Review Article -Traumatic elbow dislocations

Abstract
Elbow dislocations occur mostly in the young adult population and nearly 50% occur during sporting activities. Diagnosis and assessment of concentric reduction following manipulation are performed using plain radiography and fluoroscopy. Computed Tomography (CT) enable identifying subtle fractures that can otherwise lead to chronic instability. Simple dislocations by definition have no associated fractures and complex dislocations are associated with a variety of fractures, with the terrible triad injury and trans-humeral dislocations leading to surgical challenges.
Assessment of the direction and the mechanics of elbow dislocation enable identify the structures that have been injured. Posterior and posterolateral dislocations are the most common patterns, where the lateral ligament complex is often compromised. Most simple dislocations are amenable to reduction, immobilization, and gradual rehabilitation resulting in good functional outcome. Ongoing instability can occur in 10% of the patients. Complex dislocations pose a surgical challenge and lead to joint stiffness, pain and ongoing instability if not managed properly. Identifying the individual component of a complex dislocation such as radial head fractures, coronoid fractures, proximal ulnar fractures, and ligament injures is important for satisfactory outcome.
Article
Traumatic elbow dislocations
Authors;
Melanie Amarasooriya1,2, Supun Gamage3, Udesh Somarathne3, Salinda Pathirana3
- Consultant Orthopaedic Surgeon, National Hospital Sri Lanka.
- Lecturer/Academic Consultant, University of Moratuwa, Sri Lanka
- Registrar, Orthopaedic Surgery, National Hospital Sri Lanka.
ORCID https://orcid.org/0000-0002-5629-543X
DOI; https://doi.org/10.62474/FGDB3996
Introduction
The elbow is the second most common joint to dislocate in adults after the shoulder joint (1). The reported incidence is 2.9 to 5.1 dislocations per 100,000 population per year (2). Among children, the elbow is recognized as the most common joint to dislocate, with 45% of the dislocations occurring in the age group between 10 to 19 years. The incidence is higher among males (3) and the high energy mechanisms are the usual cause. Elderly females can present with low-velocity falls resulting in elbow dislocations. Approximately 50% of elbow dislocations occur due to athletic activities, specifically during competition rather than during practice (2). Healthcare costs following elbow injury cannot be underestimated. The direct medical cost associated with elbow dislocations varies between populations. A study from Taiwan reported that the medical cost per patient with simple or complex dislocation is USD 508 per patient (4). A study conducted by the National Health Service (NHS) United Kingdom reported an average cost of GBP 1088 per patient (5).
image
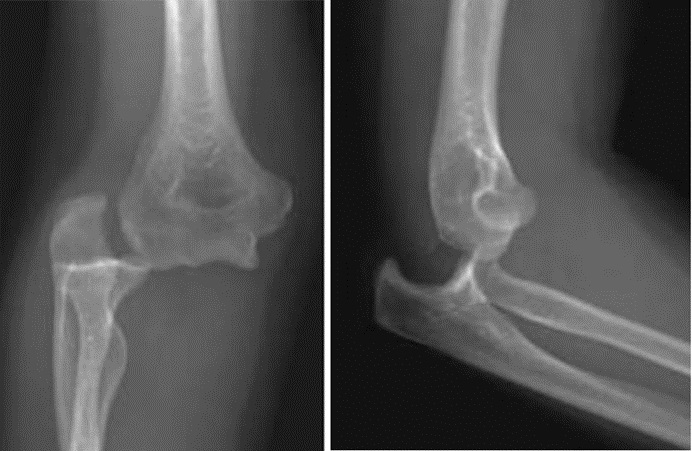
Figure 1 Simple elbow dislocation. From “The Assessment and Management of Simple Elbow Dislocations ” by Grazette AJ; Aquilina A. Open Orthop J. 2017 Nov 30; 11:1373-1379. [used under Creative Commons CC-BY license].
Applied anatomy
The elbow is stabilized by both static (osseous and soft tissue) and dynamic mechanisms (6). The static mechanisms include the osseous congruity of the ulna-humeral joint and the medial and lateral ligament complexes. The elbow flexion angle affects the stability provided by these osseous and soft tissue structures (6). Bony stability is maximum at <20° and >120° of flexion(7). Soft tissue structures like static medial and lateral collateral ligament complexes are dynamically supported by muscular stabilizers; common flexor and extensor origins, the biceps brachii and triceps brachii. The anterior bundle of the medial collateral ligament (aMCL) is the primary stabilizer against valgus strain at 30°-110° of flexion. The anterior bundle is mainly active during extension and early flexion whereas the posterior bundle becomes the principal stabilizer from 60° to full flexion (6).
The lateral ligament complex resists excessive varus and external rotation forces on the elbow (8). The lateral ligament complex consists of an annular ligament, lateral/ radial collateral ligament, and lateral ulnar collateral ligament (LUCL). LUCL originates at the lateral humeral epicondyle, partly blends with the annular ligament, and inserts at the supinator crest of the ulnar. About 30% of the population has an accessory lateral collateral ligament extending from the annular ligament to the supinator crest of the ulna (8).
Applied biomechanics
Falling on an outstretched hand during sporting events or high-velocity trauma is the most common mechanism that leads to elbow dislocation. The most common directions of dislocation are posterior or posterolateral. O’Driscoll et al demonstrated simple elbow dislocations can be produced by sequential ligament failure from the lateral to the medial side, a concept termed “Horii circle”(9). Schreiber reviewing 62 youtube.com video footage of elbow dislocation concluded that the elbow dislocates in a position of relative extension (10). He stated that the sequence of disruption occurs from medial to lateral, disrupting the anterior bundle of the medial collateral ligament (aMCL) first. Evidence of MRI from further studies by Schreiber et al and Rhyou et al confirms this concept, the first study showing significant partial or complete medial ligament tears in all MRI scans following simple dislocations(11, 12). Other mechanisms can result in different sequences of osseous and soft tissue injury leading to elbow dislocation.
Definition and classifications
Dislocation of the elbow is defined as static loss of ulnohumeral and radiocapitellar joint congruency whereas instability is defined as dynamic disturbance to joint congruency with stress (13). Elbow dislocations are primarily classified as simple, or complex based on the presence of concomitant fractures. Simple elbow dislocations are by definition not associated with fractures; however small osteochondral fractures may still be present in a dislocation classified as simple based on initial radiographs. The commonly associated fractures include the radial head and the neck, the olecranon and the proximal ulna, the coronoid process, the capitulum, and the distal humerus. Approximately 17% of the elbow dislocations are associated with fractures (4). When elbow dislocations are compounded by radial head fractures and ulnar coronoid fractures, it is classified under “Terrible Triad Injury” which lead to poor outcomes if not treated properly (14). Elbow dislocations can occur as open or compound injuries where the dislocation or the fractures are communicating with the exterior. Although rare, the median nerve, the radial nerve, the ulnar nerve, and the brachial artery are at risk of injury during elbow dislocation (15). Therefore, neurovascular examination remains an important part of assessment following elbow dislocation. Elbow dissociations are also classified by the direction of the dislocation, with posterior and posterolateral dislocation accounting for 90% (16).
image
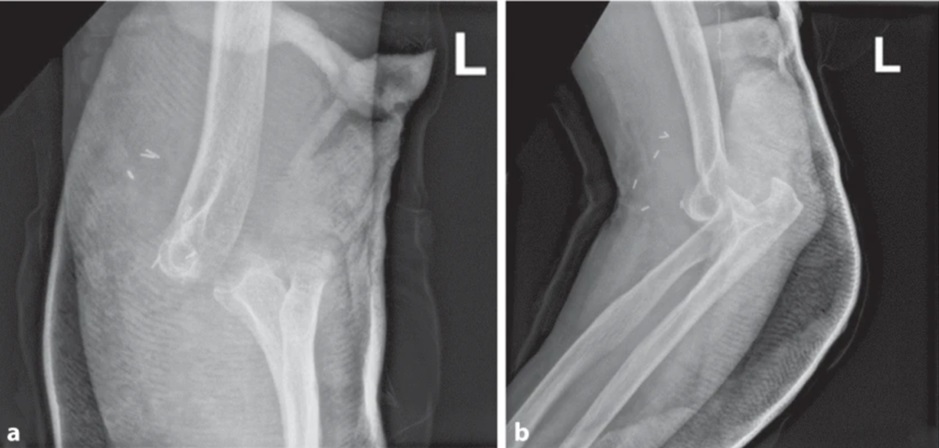
Figure 2 Complex elbow dislocation from Surgical management of a traumatic elbow dislocation with disruption of the brachial artery by Habarta, J., Jordan, M., Meffert, R. et al. Obere Extremität 17, 267–271 (2022). [used under Creative Commons CC-BY license].
Assessment
The importance of history, physical examination, and directed imaging to diagnose elbow dislocation cannot be overstated. The normal range of elbow flexion-extension prono-supination and varus and valgus stability can help rule out a dislocated elbow clinically. Palpation of anatomical landmarks in relation to each other also provides convincing evidence of an enlocated elbow. Plain anteroposterior and lateral radiographs are the mainstay in diagnosing a dislocated elbow.
The upper extremity is placed adjacent to the radiographic table with the entire posterior surface of the extremity contacting the cassette for the standard anteroposterior elbow radiograph. The beam is directed from anterior to posterior, perpendicular to the elbow. The hand is supinated, and the elbow is extended. Using the anteroposterior view the radiographic anatomy of the medial and lateral condyles, the radiocapitellar joint, the trochlea, the olecranon, the radial tuberosity, and the anteromedial facet of the coronoid can be delineated. The normal carrying angle of 5° to 20° valgus angle can also be appreciated.
The lateral view is obtained by flexing the elbow to 90° and placing it on the cassette. The entire upper extremity is maintained parallel to the floor and the forearm is maintained in the neutral position with the thumb pointed towards the ceiling. The X-ray beam is directed perpendicular to the elbow. Three concentric rings can be identified in a lateral radiograph of the elbow. From outside to inside, they represent the medial trochlear ridge, the capitellum, and the trochlear groove. Disruption of this concentric anatomy may indicate a pathology. Also, the anterior humeral line should intersect the capitellum in its middle third. If the radiocapitellar line that passes through the radial neck does not intersect the capitellum, the radial head dislocation or subluxation should be suspected.
In addition, the dislocation is associated with fractures and complex patterns the radiographs provide the initial assessment of the complex fracture patterns. In situations where the elbow is dislocated and relocated in the field, standard static X-ray imaging gives minimal details on instability which is a dynamic phenomenon. Standard anteroposterior and lateral X-rays may still reveal the presence of loose bodies, arthritis, coronoid dysplasia, and malalignments that occurred because of a paediatric fracture. Also following an acute dislocation, this may reveal, angulations in the radial neck, rim defects in the radial head, and impaction fractures of the capitellum.
Once the elbow is reduced assessment for physical signs of instability is important and is based on indirectly eliciting instability with stress testing. Thus, all involve axial loading with varus, valgus, or rotatory forces acting upon the elbow to demonstrate instability. This recreates the forces that disturb joint congruity, thereby indirectly observing features of instability like subluxation of the radial head, apprehension, and a palpable clunk. Eliciting subtle forms of instability clinically can be challenging, and findings can be equivocal in milder forms, in which ligament reconstruction is helpful.
While radiographs are helpful in most simple elbow dislocations, computed tomography (CT) is an important investigation to identify whether there are any fractures leading to long-term instability. Coronoid fractures are one such example. In complex dislocations, 3D CT scans are immensely helpful in assessing the fracture morphology in coronoid fractures, radial head fractures, and associated bone loss of the capitellum as in a ‘Hill-Sach’s lesion (17).
MRI Can help assess the extent of chondral injuries, ligament tears, chondral injuries, and joint subluxations. However, MRI is not a routine investigation in the acute setting. Dynamic imaging like ultra-sonography and fluoroscopy can demonstrate radial head subluxation or ulno-humeral widening. Ulno-humeral laxity of more than 4 mm is indicative of posterolateral rotatory instability (PLRI). Examination for the integrity of the nerves, specifically the ulnar nerve is mandatory. Associated injury to the forearm interosseous membrane can lead to longitudinal instability patterns such as Essex-Lopressti injury. The distal radioulnar joint must also be examined to identify any possibility of longitudinal instability (18).
Principles of management
Simple acute elbow dislocation rarely needs surgery, except for irreducible dislocations and the inability to maintain reduction. These occur in less than 10% of cases of acute simple elbow dislocations. Over 90% of the simple dislocations are managed with reduction and splinting. Pronation increases the stability of the elbow if lateral instability is the aetiology (19). In isolated medial instability, the patient should be splinted in supination (20). However, if both lateral and medial ligament complexes are compromised immobilization in the neutral position is recommended. At least for 4 weeks, unprotected shoulder abduction is not recommended. This is to prevent varus strain on the healing lateral ligament complex.
Some authors recommend examination under anaesthesia for simple dislocations if the mechanism of injury is of high energy, severe swelling and bruising all around the elbow, and if the patients are reluctant for active mobilization after 1-2 weeks of non-operative management (17). This is due to the extent of soft tissue injury being more dramatic where the whole distal humerus can be stripped off the soft tissue. Ligament repair is recommended in the acute stage for unstable elbows <30°. The repair can also be attempted for early, less symptomatic chronic PLRI if soft tissues are favourable. For open surgery, the patient is positioned supine with the affected arm on a hand table. The use of a sterile tourniquet is helpful for adequate access during the procedure. The Kocher approach is used for isolated lateral access, but a posterior incision is an option in the presence of co-existing medial instability. In acute elbow dislocations, it is common to find a hematoma with a torn anterior capsule and brachialis muscle. Once the hematoma is cleared laxity of the lateral ligament complex and annular ligament can be observed. It is not uncommon to find the entire lateral ligament complex avulsed from the humeral origin and flipped into the radio-capitellar joint.
Once the avulsed proximal end is freed up, the footprint on the posterior aspect of the lateral humeral epicondyle can be identified. This is seen as a bare area directly lateral and slightly inferior to the centre of the olecranon fossa. After debriding the footprint, a trans osseous repair can be done with No 1 or 2 non-absorbable braided sutures. Sutures are tied at elbow flexion of 30°. Suture anchor repair is another option. A cast or brace is applied for the initial post-operative period which can be replaced by a removal splint/ brace at 10-14 days. The elbow is splinted at rest for 4 weeks, strictly avoiding shoulder abduction.
Complex elbow dislocations involving fractures are managed with anatomical reduction of the fracture fragments and stable fixation. The associated lateral collateral and medial collateral ligaments should be repaired either using suture anchors or trans-osseous sutures.
Outcome
The outcome following simple dislocations is generally satisfactory with only 10% reporting ongoing instability. Approximately 50% of the patients gain full range of motion, absent pain with good functional outcome. One-third of patients have less than 15 ° of loss of the range of motion, minimal pain, and good stability. With complex dislocations, associated fractures of the ulna, radial head and coronoid are the predictors of poor prognosis if not treated appropriately.
Conflicting interests: The author(s) declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Artificial intelligence: Generative artificial intelligence or artificial intelligence assisted technologies were not used in preparing this manuscript.
References
- Kuhn MA, Ross G. Acute elbow dislocations. Orthop Clin North Am. 2008;39(2):155-61, v.https://doi.org/10.1016/j.ocl.2007.12.004
- Stoneback JW, Owens BD, Sykes J, Athwal GS, Pointer L, Wolf JM. Incidence of elbow dislocations in the United States population. JBJS. 2012;94(3):240-5.https://doi.org/10.2106/jbjs.j.01663
- Mehlhoff TL, Noble PC, Bennett JB, Tullos HS. Simple dislocation of the elbow in the adult. Results after closed treatment. J Bone Joint Surg Am. 1988;70(2):244-9.https://pubmed.ncbi.nlm.nih.gov/3343270/
- Yang NP, Chen HC, Phan DV, Yu IL, Lee YH, Chan CL, et al. Epidemiological survey of orthopedic joint dislocations based on nationwide insurance data in Taiwan, 2000-2005. BMC Musculoskelet Disord. 2011;12:253.https://doi.org/10.1186/1471-2474-12-253
- Panteli M, Pountos I, Kanakaris NK, Tosounidis TH, Giannoudis PV. Cost analysis and outcomes of simple elbow dislocations. World J Orthop. 2015;6(7):513-20.https://doi.org/10.5312/wjo.v6.i7.513
- Alcid JG, Ahmad CS, Lee TQ. Elbow anatomy and structural biomechanics. Clin Sports Med. 2004;23(4):503-17, vii.https://doi.org/10.1016/j.csm.2004.06.008
- Cain Jr EL, Dugas JR, Wolf RS, Andrews JR. Elbow injuries in throwing athletes: a current concepts review. The American journal of sports medicine. 2003;31(4):621-35.https://doi.org/10.1177/03635465030310042601
- Acosta Batlle J, Cerezal L, López Parra MD, Alba B, Resano S, Blázquez Sánchez J. The elbow: review of anatomy and common collateral ligament complex pathology using MRI. Insights into Imaging. 2019;10(1):43.https://doi.org/10.1186/s13244-019-0725-7
- O’Driscoll SW, Morrey BF, Korinek S, An K-N. Elbow subluxation and dislocation. A spectrum of instability. Clinical orthopaedics and related research. 1992(280):186-97.https://pubmed.ncbi.nlm.nih.gov/1611741/
- Schreiber JJ, Warren RF, Hotchkiss RN, Daluiski A. An online video investigation into the mechanism of elbow dislocation. The Journal of hand surgery. 2013;38(3):488-94.https://doi.org/10.1016/j.jhsa.2012.12.017
- Schreiber JJ, Potter HG, Warren RF, Hotchkiss RN, Daluiski A. Magnetic resonance imaging findings in acute elbow dislocation: insight into mechanism. The Journal of hand surgery. 2014;39(2):199-205.https://doi.org/10.1016/j.jhsa.2013.11.031
- Rhyou IH, Kim YS. New mechanism of the posterior elbow dislocation. Knee Surgery, Sports Traumatology, Arthroscopy. 2012;20(12):2535-41.https://doi.org/10.1007/s00167-011-1872-7
- Marinelli A, Guerra E, Rotini R. Elbow instability: are we able to classify it? Review of the literature and proposal of an all-inclusive classification system. Musculoskeletal surgery. 2016;100(1):61-71.https://doi.org/10.1007/s12306-016-0424-1
- Rodriguez-Martin J, Pretell-Mazzini J, Andres-Esteban EM, Larrainzar-Garijo R. Outcomes after terrible triads of the elbow treated with the current surgical protocols. A review. Int Orthop. 2011;35(6):851-60.https://doi.org/10.1007/s00264-010-1024-6
- Carter SJ, Germann CA, Dacus AA, Sweeney TW, Perron AD. Orthopedic pitfalls in the ED: neurovascular injury associated with posterior elbow dislocations. The American Journal of Emergency Medicine. 2010;28(8):960-5.https://doi.org/10.1016/j.ajem.2009.05.024
- Taylor F, Sims M, Theis JC, Herbison GP. Interventions for treating acute elbow dislocations in adults. Cochrane Database Syst Rev. 2012;2012(4):Cd007908.https://doi.org/10.1002/14651858.cd007908.pub2
- Phadnis J, Bain GI. Posterolateral Rotatory Instability of the Elbow. Sports Injuries of the Elbow: Springer; 2021. p. 51-62.https://doi.org/10.5435/00124635-200411000-00005
- Gong M, Wang H, Jiang X, Liu Y, Zhou J. Traumatic divergent dislocation of the elbow in the adults. International Orthopaedics. 2023;47(3):847-59.https://doi.org/10.1007%2Fs00264-022-05679-5
- Dunning CE, Zarzour ZD, Patterson SD, Johnson JA, King GJ. Muscle forces and pronation stabilize the lateral ligament deficient elbow. Clinical Orthopaedics and Related Research (1976-2007). 2001;388:118-24.https://doi.org/10.1097/00003086-200107000-00018
- Armstrong AD, Dunning CE, Faber KJ, Duck TR, Johnson JA, King GJ. Rehabilitation of the medial collateral ligament-deficient elbow: an in vitro biomechanical study. The Journal of hand surgery. 2000;25(6):1051-7.https://doi.org/10.1053/jhsu.2000.17819