Abstract
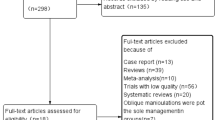
Percutaneous vertebral augmentation (PVA), which includes percutaneous kyphoplasty (PKP) and percutaneous vertebroplasty (PVP). Robot-assisted (RA) and fluoroscopy-assisted (FA) are important methods for treating osteoporotic vertebral compression fractures (OVCFs), though it is still unclear which is superior. This analysis aimed to compare the efficacy and safety of RA and FA. PubMed, Web of Science, Cochrane Library, and China National Knowledge Infrastructure were systematically searched, the outcomes included surgical parameters (leakage rate, operation time, number of fluoroscopic, injection volume, inclination angle), and clinical indexes (hospital stays, Visual Analog Scale (VAS), Oswestry Disability Index (ODI), Cobb angle, the midline height of vertebral). Thirteen articles involving 1094 patients were included. RA group produced better results than the FA group in the leakage rate (OR = 0.27; 95% CI 0.17–0.42; P < 0.00001), number of fluoroscopic (WMD = – 13.88; 95% CI – 18.47 to – 9.30; P < 0.00001), inclination angle (WMD = 5.02; 95% CI 4.42–5.61; P < 0.00001), hospital stays (WMD = – 0.32; 95% CI – 0.58 to – 0.05; P = 0.02), VAS within 3 days (WMD = – 0.19; 95% CI – 0.26 to – 0.12; P < 0.00001), Cobb angle within 3 days (WMD = – 1.35; 95% CI – 2.56 to – 0.14; P = 0.003) and Cobb angle after 1 month (WMD = – 1.02; 95% CI – 1.84 to – 0.20; P = 0.01). But no significant differences in operation time, injection volume, ODI, the midline height of vertebral, and VAS score after 1 month. Our analysis found that the RA group had lower cement leakage rates, number of fluoroscopic and hospital stays, a larger inclination angle, better short-term pain improvement, and Cobb angle improvement. It is worth acknowledging that robotic-assisted surgery holds promise for the development of spine surgery. The study was registered in the PROSPERO (CRD42023393497).





Similar content being viewed by others
Data availability
The data sets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- OVCFs:
-
Osteoporotic vertebral compression fractures
- PVA:
-
Percutaneous vertebral augmentation
- PKP:
-
Percutaneous kyphoplasty
- PVP:
-
Percutaneous vertebroplasty
- RA:
-
Robot-assisted
- FA:
-
Fluoroscopy-assisted
- BMI:
-
Body mass index
- BMD:
-
Bone mineral density
- VAS:
-
Visual analog scale
- ODI:
-
Oswestry disability index
- RCT:
-
Randomized controlled trial
- WMD:
-
Weighted mean difference
- SMD:
-
Standardized mean difference
- CI:
-
Confidence interval
- OR:
-
Odds ratio
- CT:
-
Computed tomography
- M–H:
-
Mantel–Haenszel
- IV:
-
Inverse variance
- df:
-
Degrees of freedom
References
Patel D, Liu J, Ebraheim NA (2022) Managements of osteoporotic vertebral compression fractures: a narrative review. World J Orthop 13:564–573. https://doi.org/10.5312/wjo.v13.i6.564
Qin J, Zhong W, Quan Z (2022) The surgical management trends of osteoporotic vertebral compression fractures: 5-year experience in one institution. Sci Rep 12:18040. https://doi.org/10.1038/s41598-022-23106-y
Long Y, Yi W, Yang D (2020) Advances in vertebral augmentation systems for osteoporotic vertebral compression fractures. Pain Res Manag 2020:3947368. https://doi.org/10.1155/2020/3947368
Ren H, Feng T, Cao J et al (2022) A retrospective study to evaluate the effect of dynamic fracture mobility on cement leakage in percutaneous vertebroplasty and percutaneous kyphoplasty in 286 patients with osteoporotic vertebral compression fractures. Med Sci Monit 28:e935080. https://doi.org/10.12659/MSM.935080
Patel S, Chiu RG, Chaker AN et al (2022) Current trends and socioeconomic disparities in the utilization of spine augmentation for patients with osteoporotic vertebral compression fracture: a nationwide inpatient sample analysis from 2012 to 2016. Int J Spine Surg 16:490–497. https://doi.org/10.14444/8262
Lopez IB, Benzakour A, Mavrogenis A et al (2023) Robotics in spine surgery: systematic review of literature. Int Orthop 47:447–456. https://doi.org/10.1007/s00264-022-05508-9
Qian J, Fang C, Ge P et al (2022) Efficacy and safety of establishing an optimal path through unilateral pedicle under the assistance of surgical robot in percutaneous kyphoplasty. Pain Physician 25:E133–E140
Huang J, Xing T, Cheng Z et al (2022) AOSRV: development and preliminary performance assessment of a new robotic system for autonomous percutaneous vertebroplasty. Int J Med Robot 18:e2456. https://doi.org/10.1002/rcs.2456
Yuan W, Cao W, Meng X et al (2020) Learning curve of robot-assisted percutaneous kyphoplasty for osteoporotic vertebral compression fractures. World Neurosurg 138:e323–e329. https://doi.org/10.1016/j.wneu.2020.02.110
Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. PLoS Med 18:e1003583. https://doi.org/10.1371/journal.pmed.1003583
Faiz KW (2014) VAS–visual analog scale. Tidsskr Nor Laegeforen 134:323. https://doi.org/10.4045/tidsskr.13.1145
Fairbank JC, Pynsent PB (2000) The Oswestry disability index. Spine Phila Pa (1976) 25:2940–2952. https://doi.org/10.1097/00007632-200011150-00017
Sterne JAC, Savovic J, Page MJ et al (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 366:l4898. https://doi.org/10.1136/bmj.l4898
Sterne JA, Hernan MA, Reeves BC et al (2016) ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 355:i4919. https://doi.org/10.1136/bmj.i4919
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539–1558. https://doi.org/10.1002/sim.1186
Yuan W, Meng X, Cao W et al (2022) Robot-assisted versus fluoroscopy-assisted kyphoplasty in the treatment of osteoporotic vertebral compression fracture: a retrospective study. Global Spine J 12:1151–1157. https://doi.org/10.1177/2192568220978228
Wang B, Cao J, Chang J et al (2021) Effectiveness of Tirobot-assisted vertebroplasty in treating thoracolumbar osteoporotic compression fracture. J Orthop Surg Res 16:65. https://doi.org/10.1186/s13018-021-02211-0
Sun T, Zhang YZ, Hu XF et al (2022) Feasibility analysis of bi-planar fluoroscopic imaging robot assisted PKP in the treatment of osteoporotic vertebral compression fractures. Orthop Biomech Mater Clin Study 19:27–31. https://doi.org/10.3969/j.issn.1672-5972.2022.03.005
Lin S, Tan K, Hu J et al (2022) Effectiveness of modified orthopedic robot-assisted percutaneous kyphoplasty in treatment of osteoporotic vertebral compression fracture. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 36:1119–1125. https://doi.org/10.7507/1002-1892.202204013
Li Q, Wu C, Huang Z et al (2022) A comparison of robot-assisted and fluoroscopy-assisted kyphoplasty in the treatment of multi-segmental osteoporotic vertebral compression fractures. J Biomed Res 36:208–214. https://doi.org/10.7555/JBR.36.20220023
Jin M, Ge M, Lei L et al (2022) Clinical and radiologic outcomes of robot-assisted kyphoplasty versus fluoroscopy-assisted kyphoplasty in the treatment of osteoporotic vertebral compression fractures: a retrospective comparative study. World Neurosurg 158:e1–e9. https://doi.org/10.1016/j.wneu.2021.10.066
Zheng BL, Hao DJ, Lin B et al (2021) Puncture assisted by a “TINAVI” orthopaedic robot versus freehand puncture in vertebroplaty for osteoporotic vertebral compression fracture of the upper thoracic vertebra. Chin J Orthop Trauma 23:20–26
Zhang ZT, Zhang XH, Wei ZH et al (2018) Comparison of outcomes of robot assisted and conventional percutaneous vertebroplasty on osteoporotic vertebral compression fracture. J Clin Orthop Res 3:205–208
Yang N, Wang SB, Liu SF et al (2022) Effectiveness of robot-assisted percutaneous vertebroplasty for osteoporotic vertebral compression fracture in the elderly. West China Med J 37:1471–1475. https://doi.org/10.7507/1002-0179.202108283
Xie HQ, Li XK, Sun J et al (2021) Percutaneous vertebroplasty with robotic orthopedic assistance versus conventional fluoroscopy assistance for treatment of osteoporotic vertebral compression fractures: a clinical comparative study. Guangdong Med J 42:1102–1106
Tan L, Wen B, Guo Z et al (2023) Robot-assisted percutaneous vertebroplasty for osteoporotic vertebral compression fractures: a retrospective matched-cohort study. Int Orthop 47:595–604. https://doi.org/10.1007/s00264-022-05654-0
Shi B, Hu L, Du H et al (2021) Robot-assisted percutaneous vertebroplasty under local anaesthesia for osteoporotic vertebral compression fractures: a retrospective, clinical, non-randomized, controlled study. Int J Med Robot 17:e2216. https://doi.org/10.1002/rcs.2216
Guo S, Fu Q, Hang DH et al (2021) Effectiveness of Mazor spine robot -assisted percutaneous vertebroplasty with modified approach in treating lumbar osteoporotic vertebral compression fractures. Chin J Spine Spinal Cord 31:818–824. https://doi.org/10.3969/j.issn.1004-406X.2021.09.06
Zhang K, She J, Zhu Y et al (2021) Risk factors of postoperative bone cement leakage on osteoporotic vertebral compression fracture: a retrospective study. J Orthop Surg Res 16:183. https://doi.org/10.1186/s13018-021-02337-1
Tang B, Cui L, Chen X et al (2021) Risk factors for cement leakage in percutaneous vertebroplasty for osteoporotic vertebral compression fractures: an analysis of 1456 vertebrae augmented by low-viscosity bone cement. Spine (Phila Pa 1976) 46:216–222. https://doi.org/10.1097/BRS.0000000000003773
Li M, Zhang T, Zhang R et al (2023) Systematic retrospective analysis of risk factors and preventive measures of bone cement leakage in percutaneous kyphoplasty. World Neurosurg 171:e828–e836. https://doi.org/10.1016/j.wneu.2022.12.117
Wang L, Li C, Wang Z et al (2023) Comparison of robot-assisted versus fluoroscopy-assisted minimally invasive transforaminal lumbar interbody fusion for degenerative lumbar spinal diseases: 2-year follow-up. J Robot Surg 17:473–485. https://doi.org/10.1007/s11701-022-01442-5
Lin S, Wang F, Hu J et al (2022) Comparison of the accuracy and safety of TiRobot-assisted and fluoroscopy-assisted percutaneous pedicle screw placement for the treatment of thoracolumbar fractures. Orthop Surg 14:2955–2963. https://doi.org/10.1111/os.13504
Probst T, Akalin ER, Giannouchos A et al (2022) Learning curves of robotic technology in an orthopedic teaching hospital. Orthopadie (Heidelb) 51:739–747. https://doi.org/10.1007/s00132-022-04287-w
Hijikata Y, Kotani Y, Suzuki A et al (2023) Protective attitudes toward occupational radiation exposure among spine surgeons in japan: an epidemiological description from the survey by the society for minimally invasive spinal treatment. Medicina (Kaunas). https://doi.org/10.3390/medicina59030545
Li J, Fang Y, Jin Z et al (2020) The impact of robot-assisted spine surgeries on clinical outcomes: a systemic review and meta-analysis. Int J Med Robot 16:1–14. https://doi.org/10.1002/rcs.2143
D’Souza M, Gendreau J, Feng A et al (2019) Robotic-assisted spine surgery: history, efficacy, cost, and future trends. Robot Surg 6:9–23. https://doi.org/10.2147/RSRR.S190720
Zhang RJ, Zhou LP, Zhang L et al (2022) Safety and risk factors of TINAVI robot-assisted percutaneous pedicle screw placement in spinal surgery. J Orthop Surg Res 17:379. https://doi.org/10.1186/s13018-022-03271-6
Matur AV, Palmisciano P, Duah HO et al (2023) Robotic and navigated pedicle screws are safer and more accurate than fluoroscopic freehand screws: a systematic review and meta-analysis. Spine J 23:197–208. https://doi.org/10.1016/j.spinee.2022.10.006
Alsalmi S, Capel C, Chenin L et al (2018) Robot-assisted intravertebral augmentation corrects local kyphosis more effectively than a conventional fluoroscopy-guided technique. J Neurosurg Spine 30:289–295. https://doi.org/10.3171/2018.8.SPINE18197
Song Q, Zhao Y, Li D et al (2023) Effect of different bone cement distributions in percutaneous kyphoplasty on clinical outcomes for osteoporotic vertebral compression fractures: a retrospective study. Medicine (Baltimore) 102:e33309. https://doi.org/10.1097/MD.0000000000033309
Garcia D, Akinduro OO, De Biase G et al (2022) Robotic-assisted vs nonrobotic-assisted minimally invasive transforaminal lumbar interbody fusion: a cost-utility analysis. Neurosurgery 90:192–198. https://doi.org/10.1227/NEU.0000000000001779
Soliman MAR, Pollina J, Poelstra K et al (2022) Can a spine robot be more efficient and less expensive while maintaining accuracy? Int J Spine Surg 16:S50–S54. https://doi.org/10.14444/8277
Acknowledgements
The authors acknowledged the Department of Statistics, Public Health College of Jilin University for their suggestions concerning the statistical analysis in this manuscript.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
Q-sZ designed the study protocol. XW and Y-hZ managed the literature search and data acquisition. XW and Y-hZ performed the statistical analysis and drafted the manuscript. Q-sZ provided critical revision to the manuscript. Q-sZ resolved ambiguities during the study and gave final approval of the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose. All the authors have no conflict of interest to declare.
Informed consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, X., Zhu, Yh. & Zhu, Qs. Efficacy and safety of robot-assisted versus fluoroscopy-assisted PKP or PVP for osteoporotic vertebral compression fractures: a systematic review and meta-analysis. J Robotic Surg 17, 2597–2610 (2023). https://doi.org/10.1007/s11701-023-01700-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11701-023-01700-0