Abstract
Children with developmental disabilities (DD) exhibit feeding and swallowing difficulties, which can have an impact on nutritional, developmental, and psychological aspects. The existing tools assess the nature of feeding problems and behaviors only. The present study aimed to assess the physical, functional, and emotional domains in children with DD with feeding issues using Feeding handicap index for children (FHI-C). For clinical validation, FHI-C was administered on the parents/caregivers of 60 children with cerebral palsy, 61 with autism spectrum disorder, 59 with intellectual disability and 60 typically developing children in the age range of 2 to 10 years. The results revealed that the mean scores (Total FHI-C and FHI-C domain scores) were significantly higher for all three clinical groups than for the control group, which revealed good clinical validity. Also, FHI-C was found to have significantly high test–retest reliability. The study presents a valid and reliable tool for assessing the psychosocial handicapping effects of feeding problems in children with DD. FHI-C provides a holistic picture about the psychosocial impact of feeding problems in children with DD and will assist the clinicians in prioritizing the goals for feeding therapy. The scores obtained can be used as reference for pre and post therapy comparison purposes.
Similar content being viewed by others
References
Adamo, K. B., & Brett, K. E. (2013). Parental perceptions and childhood dietary quality: Who holds the reins? Diet Quality (pp. 177–197). Humana Press.
Anil, M. A., Shabnam, S., & Narayanan, S. (2019). Feeding and swallowing difficulties in children with Down syndrome. Journal of Intellectual Disability Research, 63(8), 992–1014.
Arvedson, J. C. (2006). Swallowing and feeding in infants and young children. GI Motility Online. https://doi.org/10.1038/gimo17
Badalyan, V., & Schwartz, R. H. (2011). Feeding problems and GI dysfunction in children with asperger syndrome or pervasive developmental disorder not otherwise specified: Comparison with their siblings. Open Journal of Pediatrics, 1, 51–63.
Bandini, L. G., Anderson, S. E., Curtin, C., Cermak, S., Evans, E. W., & Scampini, R. (2010). Food selectivity in children with autism spectrum disorders and typically developing children. The Journal of Pediatrics, 157, 259–264.
Benfer, K. A., Weir, K. A., Bell, K. L., Ware, R. S., Davies, P. S., & Boyd, R. N. (2013). Oropharyngeal dysphagia and gross motor skills in children with cerebral palsy. Pediatrics, 131, e1553–e1562.
Benfer, K. A., Weir, K. A., & Boyd, R. N. (2012). Clinimetrics of measures of oropharyngeal dysphagia for preschool children with cerebral palsy and neurodevelopmental disabilities: A systematic review. Developmental Medicine and Child Neurology, 54, 784–795.
Berlin, K. S., Davies, W. H., Silverman, A. H., Woods, D. W., Fischer, E. A., & Rudolph, C. D. (2010). Assessing children’s mealtime problems with the mealtime behavior questionnaire. Children’s Health Care, 39, 142–156.
Cermak, S. A., Curtin, C., & Bandini, L. (2010). Food selectivity and sensory sensitivity in children with autism spectrum disorders. Journal of the American Dietetic Association, 110, 238–246.
Cooper, P., & Stein, A. (2006). Childhood feeding problems and adolescent eating disorders. Routledge.
Cooper-Brown, L., Copeland, S., Dailey, S., Downey, D., Petersen, M. C., Stimson, C., & Van Dyke, D. C. (2008). Feeding and swallowing dysfunction in genetic syndromes. Developmental Disabilities Research Reviews, 14, 147–157.
Cullinane, D., & Novak, P. (2013). Parent’s/caregiver’s relationship and the impact on nutrition. ICAN: Infant Child, & Adolescent Nutrition, 5, 311–314.
Davies, W. H., Ackerman, L. K., Davies, C. M., Vannatta, K., & Noll, R. B. (2007). About your child’s eating: Factor structure and psychometric properties of a feeding relationship measure. Eating Behaviors, 8, 457–463.
Davis, E., Nicolas, C., Waters, E., Cook, K., Gibbs, L., Gosch, A., & Ravens-Sieberer, U. (2007). Parent-proxy and child self-reported health-related quality of life: Using qualitative methods to explain the discordance. Quality of Life Research, 16, 863–871.
Dodrill, P., & Estrem, H. H. (2020). Quality of life assessment in children with feeding and swallowing disorders. Multidisciplinary management of pediatric voice and swallowing disorders. Springer.
Gangil, A. K., Patwari, S., Aneja, B., & Ahuja, and Anand, V. K. (2001). Feeding problems in children with cerebral palsy. Indian Pediatrics, 38, 839–846.
Gustafsson, B., & Tibbling, L. (1991). Dysphagia, an unrecognized handicap. Dysphagia, 6, 193–199.
Harvey, L., Bryant-Waugh, R., Watkins, B., & Meyer, C. (2015). Parental perceptions of childhood feeding problems. Journal of Child Health Care, 19, 392–401.
Kummer, A. (2008). Cleft palate & craniofacial anomalies: Effects on speech and resonance (2nd ed.). Cengage Learning.
Learned, S. (2014). Understanding dysphagia: The social and emotional Impact. University of Arkansas.
Lukens, C. T., & Linscheid, T. R. (2008). Development and validation of an inventory to assess mealtime behavior problems in children with autism. Journal of Autism and Developmental Disorders, 38, 342–352.
Määttä, S., Laakso, M. L., Tolvanen, A., Ahonen, T., & Aro, T. (2012). Developmental trajectories of early communication skills. Journal of Speech Language, and Hearing Research, 55, 1083–1096.
Marshall, J., Hill, R. J., Ziviani, J., & Dodrill, P. (2014). Features of feeding difficulty in children with autism spectrum disorder. International Journal of Speech Language Pathology, 16, 151–158.
Martin, A., Razza, R. A., & Brooks-Gunn, J. (2012). Specifying the links between household chaos and preschool children’s development. Early Child Development and Care, 182, 1247–1263.
Matson, J. L., Gardner, W. I., Coe, D. A., & Sovner, R. (1991). A scale for evaluating emotional disorders in severely and profoundly mentally retarded persons: Development of the diagnostic assessment for the severely handicapped (DASH) scale. British Journal of Psychiatry, 159, 81–89.
McCarthy, M. L., Silberstein, C. E., Atkins, E. A., Harryman, S. E., Sponseller, P. D., & Hadley Miller, N. A. (2002). Comparing reliability and validity of pediatric instruments for measuring health and well-being of children with spastic cerebral palsy. Developmental Medical Child Neurology, 44, 468–476.
McHorney, C. A., Robbins, J., Lomax, K., Rosenbek, J. C., Chignell, K., Kramer, A. E., & Bricker, D. E. (2002). The SWAL–QOL and SWAL–CARE outcomes tool for oropharyngeal dysphagia in adults: III documentation of reliability and validity. Dysphagia, 17, 97–114.
Nadon, G., Feldman, D. E., Dunn, W., & Gisel, E. (2011). Mealtime problems in children with autism spectrum disorder and their typically developing siblings: A comparison study. Autism, 15, 98–113.
Narayanan, U., Fehlings, D., Weir, S., Knight, S., Kiran, S., & Campbell, K. (2006). Initial development and validation of the caregiver priorities and child health index of life with disabilities (CPCHILD). Developmental Medical Child Neurology, 48, 804–812.
Palmer, S., Thompson, R. J., & Linscheid, T. R. (1975). Applied behavior analysis in the treatment of childhood feeding problems. Developmental Medicine and Child Neurology, 17, 333–339.
Parry, J. B. (1994). Merycism or rumination disorder: A historical investigation and current assessment. British Journal of Psychiatry, 165, 303–314.
Perske, R., Clifton, A., McClean, B. M., & Stein, J. I. (1977). Mealtimes for severely and profoundly handicapped persons: New concepts and attitudes. University Park Press.
Piazza-Waggoner, C., Driscoll, K. A., Gilman, D. K., & Powers, S. W. (2008). A comparison using parent report and direct observation of mealtime behaviors in young children with cystic fibrosis: Implications for practical and empirically based behavioral assessment in routine clinical care. Children’s Health Care, 37, 38–48.
Rajshree, S., & Manjula, R. 1991. Assessment Scale for cerebral palsied. A dissertation submitted as a part of fulfillment of Master’s degree (Speech Language Pathology), University of Mysore
Ramsay, M., Martel, C., Porporino, M., & Zygmuntowicz, C. (2011). The Montreal children’s hospital feeding scale: A brief bilingual screening tool for identifying feeding problems. Paediatrics & Child Health, 16, 147–151.
Schwarz, S. M. (2003). Feeding disorders in children with developmental disabilities.Infants and Young Children, 16, 317–330.
Silbergleit, A. K., Schultz, L., Jacobson, B. H., Beardsley, T., & Johnson, A. F. (2012). The dysphagia handicap index: Development and validation. Dysphagia, 27, 46–52.
Singhi, P., Kumar, M., Malhi, P., & Kumar, R. (2007). Utility of the WHO ten questions screen for disability detection in a rural community—the North Indian experience. Journal of Tropical Pediatrics, 53, 383–387.
Stallings, V. A., Zemal, B. S., Davies, J. C., Cronk, C. E., & Charney, E. B. (1996). Energy expenditure of children and adolescents with severe disabilities: A cerebral palsy model. The American Journal of Clinical Nutrition, 64, 627–634.
Swapna, N., & Anne Maria, A. (2019). Validation of feeding handicap index in adolescents with cerebral palsy. International Journal of Health Science and Research, 9(9), 206–214.
Swapna, N., & Shabnam, S. (2017). Manual of Feeding Handicap Index in children (FHI-C). All India Institute of Speech and Hearing
Trier, E., & Thomas, A. G. (1998). Feeding the disabled child. Nutrition, 14, 801–805.
Varni, J. W., Burwinkle, T. M., Berrin, S. J., Sherman, S. A., Ba, K. A., Malcarne, V. L., & Chambers, H. G. (2006). The PedsQL in pediatric cerebral palsy: Reliability, validity, and sensitivity of the generic core scales and cerebral palsy module. Developmental Medicine & Child Neurology, 48, 442–449.
Venkatesan, S. 2011. Socio Economic Status Scale-2011. Mysore: AIISH. Revised version of “NIMH Socio Economic Status Scale-1993”. NIMH
Wardle, J., Guthrie, C. A., Sanderson, S., & Rapoport, L. (2001). Development of the children’s eating behaviour questionnaire. The Journal of Child Psychology and Psychiatry and Allied Disciplines, 42, 963–970.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We declare no conflict of interest in the paper titled “Clinical Validation of Feeding Handicap Index for Children (FHI-C).”
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1
Feeding Handicap Index-Children (FHI-C)


Other Significant Findings
Rating Scale for Parent/Caregivers

Please circle the number that matches the severity of your child’s feeding difficulty (1- no difficulty at all; 4- some problem is present; 7- the worse problem my child could have).
Rating Scale for the Examiner

Appendix 2
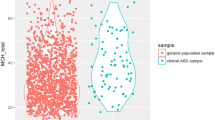
Mean and standard deviation (SD) values of FHI-C for the three clinical groups and the control group for the FHI-C domains and total FHI-C scores
Domains | FHI values | |||
|---|---|---|---|---|
CP group (n=60) | ASD group (n=61) | ID group (n=59) | Control group (n=60) | |
Physical | 15.91±8.79 | 8.41±6.42 | 9.31±6.571 | 1.68±2.20 |
Functional | 5.45±4.43 | 3.89±3.82 | 3.41±2.972 | 1.35±1.31 |
Emotional | 1.31±1.52 | 3.30±3.77 | 2.05±1.888 | 0.56±0.87 |
Total | 22.65±12.67 | 15.59±9.95 | 14.76±9.956 | 3.53±3.35 |
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shabnam, S., Swapna, N. Clinical Validation of Feeding Handicap Index for Children (FHI-C). J Autism Dev Disord 53, 4412–4423 (2023). https://doi.org/10.1007/s10803-022-05699-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-022-05699-5