Abstract
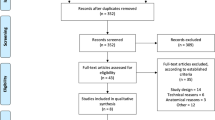
Different materials and techniques have been proposed for surgical repair of spontaneous middle cranial fossa (MCF) defects. However, conclusive evidence supporting their selection and impact on clinical outcomes is lacking. The study aims to conduct a systematic review and meta-analysis on materials and techniques employed to repair MCF defects and evaluate complications and rates of recurrent cerebrospinal fluid (CSF) leaks. A PRISMA-guided systematic review and meta-analysis were performed using MESH terms and specific keywords including studies published before May 2022. Primary outcomes included recurrence of CSF leak and complication rates by type of reconstructive material and technique utilized. Meta-analyses of proportions were performed using random effects and confidence intervals for individual proportions were calculated using the Clopper-Pearson method. Twenty-nine studies were included (n = 471 cases). Materials employed for repair were categorized according to defect size: 65% of defects were of unknown size, 24% were small (< 1 cm), and 11% were large (≥ 1 cm). Rigid reconstruction (RR) was significantly favored over soft reconstruction (SR) for larger defects (94% of cases, p < 0.05). Complications and recurrent CSF leak rates of SR and RR techniques were comparable for defects of all sizes (p > 0.05). Complication rates reported for these procedures are low regardless of technique and material. RR was universally preferred for larger defects and analysis of complication and recurrence rates did not reveal differences regardless of defect size. While RR was more frequently reported in smaller defects, SR was used by several centers, particularly for smaller MCF floor defects.








Similar content being viewed by others
Data availability
The authors confirm that the data supporting the findings of this study are available within the article and its supplementary materials.
Abbreviations
- CSF:
-
Cerebrospinal fluid
- JBI:
-
Joanna Briggs Institute
- MCF:
-
Middle cranial fossa
- MCFA:
-
Middle cranial fossa approach
- RR:
-
Rigid reconstruction
- SR:
-
Soft reconstruction
- TMA:
-
Transmastoid approach
References
Åhrén C, Thulin CA (1965) Lethal intracranial complications following inflation in the external auditory canal in treatment of serous otitis media and due to defects in the petrous bone. Acta Otolaryngol 60(1–6):407–421. https://doi.org/10.3109/00016486509127025
Gacek RR, Gacek MR, Tart R (1999) Adult spontaneous cerebrospinal fluid otorrhea: diagnosis and management. Am J Otol 20(6):770–776
Braca JA 3rd, Marzo S, Prabhu VC (2013) Cerebrospinal fluid leakage from tegmen tympani defects repaired via the middle cranial fossa approach. J Neurol Surg Part B, Skull Base 74(2):103–107. https://doi.org/10.1055/s-0033-1333616
Wind JJ, Caputy AJ, Roberti F (2008) Spontaneous encephaloceles of the temporal lobe. Neurosurg Focus 25(6):E11. https://doi.org/10.3171/foc.2008.25.12.E11
Sergi B, Passali GC, Picciotti PM, De Corso E, Paludetti G (2013) Transmastoid approach to repair meningoencephalic herniation in the middle ear. Acta Otorhinolaryngol Ital 33(2):97–101
Sonmez S, Sahin B, Polat B, Comoglu S, Orhan KS (2017) Repair of tegmen tympani defect presenting with spontaneous cerebrospinal fluid otorrhea using the middle cranial fossa approach. J Int Adv Otol 13(3):430–433. https://doi.org/10.5152/iao.2017.3386
Kutz JW Jr, Husain IA, Isaacson B, Roland PS (2008) Management of spontaneous cerebrospinal fluid otorrhea. Laryngoscope 118(12):2195–2199. https://doi.org/10.1097/MLG.0b013e318182f833
Lundy LB, Graham MD, Kartush JM, LaRouere MJ (1996) Temporal bone encephalocele and cerebrospinal fluid leaks. Am J Otol 17(3):461–469
Vivas EX, McCall A, Raz Y, Fernandez-Miranda JC, Gardner P, Hirsch BE (2014) ICP, BMI, surgical repair, and CSF diversion in patients presenting with spontaneous CSF otorrhea. Otol Neurotol 35(2):344–347. https://doi.org/10.1097/MAO.0b013e3182a473cf
Semaan MT, Wick CC, Kinder KJ, Stuyt JG, Chota RL, Megerian CA (2016) Retrosigmoid versus translabyrinthine approach to acoustic neuroma resection: a comparative cost-effectiveness analysis. Laryngoscope 126(Suppl 3):S5-12. https://doi.org/10.1002/lary.25729
Nahas Z, Tatlipinar A, Limb CJ, Francis HW (2008) Spontaneous meningoencephalocele of the temporal bone: clinical spectrum and presentation. Arch Otolaryngol Head Neck Surg 134(5):509–518. https://doi.org/10.1001/archotol.134.5.509
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 372:n71. https://doi.org/10.1136/bmj.n71
Khan A, Lapin A, Eisenman DJ (2014) Use of titanium mesh for middle cranial fossa skull base reconstruction. J Neurol Surg B Skull Base 75(2):104–109. https://doi.org/10.1055/s-0033-1358792
Acharya AN, Rajan GP (2015) Piezosurgery for the repair of middle cranial fossa meningoencephaloceles. Otol Neurotol 36(3):444–447. https://doi.org/10.1097/MAO.0000000000000645
Gonen L, Handzel O, Shimony N, Fliss DM, Margalit N (2016) Surgical management of spontaneous cerebrospinal fluid leakage through temporal bone defects—case series and review of the literature. Neurosurg Rev 39(1):141–50
Roehm PC, Tint D, Chan N, Brewster R, Sukul V, Erkmen K (2018) Endoscope-assisted repair of CSF otorrhea and temporal lobe encephaloceles via keyhole craniotomy. J Neurosurg 128(6):1880–1884. https://doi.org/10.3171/2017.1.JNS161947
McNulty B, Schutt CA, Bojrab D, Babu S (2020) Middle cranial fossa encephalocele and cerebrospinal fluid leakage: etiology, approach, outcomes. J Neurol Surg B Skull Base 81(3):268–274. https://doi.org/10.1055/s-0039-1688793
Semaan MT, Gilpin DA, Hsu DP, Wasman JK, Megerian CA (2011) Transmastoid extradural-intracranial approach for repair of transtemporal meningoencephalocele: a review of 31 consecutive cases. Laryngoscope 121(8):1765–1772. https://doi.org/10.1002/lary.21887
Wong AK, Shinners M, Wong RH (2020) Minimally invasive repair of tegmen defects through keyhole middle fossa approach to reduce hospitalization. World Neurosurg 133:e683–e689. https://doi.org/10.1016/j.wneu.2019.09.114
Hoang S, Ortiz Torres MJ, Rivera AL, Litofsky NS (2018) Middle cranial fossa approach to repair tegmen defects with autologous or alloplastic graft. World Neurosurg 118:e10–e17. https://doi.org/10.1016/j.wneu.2018.05.196
Sanna M, Fois P, Russo A, Falcioni M (2009) Management of meningoencephalic herniation of the temporal bone: personal experience and literature review. Laryngoscope 119(8):1579–1585. https://doi.org/10.1002/lary.20510
Dutt SN, Mirza S, Irving RM (2001) Middle cranial fossa approach for the repair of spontaneous cerebrospinal fluid otorrhoea using autologous bone pate. Clin Otolaryngol Allied Sci 26(2):117–123. https://doi.org/10.1046/j.1365-2273.2001.00438.x
Nguyen D, Deitrick J, Sessions W, Nguyen T (2018) Tegmen tympani cerebrospinal fluid leakage repair: transmastoid approach utilizing Stryker bone cement. J Med Cases 9(3):96–7. https://doi.org/10.14740/jmc3009w
Alwani MM, Saltagi MZ, MacPhail ME, Nelson RF (2021) Middle cranial fossa repair of temporal bone spontaneous CSF leaks with hydroxyapatite bone cement. Laryngoscope 131(3):624–632. https://doi.org/10.1002/lary.28761
Scullen T, Freeman Z, Mathkour M, Lockwood J, Aslam R, Jackson N et al (2021) Middle fossa encephaloceles treated via the transmastoid approach: a case series and review of the literature. Oper Neurosurg (Hagerstown) 21(5):332–342. https://doi.org/10.1093/ons/opab276
Patel A, Zakaria J, Bartindale MR, Germanwala AV, Anderson DE, Marzo SJ et al (2021) Fetal bovine collagen grafts for repair of tegmen defects and encephaloceles via middle cranial fossa approach. Ear Nose Throat J 100(3_suppl):347S–51S. https://doi.org/10.1177/0145561320906906
Marchioni D, Bonali M, Alicandri-Ciufelli M, Rubini A, Pavesi G, Presutti L (2014) Combined approach for tegmen defects repair in patients with cerebrospinal fluid otorrhea or herniations: our experience. J Neurol Surg Part B, Skull base 75(4):279–287. https://doi.org/10.1055/s-0034-1371524
Kuhweide R, Casselman JW (1999) Spontaneous cerebrospinal fluid otorrhea from a tegmen defect: transmastoid repair with minicraniotomy. Ann Otol Rhinol Laryngol 108(7 Pt 1):653–658. https://doi.org/10.1177/000348949910800706
Mayeno JK, Korol HW, Nutik SL (2004) Spontaneous meningoencephalic herniation of the temporal bone: case series with recommended treatment. Otolaryngol Head Neck Surg 130(4):486–489. https://doi.org/10.1016/j.otohns.2003.09.022
Scurry WC Jr, Ort SA, Peterson WM, Sheehan JM, Isaacson JE (2007) Idiopathic temporal bone encephaloceles in the obese patient. Otolaryngol Head Neck Surg 136(6):961–965. https://doi.org/10.1016/j.otohns.2006.11.036
Hernandez-Montero E, Caballero E, García-Ibanez L (2020) Surgical management of middle cranial fossa bone defects: meningoencephalic herniation and cerebrospinal fluid leaks. Am J Otolaryngol 41(4):102560. https://doi.org/10.1016/j.amjoto.2020.102560
Leonetti JP, Marzo S, Anderson D, Origitano T, Vukas DD (2005) Spontaneous transtemporal CSF leakage: a study of 51 cases. Ear Nose Throat J 84(11):700–706
Brown NE, Grundfast KM, Jabre A, Megerian CA, O’Malley BW Jr, Rosenberg SI (2004) Diagnosis and management of spontaneous cerebrospinal fluid-middle ear effusion and otorrhea. Laryngoscope 114(5):800–805. https://doi.org/10.1097/00005537-200405000-00002
Alwan M, Ibbett I, Pullar M, Lai LT, Gordon M (2019) Hearing improvement following middle cranial fossa floor defect repair utilizing a modified middle fossa approach and reconstructive techniques. Otol Neurotol 40(8):1034–1039. https://doi.org/10.1097/MAO.0000000000002322
Boo SH, Goh YB, Han CS (2013) Repair of spontaneous cerebrospinal fluid otorrhea from defect of middle cranial fossa. Korean J Audiol 17(3):148–151. https://doi.org/10.7874/kja.2013.17.3.148
Kari E, Mattox DE (2011) Transtemporal management of temporal bone encephaloceles and CSF leaks: review of 56 consecutive patients. Acta Otolaryngol 131(4):391–394. https://doi.org/10.3109/00016489.2011.557836
Gubbels SP, Selden NR, Delashaw JB Jr, McMenomey SO (2007) Spontaneous middle fossa encephalocele and cerebrospinal fluid leakage: diagnosis and management. Otol Neurotol 28(8):1131–1139. https://doi.org/10.1097/MAO.0b013e318157f7b6
Kenning TJ, Willcox TO, Artz GJ, Schiffmacher P, Farrell CJ, Evans JJ (2012) Surgical management of temporal meningoencephaloceles, cerebrospinal fluid leaks, and intracranial hypertension: treatment paradigm and outcomes. Neurosurg Focus 32(6):E6. https://doi.org/10.3171/2012.4.Focus1265
Souliere CR Jr, Langman AW (1998) Combined mastoid/middle cranial fossa repair of temporal bone encephalocele. Skull Base Surg 8(4):185–189. https://doi.org/10.1055/s-2008-1058181
Rao AK, Merenda DM, Wetmore SJ (2005) Diagnosis and management of spontaneous cerebrospinal fluid otorrhea. Otol Neurotol 26(6):1171–1175. https://doi.org/10.1097/01.mao.0000179526.17285.cc
Kim L, Wisely CE, Dodson EE (2014) Transmastoid approach to spontaneous temporal bone cerebrospinal fluid leaks: hearing improvement and success of repair. Otolaryngol Head Neck Surg 150(3):472–478. https://doi.org/10.1177/0194599813518173
King JD, Hamilton DH, Jacobs CA, Duncan ST (2018) The hidden cost of commercial antibiotic-loaded bone cement: a systematic review of clinical results and cost implications following total knee arthroplasty. J Arthroplasty 33(12):3789–3792. https://doi.org/10.1016/j.arth.2018.08.009
Braca JA 3rd, Marzo S, Prabhu VC (2013) Cerebrospinal fluid leakage from tegmen tympani defects repaired via the middle cranial fossa approach. J Neurol Surg B Skull Base 74(2):103–107. https://doi.org/10.1055/s-0033-1333616
Jeevan DS, Ormond DR, Kim AH, Meiteles LZ, Stidham KR, Linstrom C et al (2015) Cerebrospinal fluid leaks and encephaloceles of temporal bone origin: nuances to diagnosis and management. World Neurosurg 83(4):560–566. https://doi.org/10.1016/j.wneu.2014.12.011
Author information
Authors and Affiliations
Contributions
Conceptualization, methodology, and investigation: E. P., H. S., J. M. R. B., and G. P. Formal analysis: N. V., D. E. M., E. X. V., and G. P. Writing — original draft preparation: E. P., H. S., I. P., and M. P. Statistical analyses: I. P. and M. P. Writing — review and editing: E. P., H. S., C. A. S., and T. G. M. Final supervision: E. P., H. S., and G. P.
Corresponding author
Ethics declarations
Competing interests
Authors associated with this submission do have financial conflicts of interest to disclose: Gustavo Pradilla is a consultant for Stryker Corporation and C. Arturo Solares is a consultant for Stryker Corporation. The other authors do not have financial disclosures.
Ethical approval
Not applicable.
Conflict of interest
Gustavo Pradilla is a consultant for Stryker Corporation. C. Arturo Solares is a consultant for Medtronic. The other authors do not have financial disclosures.
Additional information
Submission statement
The contents of this manuscript have not been copyrighted or published previously.
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Edoardo Porto and Hanyao Sun are first co-authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Porto, E., Sun, H., Revuelta-Barbero, J.M. et al. Surgical management of spontaneous middle cranial fossa defects: a systematic review and meta-analysis of available reconstructive techniques and materials. Neurosurg Rev 46, 41 (2023). https://doi.org/10.1007/s10143-023-01947-z
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10143-023-01947-z