Abstract
Background
Thirty-day readmission penalties implemented with the Hospital Readmission Reduction Program (HRRP) place a larger burden on safety-net hospitals which treat a disproportionate share of racial minorities, leading to concerns that already large racial disparities in readmissions could widen.
Objective
To examine whether there were changes in Black-White disparities in 30-day readmissions for acute myocardial infarction (AMI), congestive heart failure (CHF), or pneumonia following the passage and implementation of HRRP, and to compare disparities across safety-net and non-safety-net hospitals.
Design
Repeated cross-sectional analysis, stratified by safety-net status.
Subjects
1,745,686 Medicare patients over 65 discharged alive from hospitals in 5 US states: NY, FL, NE, WA, and AR.
Main Measures
Odds ratios comparing 30-day readmission rates following an index admission for AMI, CHF, or pneumonia for Black and White patients between 2007 and 2014.
Key Results
Prior to the passage of HRRP in 2010, Black and White readmission rates and disparities in readmissions were decreasing. These reductions were largest at safety-net hospitals. In 2007, Blacks had 13% higher odds of readmission if treated in safety-net hospitals, compared with 5% higher odds in 2010 (P < 0.05). These trends continued following the passage of HRRP.
Conclusions
Prior to HRRP, there were large reductions in Black-White disparities in readmissions at safety-net hospitals. Although HRRP tends to assess higher penalties for safety-net hospitals, improvements in readmissions have not reversed following the implementation of HRRP. In contrast, disparities continue to persist at non-safety-net hospitals which face much lower penalties.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
BACKGROUND
Thirty-day readmissions are common and costly in Medicare.1 In order to reduce readmissions, the Hospital Readmission Reduction Program (HRRP) levies financial penalties on hospitals with higher than expected 30-day readmissions for certain targeted conditions, initially focusing on including acute myocardial infarction (AMI), congestive heart failure (CHF), and pneumonia. The program, which was passed as part of the Affordable Care Act in 2010 and went into effect in 2012, has been associated with reduced readmissions for targeted conditions following announcement and implementation of the program.2,3,4,5
The potential impact of the HRRP penalties on overall health care disparities, however, is ambiguous. Some evidence suggests that higher penalties may increase incentives to improve patient care transitions for hospitals that treat a large volume of minority patients.6 On the other hand, penalties may place a burden on already-financially constrained hospitals.7 This has been a particular concern to policymakers since safety-net and teaching hospitals are much more likely to be penalized under the HRRP.8, 9
Thirty-day hospital readmissions have been associated with a variety of patient-related factors including medical complexity and sociodemographic factors.10, 11 Previous research has also shown that there are significant racial disparities in readmissions, even after adjusting for comorbidities.10 The HRRP adjusts targeted readmission rates for age, sex, and case mix, but not race or socioeconomic factors. The purpose of this study was to investigate how HRRP may have influenced health care disparities by examining trends in readmissions by race and hospital safety-net status from 2007 to 2014.
METHODS
Data Sources and Study Population
We used the 2007–2014 state inpatient data from the Healthcare Cost and Utilization Project (HCUP) to identify hospitalizations for Medicare beneficiaries initially admitted for the conditions targeted by HRRP: acute myocardial infarction, congestive heart failure, and pneumonia. The HCUP state inpatient data include administrative data on hospital procedures, diagnoses, and charges, as well as patient characteristics, including age, gender, and race for all hospital admissions in the state.12 We included all inpatient discharges with any of the three targeted diagnoses, for patients aged 65 and older with Medicare as their primary payer from five states (Arkansas, Florida, Nebraska, New York, and Washington), discharged alive, who did not leave against medical advice (n = 1,745,686). We used these five states because the discharge records contain revisit indicators, which are needed to calculate the days between the index hospitalization and subsequent hospitalizations for the same patient, and because these states had data available for 2007 through 2014. We also performed sensitivity analysis using data from Massachusetts, which has revisit indicators back to 2011, and Iowa, which has revisit indicators back to 2009. We supplemented the HCUP data with data from the 2011 American Hospital Association Annual Survey and the CMS impact file to obtain hospital characteristics.
Thirty-Day Readmissions
We calculated 30-day readmissions following the published guidelines set by the Centers for Medicare and Medicaid Services.13 A hospitalization was identified as a readmission for any condition within 30 days of a previous hospital discharge for one of the targeted conditions. We excluded transfers to other hospitals and potentially planned readmissions, which were defined using the CMS-published algorithms. Generally, planned readmissions include non-acute admissions for typically scheduled procedures and other types of care (e.g., rehabilitation, transplant surgery).14
HRRP Passage
HRRP was announced along with the passage of the Affordable Care Act in March 2010. The program was not fully implemented until 2012, and the first rounds of penalties were not imposed until 2013. The 2013 penalties included a lookback period back to 2008. Although there are many possible cut points to look at the impact of the program, previous research has suggested most of the impact of HRRP was actually felt immediately after the March 2010 announcement, with readmissions declining at the fastest rate between 2010 and 2012, and then plateauing around the time of the full implementation of the program in 2012.2, 3, 5 Thus, we used 2010 as the relevant cut point to descriptively examine what happened to disparities in readmissions following the announcement of HRRP.
Hospital Characteristics
We examined how a hospital’s status as a safety-net provider may play a role in the change in readmission disparities over time. In order to make simple comparisons, we split hospitals into two groups. Following earlier work, we used the Disproportionate Share Hospital (DSH) index from the CMS impact file to identify safety-net hospitals as those hospitals in the top quartile of the DSH index.15, 16 The DSH index is the sum of the percentage of beneficiaries treated at the hospital who receive both Medicare Part A and Supplemental Security Income benefits and the percentage who receive Medicaid, but not Medicare benefits. Although for simplicity, we focus on safety-net hospitals, we note that safety-net status is also strongly correlated with other concepts, such as highly penalized hospitals and minority-serving hospitals. For instance, although safety-net hospitals made up approximately 25% of all hospitals, they made up 47% of highly penalized hospitals (defined as having penalties above the 50th percentile) in our sample. Additionally, 77% of safety-net hospitals were minority-serving hospitals (defined as having greater than 40% of discharges among Black or Hispanic patients) compared with just 11% of non-safety-net hospitals.
Individual Characteristics
We focused on comparisons between non-Hispanic Whites and non-Hispanic Blacks, and excluded Hispanics, Asians, and other races from our analysis since the reliability of race data is highest among these groups in state hospital discharge data,17 and this is consistent with the previous literature.10 We abstracted age, sex, and race from the discharge data. In order to adjust for patient complexity, we calculated the Elixhauser Comorbidity Index, summing the total number of the 30 Elixhauser diagnoses reported during the index admission using ICD-9 codes.18
Statistical Analysis
We used logistic regressions to model the individual likelihood of readmission as a function of race by year interactions, controlling for age, sex, and Elixhauser Comorbidity Index. Using the regression model, we calculated the adjusted readmission rate by calculating the average likelihood of readmission for each year for Whites and Blacks at the mean values of the covariates using the margins command in Stata 13.1. We then repeated this analysis, stratifying by hospital safety-net status and HRRP penalty status by using separate regression models on the restricted sample. In sensitivity analyses, we examined the state-level Black-White differences in state-level trends in readmissions using separate linear regressions for each state. Because state-level data had smaller sample sizes and a higher degree of variability, we examined the overall annual trend using a continuous year variable, and an interaction of that variable with race. All analyses were done in SAS 9.3 and Stata 13.1.
RESULTS
Table 1 compares characteristics of patients in our sample during the period from 2007 to 2014 across different hospital types. The overall readmission rate over this time period was 21.3%, and that rate was higher for patients treated in safety-net hospital (22.9%). Patients at safety-net and high-penalty hospitals were more likely to be Black or other racial minorities and to be female. Rates of comorbidities were similar across both hospital types. HRRP penalties disproportionately impacted safety-net hospitals, which had, on average, nearly doubled the penalties of their counterparts. By our definition, safety-net hospitals served a population that included over 50% patients receiving Medicaid or SSI, compared with less than 20% in all other hospitals. Appendix Table 1 expands this table by showing differences across each quartile of the DSH index, and Appendix Table 2 shows the same results stratifying by high HRRP penalties vs. low penalties. There is a sharp difference between the highest quartile, which we define as safety-net hospitals and the lower three quartiles.
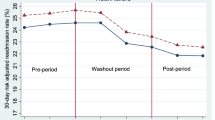
Table 2 shows adjusted readmission rates and the odds ratio comparing Blacks and Whites at three time periods—2007, 2010, and 2014—where 2010 represents the year that HRRP was enacted. Similarly Figure 1 presents this information graphically for all years with a vertical line dividing the time period between pre-HRRP and post-HRRP. Table 2 and Figure 2 also present differences in these trends between safety-net and non-safety-net hospitals. Overall, between 2007 and 2014, there was a significant decrease in readmission rates (2007, 24.3%; 2014, 18.6%, P < 0.01) in both safety-net and non-safety-net hospitals. Figure 1 and Table 2 show adjusted readmission rates by race over time. In 2007, Blacks had 17% higher odds of being readmitted compared with non-Hispanic Whites. By 2014, this ratio was reduced to 10% higher odds for Blacks, and the reduction was statistically significant (P < 0.01). Results from our sensitivity analysis including data from Massachusetts and Iowa are shown in Appendix Table 4, and provide similar results. Appendix Table 5 shows results by state. The individual state results are nosier, with significant narrowing of disparities in Arkansas and Washington, and non-significant differences in other states.
Pre-HRRP (2007–2010)
Even prior to the passage of HRRP, readmission rates were declining for both Blacks and Whites, and this was occurring at both safety-net and non-safety-net hospitals. In this period, disparities between Blacks and Whites were also declining. In fact, most of the decrease in disparities occurred prior to the passage of HRRP. This was entirely due to declining disparities at safety-net hospitals. In fact, the Black-White gap in readmissions at safety-net hospitals was only borderline significant in 2010, prior to the enactment of HRRP. Disparities persisted at non-safety-net hospitals, which saw small but not statistically significant increases in the Black-White readmission gap. Although disparities in readmission rates were initially slightly larger in safety-net hospitals compared with their counterparts, by 2010, these disparities were smaller in safety-net hospitals.
Post-HRRP (2010–2014)
During the period following the enactment of HRRP, readmission rates continued to decline for both Black and White patients. Despite being disproportionately impacted by the HRRP penalties, the earlier gains made in disparities at safety-net hospitals were not reversed following implementation of HRRP. In fact, our point estimates suggest a continued decrease in disparities at safety-net hospitals over the period from 2010 to 2014, though this change is not statistically significant. By 2014, readmission rates between Whites and Blacks were not statistically different from one another in safety-net hospitals. Further, by 2014, Blacks were statistically significantly less likely to be readmitted if they were treated in high-penalty hospital than if they were treated at a low-penalty hospital (Appendix Table 3), and had similar rates of readmission in safety-net versus non-safety-net hospitals.
DISCUSSION
Black-White disparities in readmissions decreased significantly during the years leading up to and following the passage and implementation of Medicare 30-day readmission penalties. Despite these improvements, significant disparities remain—Black patients are still much more likely to be readmitted than White patients.
Our data show that both readmission rates and disparities in readmission rates were already declining prior to the announcement of the HRRP (2010) and the implementation of the program (2012), so it is difficult from these data alone to conclude how much, if any, of the decrease in disparity was associated with the policy. However, regardless of the cause of the decrease, the fact that disparities did not increase, and in some cases continued to decrease, is important. Black patients are more likely to be treated in safety-net hospitals. These hospitals also tend to have low profit margins, and there has been significant concern that the combination of financial constraints and higher penalties would leave them unable to address readmissions.7, 19, 20 Additionally, since many of the sociodemographic factors related to readmissions are outside the control of hospitals, and these factors are associated with race, it was possible that hospitals might be better positioned to reduce disparities in non-disadvantaged populations, exacerbating disparities. Our results should provide encouragement but also some concern to policymakers. We show that the large downward trend in readmissions that began prior to the passage of HRRP continued following its enactment and implementation. Further, the large decreases in disparities in safety-net hospitals that occurred in the years prior to HRRP did not reverse following the enactment and implantation as many had feared. In addition, the finding that by the end of our study period safety-net and highly penalized hospitals had lower disparities and, in the case of highly penalized hospitals, lower adjusted readmissions among Black patients than their counterparts suggests that this is not simply the case that hospitals that had the most room for improvement improved the most. On the other hand, of considerable concern is that safety-net hospitals have continued to receive higher penalties even though they have reached a major national policy goal (essentially eliminating disparities),8 while hospitals that continue to have large disparities face much lower penalties.
Our findings are similar to other recent papers by Figueroa and colleagues who found similar reductions in disparities using national data.21 In addition, previous studies have shown that safety-net hospitals have seen greater improvements in readmissions,3, 22 but the fact that disparities also decreased suggests that these constrained hospitals were still able to reduce readmissions for Black patients. Nonetheless, safety-net hospitals are among the most adversely affected by HRRP. For instance, safety-net hospitals had, on average, nearly doubled the penalties of non-safety-net hospitals. It is possible that these higher penalties result from higher rates of readmission not offset by risk adjustment. For example, safety-net hospitals may have more readmissions related to socioeconomic factors which may be correlated with race. Thus, it is possible that cuts to DSH payments, particularly in non-Medicaid expansion states, will eventually lead to a decrease in quality and a return to higher levels of readmissions and disparities in the future, and this deserves attention in future studies.
This present study had several limitations. Importantly, since we only examined trends in readmissions and disparities, we are unable to determine how much of the change in disparities is causally related to the HRRP or any other policy that may affect hospital funding. Our data are from state hospital inpatient files, which include both fee-for-service Medicare and Medicare Advantage (MA), but do not distinguish between them. Enrollment in MA plans increased slightly during our study period from 23 to 31%, and hospitals are not penalized under HRRP for readmissions among MA enrollees.23 Additionally, the state inpatient databases only capture admissions within a given state, and readmissions that occur in a different state from the index admission are not captured.
As we move forward, it is unclear how disparities in readmissions will change as the HRRP evolves to account for socioeconomic factors. The 21st Century Cures Act includes legislation requiring the HRRP to account for hospital proportion of dually eligible patients. Although this adjustment does not take race or other important socioeconomic factors into consideration, it may be a step toward leveling the playing field for hospitals treating high proportions of socioeconomically disadvantaged patients. However, it seems equally plausible that it reduces the incentives facing these hospitals to make care improvements for dually eligible patients, which, to the extent that racial minorities are more likely to be dually eligible, may exacerbate racial disparities. Thus, it will be important to monitor changes in readmission disparities following these upcoming policy changes.
References
Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418–1428.
Zuckerman RB, Sheingold SH, Orav EJ, Ruhter J, Epstein AM. Readmissions, observation, and the hospital readmissions reduction program. N Engl J Med. 2016;374(16):1543–1551.
Desai NR, Ross JS, Kwon JY, et al. Association between hospital penalty status under the hospital readmission reduction program and readmission rates for target and nontarget conditions. JAMA. 2016;316(24):2647–2656.
Mellor J, Daly M, Smith M. Does it pay to penalize hospitals for excess readmissions? Intended and unintended consequences of Medicare’s hospital readmissions reductions program. Health Econ. 2017;26(8):1037–1051.
Wasfy JH, Zigler CM, Choirat C, Wang Y, Dominici F, Yeh RW. Readmission Rates After Passage of the Hospital Readmissions Reduction Program: A Pre–Post Analysis. Ann Intern Med. 2017;166(5):324–331.
Carey K, Lin M-Y. Hospital Readmissions Reduction Program: safety-net hospitals show improvement, modifications to penalty formula still needed. Health Aff. 2016; https://doi.org/10.1377/hlthaff.2016.0537.
Bhalla R, Kalkut G. Could Medicare readmission policy exacerbate health care system inequity? Ann Intern Med. 2010;152(2):114–117.
Thompson MP, Waters TM, Kaplan CM, Cao Y, Bazzoli GJ. Most Hospitals Received Annual Penalties For Excess Readmissions, But Some Fared Better Than Others. Health Aff. 2017;36(5):893–901.
Joynt KE, Jha AK. Characteristics of hospitals receiving penalties under the Hospital Readmissions Reduction Program. JAMA. 2013;309(4):342–343.
Joynt KE, Orav EJ, Jha AK. Thirty-day readmission rates for Medicare beneficiaries by race and site of care. JAMA. 2011;305(7):675–681.
Kind AJ, Jencks S, Brock J, et al. Neighborhood Socioeconomic Disadvantage and 30-Day RehospitalizationA Retrospective Cohort StudyNeighborhood Socioeconomic Disadvantage and 30-Day Rehospitalization. Ann Intern Med. 2014;161(11):765–774.
Healthcare Cost and Utilization Project (HCUP). HCUP State Inpatient Databases (SID). In: Quality AfHRa, ed. Rockville, MD2007–2014.
Centers for Medicare & Medicaid Services. Readmissions Reduction Program. 2014; http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.html. Accessed December 4, 2018.
Horwitz L, Partovian C, Lin Z, et al. Centers for Medicare & Medicaid Services Planned Readmission Algorithm—Version 2.1. In:2015.
Jha AK, Orav EJ, Epstein AM. The effect of financial incentives on hospitals that serve poor patients. Ann Intern Med. 2010;153(5):299–306.
Glass D, Lisk C, Stensland J. Refining the hospital readmissions reduction program. Washington, DC: Medicare Payment Advisory Commission. 2012.
Andrews RM. Statewide hospital discharge data: collection, use, limitations, and improvements. Health Serv Res. 2015;50(S1):1273–1299.
Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998:8–27.
Gu Q, Koenig L, Faerberg J, Steinberg CR, Vaz C, Wheatley MP. The Medicare Hospital Readmissions Reduction Program: potential unintended consequences for hospitals serving vulnerable populations. Health Serv Res. 2014;49(3):818–837.
Joynt KE, Jha AK. A path forward on Medicare readmissions. N Engl J Med. 2013;368(13):1175–1177.
Figueroa JF, Zheng J, Orav EJ, Epstein AM, Jha AK. Medicare Program Associated With Narrowing Hospital Readmission Disparities Between Black And White Patients. Health Aff. 2018;37(4):654–661.
Salerno AM, Horwitz LI, Kwon JY, et al. Trends in readmission rates for safety-net hospitals and non-safety-net hospitals in the era of the US Hospital Readmission Reduction Program: a retrospective time series analysis using Medicare administrative claims data from 2008 to 2015. BMJ Open. 2017;7(7):e016149.
Jacobson G, Damico A, Neuman T, Gold M. Medicare Advantage 2015 spotlight: enrollment market update. Issue Brief, Henry J Kaiser Family Foundation files http://files.kff.org/attachment/issue-brief-medicare-advantage-2015-spotlight-enrollment-market-update. 2015. Accessed December 4, 2018.
Funding
This study was funded by the Agency for Healthcare Research and Quality (R01 HS023783).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Kaplan previously served as a co-investigator on a research contract funded by AbbVie Pharmaceuticals. Dr. Waters has provided expert testimony for several health care providers. All remaining authors declare that they do not have a conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
ESM 1
(DOCX 29 kb)
Rights and permissions
About this article
Cite this article
Kaplan, C.M., Thompson, M.P. & Waters, T.M. How Have 30-Day Readmission Penalties Affected Racial Disparities in Readmissions?: an Analysis from 2007 to 2014 in Five US States. J GEN INTERN MED 34, 878–883 (2019). https://doi.org/10.1007/s11606-019-04841-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-019-04841-x