritis in the United States and the United Kingdom. Arthritis Rheum. 2007;57(8):1431–8. https://doi.org/10.1002/art.23112.
Steingrímsson V, Gíslason GK, Þorsteinsdóttir S, et al. A nationwide study on inpatient opportunistic infections in patients with chronic lymphocytic leukemia in the pre-ibrutinib era. Eur J Haematol. 2021;106(3):346–53. https://doi.org/10.1111/ejh.13553.
Strangfeld A, Listing J, Herzer P, et al. Risk of herpes zoster in patients with rheumatoid arthritis treated with anti-TNF-alpha agents. JAMA. 2009;301(7):737–44. https://doi.org/10.1001/jama.2009.146.
Takeshita J, Shin DB, Ogdie A, Gelfand JM. Risk of serious infection, opportunistic infection, and herpes zoster among patients with psoriasis in the United Kingdom. J Invest Dermatol. 2018;138(8):1726–35. https://doi.org/10.1016/j.jid.2018.01.039.
Thomas K, Lazarini A, Kaltsonoudis E, et al. Incidence, risk factors and validation of the RABBIT score for serious infections in a cohort of 1557 patients with rheumatoid arthritis. Rheumatology (UK). 2021;60(5):2223–30. https://doi.org/10.1093/rheumatology/keaa557.
van Besouw NM, van Hal PT, Zuijderwijk JM, et al. Herpes zoster after lung transplantation boosts varicella zoster virus-specific adaptive immune responses. J Heart Lung Transplant. 2016;35(12):1435–42. https://doi.org/10.1016/j.healun.2016.04.009.
Yanni EA, Ferreira G, Guennec M, et al. Burden of herpes zoster in 16 selected immunocompromised populations in England: a cohort study in the clinical practice research datalink 2000–2012. BMJ Open. 2018;8(6): e020528. https://doi.org/10.1136/bmjopen-2017-020528.
Aldaz P, Díaz JA, Loayssa JR, Dronda MJ, Oscáriz M, Castilla J. Herpes zoster incidence in diabetic patients. An Sist Sanit Navar. 2013;36(1):57–62. https://doi.org/10.4321/s1137-66272013000100006.
Calabria S, Ronconi G, Dondi L, et al. Patterns of prescription, hospitalizations and costs of herpes zoster in patients at risk, from a large Italian claims database. Glob Reg Health Technol Assess. 2020;7(1):66–71. https://doi.org/10.33393/grhta.2020.2026.
Baronaite Hansen R, Jacobsen S. Infections increase risk of arterial and venous thromboses in Danish patients with systemic lupus erythematosus: 5102 patient-years of follow up. J Rheumatol. 2014;41(9):1817–22. https://doi.org/10.3899/jrheum.131399.
Biemans VB, Sleutjes JA, De Vries AC, et al. Tofacitinib for ulcerative colitis: results of the prospective Dutch Initiative on Crohn and Colitis (ICC) registry. Aliment Pharmacol Ther. 2020;51(9):880–8.
Blaizot R, Ouattara E, Fauconneau A, Beylot-Barry M, Pham-Ledard A. Infectious events and associated risk factors in mycosis fungoides/Sézary syndrome: a retrospective cohort study. Br J Dermatol. 2018;179(6):1322–8. https://doi.org/10.1111/bjd.17073.
Blennow O, Fjaertoft G, Winiarski J, Ljungman P, Mattsson J, Remberger M. Varicella-zoster reactivation after allogeneic stem cell transplantation without routine prophylaxis–the incidence remains high. Biol Blood Marrow Transplant. 2014;20(10):1646–9. https://doi.org/10.1016/j.bbmt.2014.06.002.
Chaparro M, Garre A, Mesonero F, et al. Tofacitinib in ulcerative colitis: real-world evidence from the ENEIDA registry. J Crohns Colitis. 2021;15(1):35–42.
Danhof S, Strifler S, Hose D, et al. Clinical and biological characteristics of myeloma patients influence response to elotuzumab combination therapy. J Cancer Res Clin Oncol. 2019;145(3):561–71. https://doi.org/10.1007/s00432-018-2807-1.
Daudén E, Carretero G, Rivera R, et al. Long-term safety of nine systemic medications for psoriasis: a cohort study using the Spanish registry of adverse events for biological therapy in dermatological diseases (BIOBADADERM) registry. J Am Acad Dermatol. 2020;83(1):139–50. https://doi.org/10.1016/j.jaad.2020.03.033.
Dogliotti I, Ragaini S, Vassallo F, et al. Real life use of bendamustine in elderly patients with lymphoid neoplasia. J Pers Med. 2021;11(4):249. https://doi.org/10.3390/jpm11040249.
Favalli EG, Desiati F, Atzeni F, et al. Serious infections during anti-TNFα treatment in rheumatoid arthritis patients. Autoimmun Rev. 2009;8(3):266–73. https://doi.org/10.1016/j.autrev.2008.11.002.
Formicone F, Fargnoli MC, Pisani F, Rascente M, Famulari A, Peris K. Cutaneous manifestations in Italian kidney transplant recipients. Transplant Proc. 2005;37(6):2527–8. https://doi.org/10.1016/j.transproceed.2005.06.067.
Garcia-Vidal C, Rodríguez-Fernández S, Teijón S, et al. Risk factors for opportunistic infections in infliximab-treated patients: the importance of screening in prevention. Eur J Clin Microbiol Infect Dis. 2009;28(4):331–7. https://doi.org/10.1007/s10096-008-0628-x.
Heider U, Rademacher J, Kaiser M, Kleeberg L, Von Metzler I, Sezer O. Decrease in CD4+ T-Cell counts in patients with multiple myeloma treated with bortezomib. Clin Lymphoma Myeloma. 2010;10(2):134–7. https://doi.org/10.3816/CLML.2010.n.019.
Hellgren J, Risedal A, Källén K. Rituximab in multiple sclerosis at general hospital level. Acta Neurol Scand. 2020;141(6):491–9. https://doi.org/10.1111/ane.13225.
Herrero JI, Quiroga J, Sangro B, et al. Herpes zoster after liver transplantation: incidence, risk factors, and complications. Liver Transpl. 2004;10(9):1140–3. https://doi.org/10.1002/lt.20219.
Honap S, Chee D, Chapman TP, et al. Real-world effectiveness of tofacitinib for moderate to severe ulcerative colitis: a multicentre UK experience. J Crohns Colitis. 2020;14(10):1385–93.
Kaden J, Völp A, Wesslau C. High graft protection and low incidences of infections, malignancies and other adverse effects with intra-operative high dose ATG-induction: a single centre cohort study of 760 cases. Ann Transplant. 2013;18:9–22. https://doi.org/10.12659/aot.883792.
Kamber C, Zimmerli S, Suter-Riniker F, et al. Varicella zoster virus reactivation after autologous SCT is a frequent event and associated with favorable outcome in myeloma patients. Bone Marrow Transplant. 2015;50(4):573–8. https://doi.org/10.1038/bmt.2014.290.
Lenti MV, Levison S, Eliadou E, et al. A real-world, long-term experience on effectiveness and safety of vedolizumab in adult patients with inflammatory bowel disease: the cross Pennine study. Dig Liver Dis. 2018;50(12):1299–304. https://doi.org/10.1016/j.dld.2018.07.007.
Leon L, Peñuelas M, Candel FJ, et al. Indicator opportunistic infections after biological treatment in rheumatoid arthritis, 10 years follow-up in a real-world setting. Ther Adv Musculoskelet Dis. 2019. https://doi.org/10.1177/1759720X19878004.
Maloisel F, Benboubker L, Gardembas M, et al. Long-term outcome with pentostatin treatment in hairy cell leukemia patients: a French retrospective study of 238 patients. Leukemia. 2003;17(1):45–51. https://doi.org/10.1038/sj.leu.2402784.
Masci G, Magagnoli M, Gullo G, et al. Herpes infections in breast cancer patients treated with adjuvant chemotherapy. Oncology. 2006;71(3–4):164–7. https://doi.org/10.1159/000106065.
Obrișcă B, Vornicu A, Jurubiță R, et al. Corticosteroids are the major contributors to the risk for serious infections in autoimmune disorders with severe renal involvement. Clin Rheumatol. 2021;40(8):3285–97. https://doi.org/10.1007/s10067-021-05646-2.
Pour L, Adam Z, Buresova L, et al. Varicella-zoster virus prophylaxis with low-dose acyclovir in patients with multiple myeloma treated with bortezomib. Clin Lymphoma Myeloma. 2009;9(2):151–3. https://doi.org/10.3816/CLM.2009.n.036.
Rampotas A, Djebbari F, Panitsas F, et al. Efficacy and tolerability of VCD chemotherapy in a UK real-world dataset of elderly transplant-ineligible newly diagnosed myeloma patients. Eur J Haematol. 2021;106(4):563–73. https://doi.org/10.1111/ejh.13588.
Rodriguez-Moreno A, Sanchez-Fructuoso AI, Calvo N, et al. Varicella infection in adult renal allograft recipients: experience at one center. Transplant Proc. 2006;38(8):2416–8. https://doi.org/10.1016/j.transproceed.2006.08.060.
Sulowicz J, Wojas-Pelc A, Kuzniewski M, Ignacak E, Janda K, Sulowicz W. Cutaneous viral infections in patients after kidney transplantation: risk factors. Polskie Arch Med Wewnetrznej. 2013;123(12):686–92. https://doi.org/10.20452/pamw.2013.
Thomson KJ, Hart DP, Banerjee L, Ward KN, Peggs KS, Mackinnon S. The effect of low-dose aciclovir on reactivation of varicella zoster virus after allogeneic haemopoietic stem cell transplantation. Bone Marrow Transplant. 2005;35(11):1065–9. https://doi.org/10.1038/sj.bmt.1704959.
Tischer J, Engel N, Fritsch S, et al. Virus infection in HLA-haploidentical hematopoietic stem cell transplantation: incidence in the context of immune recovery in two different transplantation settings. Ann Hematol. 2015;94(10):1677–88. https://doi.org/10.1007/s00277-015-2423-y.
Van Den Neste E, Michaux L, Layios N, et al. High incidence of complications after 2-chloro-2’-deoxyadenosine combined with cyclophosphamide in patients with advanced lymphoproliferative malignancies. Ann Hematol. 2004;83(6):356–63. https://doi.org/10.1007/s00277-004-0858-7.
van der Have M, Belderbos TDG, Fidder HH, et al. Screening prior to biological therapy in Crohn’s disease: Adherence to guidelines and prevalence of infections—results from a multicentre retrospective study. Dig Liver Dis. 2014;46(10):881–6. https://doi.org/10.1016/j.dld.2014.07.006.
Zappulo E, Buonomo AR, Saccà F, et al. Incidence and predictive risk factors of infective events in patients with multiple sclerosis treated with agents targeting CD20 and CD52 surface antigens. Open Forum Infect Dis. 2019;6(11):1–9. https://doi.org/10.1093/ofid/ofz445.
Nissen JC, Hummel M, Brade J, et al. The risk of infections in hematologic patients treated with rituximab is not influenced by cumulative rituximab dosage: a single center experience. BMC Infect Dis. 2014;14(1):364. https://doi.org/10.1186/1471-2334-14-364.
Lair-Mehiri L, Stefanescu C, Vaysse T, et al. Real-world evidence of tofacitinib effectiveness and safety in patients with refractory ulcerative colitis. Dig Liver Dis. 2020;52(3):268–73.
Acknowledgements
Medical Writing, Editorial and Other Assistance. The authors would like to thank Business & Decision Life Sciences Medical Communication Service Center for editorial assistance and manuscript coordination, on behalf of GSK. Kavi Littlewood (Littlewood Writing Solutions, on behalf of GSK) provided medical writing support.
Funding
GlaxoSmithKline Biologicals S.A. (VEO-000299) funded this literature review and all costs related to the development of the publication, including the journal’s Rapid Service Fee.
Author information
Authors and Affiliations
Contributions
Amit Bhavsar, Alen Marijam, Hilde Vroling, Inga Posiuniene, Nicolas Lecrenier and Nikki Vroom were involved in the design of the study. Hilde Vroling and Nikki Vroom collected or generated the data. Alen Marijam, Hilde Vroling, Inga Posiuniene, Nicolas Lecrenier and Nikki Vroom analyzed and/or interpreted the data. All authors participated to the development of this manuscript and in its critical review with important intellectual contributions. All authors had full access to the data and gave approval of the final manuscript before submission. All authors agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of Interest
Amit Bhavsar, Alen Marijam, Inga Posiuniene and Nicolas Lecrenier are employed by and hold shares in GSK. Hilde Vroling and Nikki Vroom are employees of P95/Pallas. P95/Pallas received funding from GSK for the submitted work. P95/Pallas holds/held contracts with AstraZeneca, GSK, Pfizer, Sanofi and Seqirus, Orchard, BioMarin, Daiichi, Bavarian Nordic and Bayer. The authors declare no other financial and non-financial relationships and activities and no conflicts of interest.
Ethical Approval
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Trademark Statement
Shingrix is a trademark owned by or licensed to GSK. Zostavax is a trademark of MSD.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Prior Presentation. Data reported in the manuscript were presented at the 16th European Public Health Conference (EPH) 2023 in Dublin, Ireland, 8–11 Nov 2023.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Marijam, A., Vroom, N., Bhavsar, A. et al. Systematic Literature Review on the Incidence of Herpes Zoster in Populations at Increased Risk of Disease in the EU/EEA, Switzerland, and the UK. Infect Dis Ther 13, 1083–1104 (2024). https://doi.org/10.1007/s40121-024-00963-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-024-00963-w