Abstract
Purpose
A significant number of people will experience prolonged symptoms after COVID-19 infection that will greatly impact functional capacity and quality of life. The aim of this study was to identify trajectories of health-related quality of life (HRQOL) and their predictors among adults diagnosed with COVID-19.
Methods
This is a retrospective analysis of an ongoing prospective cohort study (BQC-19) including adults (≥18y) recruited from April 2020 to March 2022. Our primary outcome is HRQOL using the EQ-5D-5L scale. Sociodemographic, acute disease severity, vaccination status, fatigue, and functional status at onset of the disease were considered as potential predictors. The latent class mixed model was used to identify the trajectories over an 18-month period in the cohort as a whole, as well as in the inpatient and outpatient subgroups. Multivariable and univariable regressions models were undertaken to detect predictors of decline.
Results
2163 participants were included. Thirteen percent of the outpatient subgroup (2 classes) and 28% in the inpatient subgroup (3 classes) experienced a more significant decline in HRQOL over time than the rest of the participants. Among all patients, age, sex, disease severity and fatigue, measured on the first assessment visit or on the first day after hospital admission (multivariable models), were identified as the most important predictors of HRQOL decline. Each unit increase in the SARC-F and CFS scores increase the likelihood of belonging to the declining trajectory (univariable models).
Conclusion
Although to different degrees, similar factors explain the decline in HRQOL over time among the overall population, people who have been hospitalized or not. Clinical functional capacity scales could help to determine the risk of HRQOL decline.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The severe acute respiratory syndrome coronavirus 2 infection, responsible for the novel coronavirus disease 2019 (COVID-19), caused more than six million deaths worldwide between December 2019 and October 2022 [1]. During COVID-19, people may be asymptomatic or experience a spectrum of symptoms varying from very mild to severe [2]. Although most of the population has presented the asymptomatic or mild form of the disease, between 5 and 15% of COVID-19 survivors have developed more severe symptoms that required hospitalization, especially in the pre-vaccination era of the pandemic [3].
Furthermore, it has been reported that a significant number of people will experience persistent post-COVID-19 symptoms [4,5,6] commonly referred to as post-COVID condition. According to the WHO definition, this condition would be present in “individuals with a history of probable or confirmed infection, usually 3 months from the onset of COVID-19 with symptoms that last for at least 2 months and cannot be explained by an alternative diagnosis” [7]. Since then, the post-COVID condition has been associated with a broad range of symptoms involving various organ systems and several health outcomes [8]. The most prevalent symptoms reported include fatigue, attention and cognitive disorders, dyspnea and post-exertional malaise [4, 5]. Long-term adverse effects on overall functional capacity, ability to perform activities of daily living, ability to return to work, and quality of life have been reported [9].
The complex concept of health-related quality of life (HRQOL) is multidimensional and includes domains related to the physical, mental, emotional and social functioning, each in terms of objective and subjective measures [10]. HRQOL is well known to be affected by the individual’s physical, functional status and mental functioning, which can be reflected by the person’s level of fitness and ability to move and walk around independently and safely [11].
Although we have taken great steps towards understanding and managing COVID-19 and its long-term effects from a medical perspective, there are still few studies that investigated the clinical implications and their impact on affected individuals’ quality of life [12, 13] and the factors that predispose some individuals to a greater decline remain poorly understood.
This study aimed to identify HRQOL trajectories among predefined subpopulations (overall, outpatients and inpatients) and to identify the modifiable and non-modifiable predictors of these trajectories over time.
Methods
This is a retrospective analysis of an ongoing prospective cohort study of adults included in the Biobanque Québécoise de la COVID-19 (BQC-19) from April 2020 to March 2022[14], which consists of a provincial infrastructure involving 10 healthcare facilities of the Health and Social Services Network of Quebec (Canada). This province-wide, multicentre, initiative enabled the collection of biosamples and clinical data since the beginning of the pandemic [14]. This secondary-analysis study was approved by the Ethics Review Board of one of the recruiting healthcare facilities, the CIUSSS de l’Estrie–Centre Hospitalier Universitaire de Sherbrooke (#2022–4413). Informed consent was obtained from all participants included in the original study. The present study followed the Strengthening the Reporting of Observational studies in Epidemiology guidelines for cohort studies [15].
Study design and participants
From the original database, we included in the present study people who:1) were aged 18 and over, 2) had a confirmed diagnosis (PCR test), 3) were recruited in a hospital center (inpatient subgroup) or in a COVID-19 outpatient clinic (outpatient subgroup), 4) had at least the first assessment (baseline) and one follow-up clinical assessment (functional capacity and quality of life) one month after hospital discharge or one month after PCR diagnostic test in an outpatient clinic and 5) had at least one valid score on the primary outcome. For the outpatient subgroup, sociodemographic and clinical characteristics were collected at the first assessment visit. HRQOL data were collected at 1, 3, 6, 12 and 18 months after the PCR test. For the inpatient subgroup, sociodemographic and clinical characteristics were collected at the hospital admission and HRQOL data were collected at 1, 3, 6, 12 and 18 months after hospital discharge.
Health-related quality of fife
The primary outcome of this study was HRQOL, measured with the EuroQol 5-dimension 5-level preference-based questionnaire (EQ-5D-5L) [16]. This tool demonstrates moderate-to-strong correlations with global, physical, and functional health as well as with the performance on activities of daily living. It is associated with other multi-attribute utility instruments and has been used in a broad range of conditions, populations and settings [17]. The tool assesses five aspects of health: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression, each being rated on a scale of 0 to 5, where a score of 0 represents no problems and a score of 5 represents unable to or extreme problems. Based on the value set derived from Canadian population norms and preferences [18,19,20], the EQ-5D-5L can be summarized as an index value varying from −0.148 (worst score) to +0.949 (best score) [20]. The minimal important difference found in an adult population on the EQ-5D-5L range between 0.03 and 0.05 [21].
Potential predictors
The sociodemographic and clinical baseline characteristics as well as the severity of the disease (mild, moderate and severe) were collected. The severity grading score was based on the definitions of the WHO Working Group on the Clinical Characterization and Management of COVID-19 infection [2]. Fatigue was assessed by a physician and collected in a dichotomous way (yes or no) from the following question: “Do you currently experience any fatigue?”. Participants were also asked whether they were vaccinated or not.
Functional status was assessed by two validated tools: the 5-item sarcopenia screening self-administered questionnaire (SARC-F) [22] and the Clinical Frailty scale (CFS) [23,24,25]. The former assesses five components: strength, assistance with walking, rise from a chair, climb stairs, and falls in the past year, with the total score ranging from 0 to 10, where a score ≥4 is considered a negative predictor of poor muscle function, known under the term sarcopenia. In fact, individuals with post-COVID-19 condition are at high risk of developing sarcopenia [26]. This scale has been validated to detect people at risk of sarcopenia-related adverse outcomes and decline in functional capacity in older adults [22]. The CFS has been used in several clinical studies to screen and assess physical phenotypes. The scale stratifies the patients according to their physical fitness or condition and level of independence in performing daily tasks. Its score ranges from 1 to 9, where 1 represents a person that is very fit and 9 a person that is terminally ill [27].
Statistical methods
The sample is described using descriptive statistics. Categorical variables are summarized using counts and percentages. Normally distributed continuous variables, assessed visually using Q-Q plots, are described using the mean and standard deviations. No imputation methods were used. Except for vaccination status, missing data were not reported in the descriptive statistics because of their small proportion (percentage equal to or below 6%). These were handled by mixed modelling for trajectories and by listwise deletion for association of covariate and classes. The X2 test was used to identify differences between subgroups for categorical variables. Continuous variables were presented as means and standard deviations and a 5% significant level was adopted.
The latent class mixed model (LCMM) was used to identify the trajectories of HRQOL over an 18-month period among all participants and by subgroups (inpatients and outpatient). This model creates potential profiles by combining a latent class model to identify homogenous latent groups of subjects and a mixed model to describe the mean trajectory over time in each group. This method allows to obtain an adequate estimate of the error while considering the individual correlation between repeated measures. Different criteria were examined to determine the optimal model structure: a) number of latent classes, b) shape and functional forms of the trajectories (linear or quadratic), and c) the form and structure of the variance–covariance matrix of random effects (unstructured or diagonal). The appropriate model was then determined according to the Bayesian Information Criterion (BIC). The entropy and relative entropy indexes were used to evaluate the accuracy of classification of individuals into the different latent classes, with higher values indicating a better accuracy. Results were obtained using the R function hlme in the lcmm package[28]. For covariates, since the main goal was to predict class membership, we used a standard three-step method [29, 30]. More precisely, we used LCMM without any predictors (Step 1), we saved the most likely class and merged it with the original data (Step 2) and analyzed it separately with a multinomial logistic regression (Step 3).
The multinomial logistic regression assessed the strength of the associations between the covariates (predictors) of interest and the identified trajectories to characterize them. As reference for the multinomial outcome, the upper trajectory was the more stable over time and was chosen to give a better portrayal of lower trajectories groups. Covariates included age, sex, acute disease severity and fatigue symptoms. For the inpatient subgroup, intensive care unit admission (ICU) was added as a covariable. CFS and SARC-F scores were only in the form of univariable model as supplementary information but were excluded from the multivariable modeling due to the presence of multicollinearity. Results are presented as odds ratio (OR) for univariable models, and as adjusted odds ratio (aOR) for multivariable models, with their respective 95%-confidence intervals. Results were obtained using SPSS v.28 and R v.4.0.2.
Results
A total of 2163 individuals were eligible for this secondary-analysis study. Among these, 26% was infected during the first wave of COVID-19 in Quebec (January 25 to August 22, 2020), 38% during the second wave (August 23, 2020, to March 20, 2021), 9% during the third wave (March 21 to July 17, 2021) and 27% after July 17, 2021. There is many missing data on vaccination status (88% of these data were missing at the first assessment visit). Therefore, vaccination status could not be considered as a potential covariate.
Participants’ characteristics and between-subgroup comparisons are presented in Table 1. In summary, the outpatient subgroup is mostly composed of woman (63%) and adults aged between 18 and 65 years old (91%). The inpatient subgroup had a higher proportion of comorbidities than the outpatient subgroup, the most prevalent being hypertension (49%) and diabetes (31%). A higher percentage of individuals with obesity were found in the inpatient group (13%).
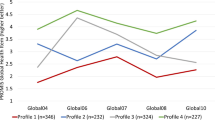
Health-related quality of life trajectories
The trajectories for all participants are presented followed by the presentation of the characteristics of participants in each trajectory as well as the multivariable and univariable analyses. Overall, without stratification according to hospitalization status, three main trajectories were identified (Fig. 1). The stable trajectory had an average HRQOL index value varying between 0.929 (95% CI: 0.926–0.932) and 0.928 (0.921–0.935). The middle trajectory remained stable over time. The average HRQOL index value started at 0.83 (0.81–0.84) and reached 0.80 (0.73–0.86) at 18 months. The decline trajectory had an HRQOL index of 0.52 (0.48–0.56) at baseline. After 6 months, the average index increased slightly and then had a sharp decline between months 6 and 18 to end up with an average index of 0.30 (0.18–0.41).
The characteristics of the participants identified in each of the trajectories are described in Table 2 and in the supplementary material. The stable trajectory represented 69% of the entire sample and the middle and decline trajectories represent 16% each.
The results of the multivariable and univariable analyses are presented in Table 3. The likelihood of belonging to the middle trajectory compared to the stable trajectory was significantly affected by age (≥65 years old), sex (women), COVID-19 disease severity, and the presence of fatigue. Finally, each unit increase in the SARC-F and CFS scores significantly increased the odds of being in the middle trajectory, when examined separately (univariable models).
The likelihood of belonging to the decline trajectory compared to the stable trajectory was significantly affected by age (≥65 y), sex (women), and COVID-19 disease severity. Each unit increase in the SARC-F and CFS scores significantly increased the odds of being in the decline trajectory when examined separately (univariable models).
Outpatient trajectories
In the outpatient subgroup, two trajectories were identified (Fig. 2a). The stable trajectory (upper curve) remained stable over time with an average HRQOL index value varying between 0.928 (0.924–0.932) at baseline and 0.924 (0.916–0.931) at 18 months. The HRQOL index value of the decline trajectory decreased progressively from 0.76 (0.72–0.79) to 0.60 (0.52–0.68) indicating a gradual decline in the HRQOL index over time, with the first and second thresholds of decline occurring around months 6 and 12 after diagnosis, respectively.
The characteristics of the participant in each trajectory are described in Table 2 and in Supplementary material. The stable trajectory represents 87% of the subsample and the decline trajectory represents 13%.
The results of the multivariable and univariable analyses are presented in Table 3. The likelihood of belonging to the decline trajectory compared to the stable trajectory was significantly affected by sex (woman) and the presence of fatigue at the time of the diagnosis. Each unit increase in the SARC-F and CFS score significantly increased the odds of being in the decline trajectory when examined separately.
Inpatient trajectories
In the inpatient subgroup, three trajectories were identified (Fig. 2b). The stable trajectory remained stable over time with an average HRQOL index value varying between 0.928 (0.923–0.932) at baseline and 0.926 (0.912–0.940) at 18 months. The middle trajectory remained relatively stable over time. The average HRQOL index value started at 0.80 (0.78–0.82) and reached 0.73 (0.62–0.83) at 18 months. The decline trajectory had an average HRQOL index of 0.43 (0.38–0.48) at baseline. At 6 months, the index value had slightly increased to reach 0.56 (0.49–0.63) and then had a pronounced decrease between months 6 and 18 to end up with an average index value of −0.04 (−0.42–0.33).
The characteristics of the participants in each trajectory are described in Table 2 and in supplementary material. The stable trajectory represented 53% of the subsample, the middle trajectory 21%, and the decline trajectory 28%.
The likelihood of belonging to the middle trajectory compared to the stable trajectory was significantly affected by age (≥65 y) and sex (woman). Each unit increase in the SARC-F and CFS scores significantly increased the odds of being in the middle trajectory (univariable models).
The likelihood of belonging to the decline trajectory compared to the stable trajectory was significantly affected by age (≥65 y), sex (women), and acute disease severity. Each unit increase in the SARC-F and CFS scores significantly increased the odds of being in the decline trajectory when examined separately.
Discussion
From our results, we can conclude that people with different profiles will present different HRQOL trajectories after a COVID-19 infection. In addition, 87% of participants in the outpatient subgroups remained stable in terms of quality of life over time, while 52% maintained this stability in the inpatient subgroups. Similar factors explained the decline in HRQOL among participants overall, regardless of whether they were hospitalized for COVID-19. Interestingly, self-reported fatigue, but not age or acute disease severity, predicted the decline trajectory in people diagnosed in the community.
Our results demonstrate that people who experienced a more important decline were those who had a poor HRQOL one month after the PCR test (outpatient) or one month after hospital discharge (inpatient). These findings suggest that people at risk of belonging to a trajectory of decline have some degree of health-related impairment of quality of life. Our findings are consistent with the results obtained in the COVID-19 survivors, which showed a significant decrease in HRQOL 90 after infection[31]. A meta-regression analysis performed showed that HRQOL was more impaired in ICU patients with fatigue than in those without it [12].
Some people with asymptomatic or mild disease will experience a decline in quality of life after a COVID-19 infection. Our analyses have shown that 13% of non- hospitalized people will experience a decrease in quality of life several months after the acute infection. This decrease was greater than the minimal important difference found in an adult population on the EQ-5D-5L[21, 32]. Although the reported prevalence of post-COVID condition is extremely variable[33,34,35], the 13% “decliners” found is consistent with the most conservative estimates of long COVID prevalence. In a longitudinal study of non-hospitalized patients, it has been shown that four months after the COVID-19 infection, patients still presented with some shortness of breath, anosmia, ageusia and fatigue [36]. Therefore, people in the community are also at risk of needing rehabilitation and seeking other healthcare services because of the long-term consequences of COVID-19.
For people diagnosed in the community, sex and the presence of fatigue seem to be the most important predictors of a more pronounced decline in quality of life, while being older and being a women seem to have a greater impact in the inpatient subgroup. Interestingly, fatigue has been shown to be an important predictor of HRQOL in many other conditions and several studies revealed that it is one of the most prevalent symptoms of the post-COVID condition [4, 36,37,38,39]. However, the presence of fatigue doesn’t appear to impact the risk of being in a decline trajectory in people who were hospitalized. One may argue that many other factors that go much beyond fatigue, such as prolonged immobilization, secondary complications and polypharmacy, can contribute to a worsening of function and quality of life in those patients [40, 41]. In summary, age, sex, severity of the COVID-19 infection and fatigue increase the likelihood of belonging to the declining trajectory and these are the most important predictors to HRQOL decline in the long term, although some differences can be observed according to the hospitalization status.
Physical and functional-related measures at the time of diagnosis, provided by the SARC-F and the Clinical Frailty scales, could be used, as complementary information, for rapid clinical risk assessment. Interestingly, the CFS has been evaluated as a prognostic tool to predict mortality in people with COVID-19 [24]. In this study, the severely frail or terminally ill patients were older (median age 80y) and had more comorbidities [24]. Along with the baseline HRQOL index and easily accessible information about non-modifiable factors (age, sex and acute disease severity), these two scales could be useful in assessing and determining prognosis (https://qualicovid.recherche.usherbrooke.ca/) in the context of physical rehabilitation and could, to a certain extent, assist decision-making in terms of the modality and volume of physical interventions that best meets their needs.
Early intervention is of utmost importance for people at risk of having a significant impact on quality of life [42]. Indeed, trajectories generally demonstrate a progressive decline without a noticeable improvement, even after 18 months. In addition, it is well known that acute, exacerbating, events that would happen throughout the individuals’ lives would make these trajectories even worse, as already demonstrated in other chronic and end-of-life health conditions [43, 44]. According to this “crisis model”, an acute event in an already debilitated health trajectory would cause a significant and even more pronounced decline in functionality, which would imply a reduced quality of life and, eventually, premature death. Therefore, people must be well identified as to the risk of decline and treated according to priorities and availability of resources. At first, predictors that are easy to use could help quickly identify a clientele at greater risk of decline. Since, age, sex, severity of the COVID-19 infection and fatigue increase the likelihood of belonging to a HRQOL declining trajectory, these could be useful as a quick risk screening test to be performed by healthcare practitioners when evaluating patients.
Strengths and limitations
Our study is based on the largest provincial multi-centre cohort study, which allows easy generalizability of results to a larger population. The cohort also includes individuals who were hospitalized, both in the ward and in the ICU, and individuals who had the diagnosis in a clinical outpatient setting, which is rare in most studies of COVID-19.
Finally, the standardized questionnaire used to measure quality of life is widely recommended in the literature [45]. It can be easily applied, and the results derived from it easily compared with other studies already published in other population. However, a generic HRQOL questionnaire may not capture the range of potential symptoms specifically associated with COVID-19 that could alter quality of life and may therefore be less sensitive to changes in HRQOL than a disease-specific questionnaire. The EQ-5D-5L takes into account the impact on quality of life in terms of mobility and ability to perform activities of daily living but does not take into account how specific symptoms of COVID-19 [16] may, by themselves, affect quality of life.
Our study, however, is not without limitations. We have a significant number of missing data on the vaccination status as well as the different variants that appeared over the duration of the study. It should be noted that the vaccine was not introduced to the Quebec population until spring of 2021, so 64% of our sample was infected in the first two waves of COVID-19 in Quebec, before the vaccine was even available. Therefore, the data collection was not designed to collect data on vaccination status, which explains the high percentage of missing data. Thus, vaccination status could not be considered as a potential covariate. It is possible that the vaccination status had an influence—possibly a protective influence—on the observed decline trajectories and that different variants affected these trajectories in different ways and to varying degrees. A study has shown, however, that being vaccinated prior to a COVID-19 infection seems to confer only a partial protection from the long-term effects of COVID-19, which suggests that there may have been only a small effect on HRQOL trajectories [46].
Our data analysis study ends at 18 months. Therefore, it is possible that downward trajectories experience gradual improvement, stabilization, or gradual decline thereafter. However, since the BQC-19 study in an ongoing study, further time points could be explored in a future study.
Participants were asked whether they had any fatigue symptoms, without further specification. Therefore, this does not quantify and qualify the level and extent of the fatigue symptoms. Other measurements such as the fatigue severity scale (FSS) [47], the Chalder Fatigue Scale (CFS) [48] or the Functional Assessment of Chronic Illness Therapy Fatigue (FACIT-F) [49] among others, would have provided more robust information on this potential predictor.
Frailty is increasingly recognized as an important construct affecting adult health and has been associated with poor physical and emotional health as well as with poor HRQOL. Because we do not have access to information about emotional health, it is impossible to know the extent to which this may have influenced HRQOL trajectories.
Some individuals were misclassified. At the time of recruitment, some people were recruited from the outpatient clinical settings and were considered outpatients, although further analysis showed that some of them had a previous hospitalization. These represent slightly under 3% of the data in the outpatient subgroup.
Finally, our cohort has a high percentage of people who have had a hospital stay because the BQC-19 study started recruiting exclusively in hospital centres that had the necessary infrastructure and staff needed to initiate data collection and, only a few months later, began to include people diagnosed in the community. Therefore, hospitalized individuals are probably over-represented in our cohort, influencing only the trajectories that have not been stratified.
Conclusion
In conclusion, people with different baseline profiles will present different quality of life trajectories after a COVID-19 infection and this, regardless of whether they were hospitalized or not. Among patients diagnosed in the community and in hospital centers, 13 and 28% of people, respectively, will experience an important decline in HRQOL after a COVID-19 infection. Age, sex, severity of the COVID-19 infection and fatigue increase the likelihood ratio of belonging to a HRQOL declining trajectory. Because it is unlikely that the quality of life of these people will improve over time without any concrete action or intervention, individualized and standardized assessments and interventions must be further investigated and implemented to better assist clinical decision-making in terms of approaches and modalities that best respond to the patient’s needs.
Data availability
Data with a very low risk of re-identification and no particular sensitivity (“open access data”), such as aggregated patient data from the different cohorts is available via the BQC19 website (https://www.bqc19.ca/) or can be requested by email at: info@bqc19.ca. Upon completion of the study, the publicly available data will be deposited in a repository.
References
WHO, (2022) WHO Coronavirus (COVID-19) Dashboard, 8 juillet 2022. https://covid19.who.int
WHO, (2020). A minimal common outcome measure set for COVID-19 clinical research. The Lancet. Infectious diseases, 20(8), 192–197. https://doi.org/10.1016/S1473-3099(20)30483-7
Government of Canada, (2020) Coronavirus disease (COVID-19), 13 septembre 2020. https://www.canada.ca/en/public-health/services/diseases/coronavirus-disease-covid-19.html (consulté le 5 octobre 2022)
Davis H, E. et al. (2020) Characterizing Long COVID in an International Cohort: 7 Months of symptoms and their impact. medRxiv. doi: https://doi.org/10.1101/2020.12.24.20248802
Lopez-Leon, S., et al. (2021). More than 50 long-term effects of COVID-19: a systematic review and meta-analysis. Scientific Reports, 11(1), 16144. https://doi.org/10.1038/s41598-021-95565-8
Nasserie, T., Hittle, M., Goodman, S. N. (2021) Assessment of the frequency and variety of persistent symptoms among patients with COVID-19: A systematic review. JAMA Network Open, 4(5), e2111417, doi: https://doi.org/10.1001/jamanetworkopen.2021.11417
Soriano, J. B., Murthy, S., Marshall, J. C., Relan, P., & Diaz, J. V. (2022). A clinical case definition of post-COVID-19 condition by a Delphi consensus. The Lancet Infectious Diseases, 22(4), e102–e107. https://doi.org/10.1016/S1473-3099(21)00703-9
Centers for Disease Control and Prevention (2022) Post-COVID conditions. Centers for Disease Control and Prevention. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html
Beauchamp, M. K. et al. (2022) Assessment of functional mobility after COVID-19 in adults Aged 50 years or older in the Canadian longitudinal study on Aging. JAMA Network Open, 5(1), e2146168. doi: https://doi.org/10.1001/jamanetworkopen.2021.46168
M. de Wit, M., Hajos, T. (2013). Health-related quality of life. In M. D. Gellman et J. R. Turner (Éds) Encyclopedia of Behavioral Medicine (pp. 929‑931) New York, NY: Springer New York. doi: https://doi.org/10.1007/978-1-4419-1005-9_753
Grassi, L., et al. (2020). Quality of life, level of functioning, and its relationship with mental and physical disorders in the elderly: results from the MentDis_ICF65+ study. Health and Quality of Life Outcomes, 18(1), 61. https://doi.org/10.1186/s12955-020-01310-6
Malik, P., et al. (2022). Post-acute COVID-19 syndrome (PCS) and health-related quality of life (HRQoL)—A systematic review and meta-analysis. Journal of Medical Virology, 94(1), 253–262. https://doi.org/10.1002/jmv.27309
Poudel, A. N., et al. (2021). Impact of Covid-19 on health-related quality of life of patients: A structured review. PLoS ONE, 16(10), 1–20.
Tremblay, K. et al. (2022) The Biobanque québécoise de la COVID-19 (BQC19)—A cohort to prospectively study the clinical and biological determinants of COVID-19 clinical trajectories. PLOS ONE, 16(5), e0245031. doi: https://doi.org/10.1371/journal.pone.0245031
Vandenbroucke, J. P., et al. (2014). Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. International Journal of Surgery (London, England), 12(12), 1500–1524. https://doi.org/10.1016/j.ijsu.2014.07.014
Herdman, M., et al. (2011). Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Quality of Life Research : An International Journal of Quality of Life Aspects of Treatment, care and Rehabilitation, 20(10), 1727–1736. https://doi.org/10.1007/s11136-011-9903-x
Feng, Y.-S., Kohlmann, T., Janssen, M. F., & Buchholz, I. (2021). Psychometric properties of the EQ-5D-5L: a systematic review of the literature. Quality of Life Research, 30(3), 647–673. https://doi.org/10.1007/s11136-020-02688-y
APERSU Team, (2018) Alberta Population Norms for EQ-5D-5L. p. 14
Poder, T. G., Carrier, N., & Kouakou, C. R. C. (2020). Quebec health-related quality-of-life population norms using the EQ-5D-5L: Decomposition by sociodemographic data and health problems. Value in Health, 23(2), 251–259. https://doi.org/10.1016/j.jval.2019.08.008
Xie, F., et al. (2016). A Time Trade-off-derived Value Set of the EQ-5D-5L for Canada. Medical care, 54(1), 98–105. https://doi.org/10.1097/MLR.0000000000000447
McClure, N. S., Sayah, F. A., Ohinmaa, A., & Johnson, J. A. (2018). Minimally important difference of the EQ-5D-5L index score in adults with type 2 diabetes. Value in Health, 21(9), 1090–1097. https://doi.org/10.1016/j.jval.2018.02.007
Malmstrom, T. K., Miller, D. K., Simonsick, E. M., Ferrucci, L., & Morley, J. E. (2016). SARC-F: a symptom score to predict persons with sarcopenia at risk for poor functional outcomes. Journal of Cachexia, Sarcopenia and Muscle, 7(1), 28–36. https://doi.org/10.1002/jcsm.12048
Church, S., Rogers, E., Rockwood, K., & Theou, O. (2020). A scoping review of the Clinical Frailty Scale. BMC Geriatrics, 20(1), 393. https://doi.org/10.1186/s12877-020-01801-7
Jachymek, M., et al. (2022) The value of clinical frailty scale (CFS) as a prognostic tool in predicting mortality in COVID-19-A retrospective Cohort study. International Journal of Environmental Research and Public Health, 19(3). doi: https://doi.org/10.3390/ijerph19031104.
Lee, C., Frishman, W. H (2021) Implications of frailty in COVID-19. Cardiology in Review, 29(6). Disponible sur: https://journals.lww.com/cardiologyinreview/Fulltext/2021/11000/Implications_of_Frailty_in_COVID_19.3.aspx
Piotrowicz, K., Gąsowski, J., Michel, J.-P., & Veronese, N. (2021). Post-COVID-19 acute sarcopenia: physiopathology and management. Aging Clinical and Experimental Research, 33(10), 2887–2898. https://doi.org/10.1007/s40520-021-01942-8
Rockwood, K., et al. (2005). A global clinical measure of fitness and frailty in elderly people. CMAJ, 173(5), 489. https://doi.org/10.1503/cmaj.050051
Proust-Lima, C., Philipps, V., & Liquet, B. (2017). Estimation of Extended Mixed Models Using Latent Classes and Latent Processes: The R Package lcmm. Journal of Statistical Software, 78(2), 1–56. https://doi.org/10.18637/jss.v078.i02
Andersen, S. B. Karstoft, K.-I., Bertelsen, M., Madsen, T. (20124) Latent trajectories of trauma symptoms and resilience: The 3-year longitudinal prospective USPER study of Danish veterans deployed in Afghanistan. Journal of Clinical Psychiatry, 75(9), 1001–1008. doi: https://doi.org/10.4088/jcp.13m08914.
Pietrzak, R. H., et al. (2014). Trajectories of PTSD risk and resilience in World Trade Center responders: An 8-year prospective cohort study. Psychological Medicine, 44(1), 205–219. https://doi.org/10.1017/S0033291713000597
Gamberini, L., et al. (2021). Quality of Life Research, 30(10), 2805–2817. https://doi.org/10.1007/s11136-021-02865-7
Tsai, A. P. Y., et al. (2021). Minimum important difference of the EQ-5D-5L and EQ-VAS in fibrotic interstitial lung disease. Thorax, 76(1), 37. https://doi.org/10.1136/thoraxjnl-2020-214944
Daugherty, S. E., et al. (2021). Risk of clinical sequelae after the acute phase of SARS-CoV-2 infection: retrospective cohort study. BMJ (Clinical research ed.), 373, 1098. https://doi.org/10.1136/bmj.n1098
Feldman, D. E., Boudrias, M.-H., & Mazer, B. (2022). Long COVID symptoms in a population-based sample of persons discharged home from hospital. Canadian Journal of Public Health., 113(6), 930–939. https://doi.org/10.17269/s41997-022-00695-9
Greenhalgh, T., Knight, M., A’Court, C., Buxton, M., & Husain, L. (2020). Management of post-acute covid-19 in primary care. BMJ, 370, 3026. https://doi.org/10.1136/bmj.m3026
Augustin, M., et al. (2021) Post-COVID syndrome in non-hospitalised patients with COVID-19: a longitudinal prospective cohort study. The Lancet Regional Health-Europe, 6, 100122. doi: https://doi.org/10.1016/j.lanepe.2021.100122
Charalambous, A., & Kouta, C. (2016). Cancer related fatigue and quality of life in patients with advanced prostate cancer undergoing chemotherapy. BioMed Research International., 2016, 3989286. https://doi.org/10.1155/2016/3989286
Elbers, R. G., van Wegen, E. E., Verhoef, J., & Kwakkel, G. (2014). Impact of fatigue on health-related quality of life in patients with Parkinson’s disease: a prospective study. Clinical Rehabilitation, 28(3), 300–311. https://doi.org/10.1177/0269215513503355
Nourbakhsh, B., Julian, L., & Waubant, E. (2016). Fatigue and depression predict quality of life in patients with early multiple sclerosis: a longitudinal study. European Journal of Neurology, 23(9), 1482–1486. https://doi.org/10.1111/ene.13102
Albuquerque de Almeida, F., Al, M. J., Koymans, R., Riistama, J., Pauws, S., & Severens, J. L. (2020). Impact of hospitalisation on health-related quality of life in patients with chronic heart failure. Health and Quality of Life Outcomes, 18(1), 262. https://doi.org/10.1186/s12955-020-01508-8
Wu. X., et al. (2018) The association between major complications of immobility during hospitalization and quality of life among bedridden patients: A 3 month prospective multi-center study. PloS one, 13(10), e0205729. doi: https://doi.org/10.1371/journal.pone.0205729
Barker-Davies, R. M., et al. (2020). The Stanford Hall consensus statement for post-COVID-19 rehabilitation. British Journal of Sports Medicine, 54(16), 949–959. https://doi.org/10.1136/bjsports-2020-102596
Giacomini, M., DeJean, D., Simeonov, D., & Smith, A. (2012). Experiences of living and dying with COPD: a systematic review and synthesis of the qualitative empirical literature. Ontario Health Technology Assessment Series, 12(13), 1–47.
Kristjánsdóttir, I., Thorvaldsen, T., Lund, L. H. (2020) Congestion and Diuretic Resistance in Acute or Worsening Heart Failure. Cardiac Failure Review, 6, e25. doi: https://doi.org/10.15420/cfr.2019.18
Zhou, T., Guan, H., Wang, L., Zhang, Y., Rui, M., Ma, A. (2021) Health-related quality of life in patients with different diseases measured with the EQ-5D-5L: A systematic review. Frontiers in Public Health, 9. Disponible sur: https://www.frontiersin.org/articles/https://doi.org/10.3389/fpubh.2021.675523
Al-Aly, Z., Bowe, B., & Xie, Y. (2022). Long COVID after breakthrough SARS-CoV-2 infection. Nature Medicine, 28(7), 1461–1467. https://doi.org/10.1038/s41591-022-01840-0
Whitehead, L. (2009). The measurement of fatigue in chronic illness: A systematic review of unidimensional and multidimensional fatigue measures. Journal of Pain and Symptom Management, 37(1), 107–128. https://doi.org/10.1016/j.jpainsymman.2007.08.019
Cell, M., & Chalder, T. (2010). Measuring fatigue in clinical and community settings. Journal of Psychosomatic Research, 69(1), 17–22. https://doi.org/10.1016/j.jpsychores.2009.10.007
Spadaro, S., et al. (2016). Fatigue in intensive care survivors one year after discharge. Health and Quality of Life Outcomes, 14(1), 148. https://doi.org/10.1186/s12955-016-0554-z
Acknowledgements
This work was made possible through open sharing of data and samples from the Biobanque québécoise de la COVID-19, funded by the Fonds de recherche du Québec—Santé, Génome Québec, the Public Health Agency of Canada and, as of March 2022, the ministère de la Santé et des Services sociaux. We thank all participants to BQC19 for their contribution. https://www.quebeccovidbiobank.ca
Funding
This study was funded by the Reseau Provincial de Recherche en Adaptation et Réadaptation (Provincial Network for Research in Adaptation and Rehabilitation) (Quebec, Canada).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data analysis was planned and performed by Pamela Tanguay, Samuel Lemaire-Paquette, Livia Pinheiro Carvalho and Marie-France Dubois. The first draft of the manuscript was written by Pamela Tanguay and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tanguay, P., Décary, S., Lemaire-Paquette, S. et al. Trajectories of health-related quality of life and their predictors in adult COVID-19 survivors: A longitudinal analysis of the Biobanque Québécoise de la COVID-19 (BQC-19). Qual Life Res 32, 2707–2717 (2023). https://doi.org/10.1007/s11136-023-03406-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-023-03406-0