Abstract
Objective
To determine the predictive value of the neutrophil-to-lymphocyte ratio (NLR), lymphocyte-to-monocyte ratio (LMR), neutrophil-to-eosinophil ratio (NER), lymphocyte-to-eosinophil ratio (LER), monocyte-to-eosinophil ratio (MER), systemic inflammatory response index (SIRI), and ratio of inflammatory cells before and after treatment for predicting survival in advanced nasopharyngeal carcinoma (NPC) and to provide a reference for treatment.
Methods
A retrospective review of 70 patients was performed. Serological indexes were obtained by drawing blood before and after systemic therapy. The cutoff values of these indexes were determined by receiver operating characteristic (ROC) curves. The prognostic value of the indexes for overall survival (OS) and distant metastasis free survival (DMFS) was evaluated.
Results
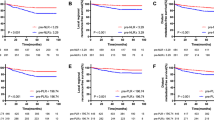
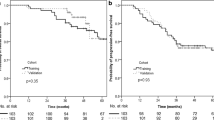
Survival analysis showed that a smaller pretreatment LMR value was associated with poor OS; larger pretreatment NER, LER, MER, and SIRI values were associated with poor OS; a smaller posttreatment LMR value was associated with poor OS; larger posttreatment NLR, NER, MER, and SIRI values were associated with poor OS; a smaller pretreatment LMR value was associated with poor DMFS; larger pretreatment NLR, NER, LER, and MER values were associated with poor DMFS; and larger posttreatment NLR, NER, LER, and MER values were associated with poor DMFS. Furthermore, a larger neutrophil after treatment-to-neutrophil before treatment ratio was associated with poor OS and DMFS. Logistic regression analysis showed that pretreatment MER and posttreatment NLR were independent predictors of OS in patients with advanced NPC; moreover, pretreatment and posttreatment MER and NLR were independent prognostic factors for DMFS in patients with advanced NPC.
Conclusions
The NLR, NER and MER can be used to predict survival in advanced NPC patients. Eosinophils might be one of the factors for the good prognosis of NPC patients. In addition, an increased number of neutrophils after treatment may indicate a favorable prognosis.








Similar content being viewed by others
Availability of data and materials
All data will be made available by the corresponding author upon reasonable request.
References
Chen YP, Chan ATC, Le QT et al (2019) Nasopharyngeal carcinoma. Lancet 394(10192):64–80. https://doi.org/10.1016/S0140-6736(19)30956-0
Zhong L, Dong D, Fang X et al (2021) A deep learning-based radiomic nomogram for prognosis and treatment decision in advanced nasopharyngeal carcinoma: a multicentre study. EBioMedicine. 70:103522. https://doi.org/10.1016/j.ebiom.2021.103522
Pan JJ, Ng WT, Zong JF et al (2016) Prognostic nomogram for refining the prognostication of the proposed 8th edition of the AJCC/UICC staging system for nasopharyngeal cancer in the era of intensity-modulated radiotherapy. Cancer. 122(21):3307–3315. https://doi.org/10.1002/cncr.30198
Sun X, Su S, Chen C et al (2014) Long-term outcomes of intensity-modulated radiotherapy for 868 patients with nasopharyngeal carcinoma: an analysis of survival and treatment toxicities. Radiother Oncol 110(3):398–403. https://doi.org/10.1016/j.radonc.2013.10.020
Pfister DG, Spencer S, Adelstein D et al (2020) Head and neck cancers, version 2020, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 18(7):873–898. https://doi.org/10.6004/jnccn.2020.0031
Chen YP, Wang ZX, Chen L et al (2015) A Bayesian network meta-analysis comparing concurrent chemoradiotherapy followed by adjuvant chemotherapy, concurrent chemoradiotherapy alone and radiotherapy alone in patients with locoregionally advanced nasopharyngeal carcinoma. Ann Oncol 26(1):205–211. https://doi.org/10.1093/annonc/mdu507
Hong X, Liu N, Liang Y et al (2020) Circular RNA CRIM1 functions as a ceRNA to promote nasopharyngeal carcinoma metastasis and docetaxel chemoresistance through upregulating FOXQ1. Mol Cancer 19(1):33. https://doi.org/10.1186/s12943-020-01149-x
Wu G, Yao Y, Bai C et al (2015) Combination of platelet to lymphocyte ratio and neutrophil to lymphocyte ratio is a useful prognostic factor in advanced non-small cell lung cancer patients. Thorac Cancer. 6(3):275–87. https://doi.org/10.1111/1759-7714.12178
Yapar A, Tokgöz MA, Yapar D et al (2021) Diagnostic and prognostic role of neutrophil/lymphocyte ratio, platelet/lymphocyte ratio, and lymphocyte/monocyte ratio in patients with osteosarcoma. Jt Dis Relat Surg. 32(2):489–496. https://doi.org/10.52312/jdrs.2021.79775
Miyahara Y, Takashi S, Shimizu Y et al (2020) The prognostic impact of neutrophil-to-lymphocyte ratio (NLR) and lymphocyte-to-monocyte ratio (LMR) in patients with distal bile duct cancer. World J Surg Oncol 18(1):78. https://doi.org/10.1186/s12957-020-01847-2.PMID:32321522;PMCID:PMC7178599
Xia LJ, Li W, Zhai JC et al (2020) Significance of neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, lymphocyte-to-monocyte ratio and prognostic nutritional index for predicting clinical outcomes in T1–2 rectal cancer. BMC Cancer 20(1):208. https://doi.org/10.1186/s12885-020-6698-6
Lu A, Li H, Zheng Y et al (2017) Prognostic significance of neutrophil to lymphocyte ratio, lymphocyte to monocyte ratio, and platelet to lymphocyte ratio in patients with nasopharyngeal carcinoma. Biomed Res Int. 2017:3047802. https://doi.org/10.1155/2017/3047802
Chen Y, Sun J, Hu D et al (2021) Predictive value of pretreatment lymphocyte-to-monocyte ratio and platelet-to-lymphocyte ratio in the survival of nasopharyngeal carcinoma patients. Cancer Manag Res 23(13):8767–8779. https://doi.org/10.2147/CMAR.S338394
Rosenberg HF, Dyer KD, Foster PS (2013) Eosinophils: changing perspectives in health and disease. Nat Rev Immunol. 13(1):9–22. https://doi.org/10.1038/nri3341
Rothenberg ME, Hogan SP (2006) The eosinophil. Annu Rev Immunol 24:147–174. https://doi.org/10.1146/annurev.Immunol.24.021605.090720
Ownby HE, Roi LD, Isenberg RR et al (1983) Peripheral lymphocyte and eosinophil counts as indicators of prognosis in primary breast cancer. Cancer 52(1):126–130. https://doi.org/10.1002/1097-0142(19830701)52:1%3c126::aid-cncr2820520123%3e3.0.co;2-y
Ishibashi S, Ohashi Y, Suzuki T et al (2006) Tumor-associated tissue eosinophilia in human esophageal squamous cell carcinoma. Anticancer Res. 26(2B):1419–24
von Wasielewski R, Seth S, Franklin J, Fischer R, Hübner K et al (2000) Tissue eosinophilia correlates strongly with poor prognosis in nodular sclerosing Hodgkin’s disease, allowing for known prognostic factors. Blood 95(4):1207–1213
Zhang MX, Wang L, Zeng L et al (2021) LCN2 is a potential biomarker for radioresistance and recurrence in nasopharyngeal carcinoma. Front Oncol 2(10):605777. https://doi.org/10.3389/fonc.2020.605777
Andersson-Anvret M, Forsby N, Klein G et al (1977) Relationship between the Epstein-Barr virus and undifferentiated nasopharyngeal carcinoma: correlated nucleic acid hybridization and histopathological examination. Int J Cancer 20(4):486–494. https://doi.org/10.1002/ijc.2910200403
Lin DC, Meng X, Hazawa M et al (2014) The genomic landscape of nasopharyngeal carcinoma. Nat Genet 46(8):866–871. https://doi.org/10.1038/ng.3006
Ward MH, Pan WH, Cheng YJ et al (2000) Dietary exposure to nitrite and nitrosamines and risk of nasopharyngeal carcinoma in Taiwan. Int J Cancer 86(5):603–609. https://doi.org/10.1002/(SICI)1097-0215(20000601)86:5%3c603::AID-IJC1%3e3.0.CO;2-H
Lam WKJ, Chan JYK (2018) Recent advances in the management of nasopharyngeal carcinoma. F1000Res. 7:1829. https://doi.org/10.12688/f1000research.15066.1
Si Y, Xu J, Meng L, Wu Y et al (2022) Role of STAT3 in the pathogenesis of nasopharyngeal carcinoma and its significance in anticancer therapy. Front Oncol 13(12):1021179. https://doi.org/10.3389/fonc.2022.1021179.PMID:36313702;PMCID:PMC9615247
Balkwill F, Mantovani A (2001) Inflammation and cancer: back to Virchow? Lancet 357(9255):539–545. https://doi.org/10.1016/S0140-6736(00)04046-0
Mantovani A, Allavena P, Sica A, Balkwill F (2008) Cancer-related inflammation. Nature 454(7203):436–444. https://doi.org/10.1038/nature07205
Ye L, Oei RW, Kong F et al (2018) Prognostic values of hematological biomarkers in nasopharyngeal carcinoma patients treated with intensity-modulated radiotherapy. Eur Arch Otorhinolaryngol. 275(5):1309–1317. https://doi.org/10.1007/s00405-018-4956-x
Schreiber RD, Old LJ, Smyth MJ (2011) Cancer immunoediting: integrating immunity’s roles in cancer suppression and promotion. Science 331:1565–1570. https://doi.org/10.1126/science.1203486
Demers M, Wagner DD (2013) Neutrophil extracellular traps: a new link to cancer-associated thrombosis and potential implications for tumor progression. Oncoimmunology 2(2):e22946. https://doi.org/10.4161/onci.22946
Germano G, Allavena P, Mantovani A (2008) Cytokines as a key component of cancer-related inflammation. Cytokine 43(3):374–379. https://doi.org/10.1016/j.cyto.2008.07.014
Li JP, Chen SL, Liu XM et al (2016) A Novel inflammation-based stage (I stage) predicts overall survival of patients with nasopharyngeal carcinoma. Int J Mol Sci 17(11):1900. https://doi.org/10.3390/ijms17111900
Kim J, Bae JS (2016) Tumor-associated macrophages and neutrophils in tumor microenvironment. Mediators Inflamm 2016:6058147. https://doi.org/10.1155/2016/6058147
Zeng Z, Xu S, Wang D et al (2022) Prognostic significance of systemic immune-inflammation index in patients with nasopharyngeal carcinoma: a meta-analysis. Syst Rev 11(1):247. https://doi.org/10.1186/s13643-022-02123-y
Wen S, Chen N, Hu Y et al (2021) Elevated peripheral absolute monocyte count related to clinicopathological features and poor prognosis in solid tumors: Systematic review, meta-analysis, and meta-regression. Cancer Med. 10(5):1690–1714. https://doi.org/10.1002/cam4.3773
Arwert EN, Harney AS, Entenberg D et al (2018) A unidirectional transition from migratory to perivascular macrophage is required for tumor cell intravasation. Cell Rep 23(5):1239–1248. https://doi.org/10.1016/j.celrep.2018.04.007
Chanmee T, Ontong P, Konno K et al (2014) Tumor-associated macrophages as major players in the tumor microenvironment. Cancers (Basel) 6(3):1670–1690. https://doi.org/10.3390/cancers6031670
Varricchi G, Galdiero MR, Loffredo S et al (2017) Eosinophils: the unsung heroes in cancer? Oncoimmunology 7(2):e1393134. https://doi.org/10.1080/2162402X.2017.1393134
Galdiero MR, Garlanda C, Jaillon S et al (2013) Tumor associated macrophages and neutrophils in tumor progression. J Cell Physiol. 228(7):1404–1412. https://doi.org/10.1002/jcp.24260
Galdiero MR, Marone G, Mantovani A (2017) Cancer inflammation and cytokines. Cold Spring Harb Perspect Biol. https://doi.org/10.1101/cshperspect.a028662
Carretero R, Sektioglu IM, Garbi N et al (2015) Eosinophils orchestrate cancer rejection by normalizing tumor vessels and enhancing infiltration of CD8(+) T cells. Nat Immunol. 16(6):609–617. https://doi.org/10.1038/ni.3159
Biswas SK, Mantovani A (2010) Macrophage plasticity and interaction with lymphocyte subsets: cancer as a paradigm. Nat Immunol. 11(10):889–896. https://doi.org/10.1038/ni.1937
Lucarini V, Ziccheddu G, Macchia I et al (2017) IL-33 restricts tumor growth and inhibits pulmonary metastasis in melanoma-bearing mice through eosinophils. Oncoimmunology. 6(6):e1317420. https://doi.org/10.1080/2162402x.2017.1317420
Esposito I, Menicagli M, Funel N, Bergmann F et al (2004) Inflammatory cells contribute to the generation of an angiogenic phenotype in pancreatic ductal adenocarcinoma. J Clin Pathol. 57(6):630–636. https://doi.org/10.1136/jcp.2003.014498
Funding
This work was supported by grants from the Natural Science Foundations of Hunan province, China [2021JJ40913].
Author information
Authors and Affiliations
Contributions
MY: data acquisition, interpretation, analysis, drafting; AH: data acquisition, interpretation; BY: data acquisition, interpretation; GT: interpretation, revisions; JA: interpretation, revisions; HL: conception, interpretation, revisions.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no potential conflicts of interest.
Ethical approval and consent to participate
The study protocol was approved by the Ethics Committee of The Third Xiangya Hospital (No: 21182) and performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ye, M., Huang, A., Yuan, B. et al. Neutrophil-to-lymphocyte ratio and monocyte-to-eosinophil ratio as prognostic indicators for advanced nasopharyngeal carcinoma. Eur Arch Otorhinolaryngol 281, 1971–1989 (2024). https://doi.org/10.1007/s00405-024-08474-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-024-08474-7