Abstract
Introduction
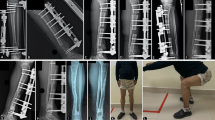
The treatment of segmental tibial bone defects remains a surgical challenge. While Bone Transport (BT) and Induced Membrane Technique (IMT) are effective strategies for regenerating bone, there are few comparative studies between them. This investigation undertakes a comparative analysis of BT and IMT for large segmental tibial defects stabilised through plate fixation.
Materials and methods
Patients with segmental tibial defects exceeding 5 cm were prospectively enrolled from 2008 to 2021 in a single institution, with a minimum follow-up duration of two years. All patients underwent either BT or IMT with plate fixation of the tibia. Procedural success, primary union as well as bone and functional outcome scores were compared. Complications, including non-unions, joint contractures and deep infections requiring surgical intervention, were also compared.
Results
41 patients were recruited in total. 28 patients underwent Bone Transport Over a Plate (BTOP), while 13 patients underwent IMT with Plate fixation (IMTP). The procedural success rate trended higher in IMTP compared to BTOP (100% vs. 85.7%). The primary union rate also trended higher in IMTP compared to BTOP (92.3% vs. 79.2%). BTOP and IMTP achieved similar rates of satisfactory bone outcome scores (78.6% vs. 84.6%) and functional outcome scores (75% vs. 76.5%). There was no statistical difference between procedural success, primary union, bone and functional outcome scores. The complication rate in BTOP was 78.6% (22 of 28), including five docking site or regenerate non-unions, eight deep infections and nine joint contractures. IMTP had a 38.5% (5 of 13) complication rate, including one non-union, two deep infections and two joint contractures. The complication rate was 2.04 times higher in BTOP compared to IMTP (p = 0.0117).
Conclusions
BTOP and IMTP are both equally effective techniques for regenerating bone in large tibial bone defects. However, IMTP may be a safer procedure than BTOP, with a lower probability of requiring additional procedures to address complications.


Similar content being viewed by others
References
Ilizarov GA (1988 Spring) The principles of the Ilizarov method. Bull Hosp Jt Dis Orthop Inst 48(1):1–11
Aktuglu K, Erol K, Vahabi A (2019) Ilizarov bone transport and treatment of critical-sized tibial bone defects: a narrative review. J Orthop Traumatol 20(1):22. https://doi.org/10.1186/s10195-019-0527-1
Park KH, Oh CW, Kim JW et al (2021) Matched comparison of bone transport using external Fixator over a nail Versus External Fixator over a plate for segmental tibial bone defects. J Orthop Trauma 35(11):e397–e404. https://doi.org/10.1097/BOT.0000000000002084
Masquelet AC, Fitoussi F, Begue T et al (2000) Reconstruction Des os longs par membrane Induite et autogreffe spongieuse [Reconstruction of the long bones by the induced membrane and spongy autograft]. Ann Chir Plast Esthet 45(3):346–353
Griffin JT, Landy DC, Sneed CR et al (2023) Masquelet technique for the Tibia: a systematic review and Meta-analysis of contemporary outcomes. J Orthop Trauma 37(1):e36–e44. https://doi.org/10.1097/BOT.0000000000002480
Rohilla R, Sharma PK, Wadhwani J et al (2022) Prospective randomized comparison of bone transport versus Masquelet technique in infected gap nonunion of tibia. Arch Orthop Trauma Surg 142(8):1923–1932. https://doi.org/10.1007/s00402-021-03935-8
Tong K, Zhong Z, Peng Y et al (2017) Masquelet technique versus Ilizarov bone transport for reconstruction of lower extremity bone defects following posttraumatic osteomyelitis. Injury 48(7):1616–1622. https://doi.org/10.1016/j.injury.2017.03.042
Ren C, Li M, Ma T et al (2022 May-Aug) A meta-analysis of the Masquelet technique and the Ilizarov bone transport method for the treatment of infected bone defects in the lower extremities. J Orthop Surg (Hong Kong) 30(2):10225536221102685. https://doi.org/10.1177/10225536221102685
Zhang H, Zhao X, Yang X et al (2023) Comparison of internal and external fixation after debridement in the Masquelet technique for Cierny-Mader type IV tibial post-traumatic osteomyelitis. Injury 54(2):422–428. https://doi.org/10.1016/j.injury.2022.11.030
Kocaoglu M, Eralp L, Rashid HU et al (2006) Reconstruction of segmental bone defects due to chronic osteomyelitis with use of an external fixator and an intramedullary nail. J Bone Joint Surg Am 88(10):2137–2145. https://doi.org/10.2106/JBJS.E.01152
Allesina L, Alessio-Mazzola M, Belluati A, Mosca S, Placella G, Salini V (2023) Surgical treatment of critical size bone defects with Masquelet technique versus bone transport: a systematic review and meta-analysis of comparative studies. Arch Orthop Trauma Surg 143(12):7081–7096. https://doi.org/10.1007/s00402-023-05049-9
El-Alfy BS, Ali AM (2015 Nov-Dec) Management of segmental skeletal defects by the induced membrane technique. Indian J Orthop 49(6):643–648. https://doi.org/10.4103/0019-5413.168757
Madhusudhan TR, Ramesh B, Manjunath K et al (2008) Outcomes of Ilizarov ring fixation in recalcitrant infected tibial non-unions - a prospective study. J Trauma Manag Outcomes 2(1):6. 10.118
Lotzien S, Rosteius T, Reinke C et al (2021) Reconstruction of Septic tibial bone defects with the Masquelet technique and External Ring Fixation-A low Healing Rate and High Complication and Revision Rates. J Orthop Trauma 35(9):e328–e336. https://doi.org/10.1097/BOT.0000000000002065
Sbitany H, Au AF, Kovach SJ et al (2013) Orthoplastic approach to composite tissue loss. In: Pu LLQ, Levine JP, Wei FC (eds) Reconstructive surgery of the Lower Extremity, 1st edn. Quality Medical Publishing Inc, St. Louis, MO, pp 1025–1045
Wen H, Zhu S, Li C et al (2020) Bone transport versus acute shortening for the management of infected tibial bone defects: a meta-analysis. BMC Musculoskelet Disord 21(1):80. https://doi.org/10.1186/s12891-020-3114-y
Fung B, Hoit G, Schemitsch E et al (2020) The induced membrane technique for the management of long bone defects. Bone Joint J 102–B(12):1723–1734. https://doi.org/10.1302/0301-620X.102B12.BJJ-2020-1125.R1
Azi M, Teixeira AA, Cotias RB et al (2016) Membrane Induced Osteogenesis in the management of posttraumatic bone defects. J Orthop Trauma 30(10):545–550. https://doi.org/10.1097/BOT.000000000000061402;10
Corona PS, Carbonell-Rosell C, Vicente M et al (2022) Three-stage limb salvage in tibial fracture related infection with composite bone and soft-tissue defect. Arch Orthop Trauma Surg 142(12):3877–3887. https://doi.org/10.1007/s00402-021-04299-9
Simpson AH, Deakin M, Latham JM (2001) Chronic osteomyelitis. The effect of the extent of surgical resection on infection-free survival. J Bone Joint Surg Br 83(3):403–407. https://doi.org/10.1302/0301-620x.83b3.10727
Yoon YC, Oh CW, Cho JW et al (2021) Early definitive internal fixation for infected nonunion of the lower limb. J Orthop Surg Res 16(1):632. https://doi.org/10.1186/s13018-021-02785-9
Paley D (1990) Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res. ;(250):81–104
Acknowledgements
This research was supported by a grant of Korea Health Technology R&D Project through the Korea Heath Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HR22C1832).
Funding
No funding was provided for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical review statement
This study received approval from Institutional Review Board (IRB No: KNUH 2023-07-042).
Disclosure
The authors do not have any financial or personal conflicts of interest to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Seng, D.W., Oh, CW., Kim, JW. et al. Induced membrane technique with plate fixation has a lower complication rate than bone transport over a plate for segmental tibial defects larger than 5 cm. Arch Orthop Trauma Surg 144, 1881–1888 (2024). https://doi.org/10.1007/s00402-024-05262-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-024-05262-0