Abstract
Context:
Head trauma (HT) is one of the most important types of traumata that has a high prevalence and may occur in different age groups, ranging from infants to the elderly.Objectives:
Considering the importance of the prevalence of all types of traumata, especially HT, this study was conducted to measure the prevalence of HT in Iran by systematic review and meta-analysis.Methods:
The present systematic review and meta-analysis was conducted according to the PARISMA checklist to assess the prevalence of HT in Iran. PICO approach was carried out with the inclusion criteria of the articles as follows, and the search was conducted by two researchers completely independently from October 1 to November 30, 2022. Analysis was done by CMA v.2.0 software and using a random model, funnel plot, and meta-regression analysis.Results:
In the 22 reviewed articles, the time of publication of the articles was between 2008 and 2022, and the total sample size was equal to 99,306. Also, in relation to the method of conducting studies, two studies were conducted using a retrospective method, two articles were conducted using a prospective method, and other articles were conducted using a cross-sectional method. The results showed the overall HT prevalence was 26.2 (95% CI, 14.4 - 29.2) in Iran. Moreover, there was no relationship between the year of publication of articles (P = 0.96, Z-value = 0.05) and sample size (P = 0.41, Z-value = -0.82) with the prevalence of HT.Conclusions:
Considering the high prevalence of HT in Iran, it is necessary to carry out necessary preventive interventions in this field.Keywords
Head Trauma Traumatic Brain Injury Meta-analysis Iran Prevalence
1. Context
Trauma is considered one of the important global challenges. It has become an important problem with the advancement of science and technology. It has now become one of the common causes of death and disability (1-3). Trauma is one of the most important causes of the absence of young forces in economic and social activities. In addition to reducing the abilities of the young population and active forces in society, it causes economic society challenges by involving health and rehabilitation caregivers (4-6).
Trauma can be divided in terms of its type and causes. Trauma can be divided into various types, including vascular trauma, dental trauma, facial trauma, penetrating and non-penetrating trauma, as well as head trauma (7-9). The causes of trauma can also include falls, violence and fights, vehicle accidents, and sports events. Head trauma (HT) is one of the most important types of trauma that has a high prevalence and may occur in different age groups, ranging from infants to the elderly (10-12).
Accidents alone are the second leading cause of years of life lost worldwide. There have been various systematic review studies or meta-analysis studies on the prevalence of trauma in Iran. In this regard, in a meta-analysis of nine articles, Shokri et al. (13) reported the overall prevalence of neonatal birth trauma in 42,327 Iranian infants was equal to 2.7% (95% CI (1.3, 5.3)). Shokri et al. (14) also stated that the prevalence of dental trauma among Iranian children was between 8.9% - 36.9%. In a review study, Maleki et al. also mentioned that the causes of trauma among Iranian children included falls, sports accidents, burns, and drowning (15). Considering the high prevalence of trauma in the world as well as in Iran, it is important to conduct extensive studies on the prevalence of trauma, especially HT (16).
Head trauma negatively affects most aspects of life and can cause physical, cognitive, and social limitations in the patient, all of which affect the well-being of patients (17, 18). Head trauma is one of the most important causes of death, and its frequency in developed countries is estimated at 266 per 1,000 people. Depending on the trauma site, the patient may experience a wide range of mild to moderate injuries, resulting in various complications, including disability, amputation, or even death (19, 20). Also, considering that HT is one of the important risk factors for nerve damage, HT can expose the patient to Parkinson's, Alzheimer's, or other neurological disorders and cause serious long-term damage (21).
2. Objectives
Considering the importance of the prevalence of all types of traumata, especially HT, this study was conducted to measure the prevalence of HT in Iran by systematic review and meta-analysis.
3. Methods
The present systematic review and meta-analysis was conducted according to the PARISMA checklist (22) to assess the prevalence of HT in Iran.
3.1. Database search strategy
3.1.1. Selection of Studies
In this study, the PICO approach was carried out with the selection criteria of the articles as follows: P: Patients with trauma in Iran; I: Prevalence of HT; C: Comparison of HT with other trauma; and O: Frequency (%) HT in total trauma in articles.
3.1.2. Paper Selection and Data Extraction
The search was conducted by two researchers completely independently from October 1 to November 30, 2022. The search was conducted among the articles published in the years 2007 to 2022 in national databases (SID, Magiran, and Irandoc) and international databases (Web of Science, PubMed, and Scopus). Also, the search was conducted using the keywords of “head trauma”, “traumatic brain injury”, “Iran”, “trauma”, and “prevalence”.
3.1.3. Inclusion and Exclusion Criteria
Inclusion criteria: Articles published (Persian and English) between 2002 - 2022 in which the prevalence of HT a (number and percentage) was reported. Exclusion criteria: Articles with incomplete data.
3.2. Data Extraction
Questions related to the number of patients (men, women, and overall), average age, city, and overall prevalence of HT were used.
3.3. Statistical Analysis
Analysis was done by CMA v.2.0 software and using a random model, funnel plot, and meta-regression analysis.
4. Results and Discussion
Table 1 shows the quality status of the articles. If any articles scored less than 3, they were considered weak in the group and excluded from the study. Also, in the case of obtaining a score of 4 to 6, it was considered to mean average quality and a score of 6 and above was considered to mean high quality. In the initial search, 183 articles were found, 90 articles were removed in the initial review, and finally, 22 articles were included in the meta-analysis stage. In the 22 reviewed articles, the time of publication of the articles was between 2008 and 2022, and the total sample size was equal to 99,306. Also, in relation to the method of conducting studies, two studies were conducted using a retrospective method, two articles were conducted using a prospective method, and other articles were conducted using a cross-sectional method (Table 2). Moreover, the sample size ranged from 264 patients in the study by Yadollahi and Sahmeddini (23) to 47,295 patients in the study by Bolandparvaz et al. (24). The HT prevalence also ranged from 0.3% in the study by Rahimi-Movaghar et al. (25) to 77.2% in the study by Yousefzadeh et al. (26) (Table 2). Also, Figure 1 shows flowcharts for systematic review (Figure 1).
The Quality of the Articles
| - | Authors | Years | Sample Size | Mean Age | Male (n) | Female (n) | Type of Study | Prevalence | Total Score |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Aghakhani et al. (27) | √ | √ | √ | - | - | √ | √ | 5 |
| 2 | Rahimi-Movaghar et al. (25) | √ | √ | √ | √ | √ | √ | √ | 7 |
| 3 | Fakharian et al. (28) | √ | √ | √ | √ | √ | √ | √ | 7 |
| 4 | Reihanian et al. (29) | √ | √ | √ | √ | √ | √ | √ | 7 |
| 5 | Alavi et al. (30) | √ | √ | √ | √ | √ | √ | √ | 7 |
| 6 | Yousef Zade Chabok et al. (31) | √ | √ | √ | √ | √ | √ | √ | 7 |
| 7 | Saeednejad et al. (32) | √ | √ | - | - | - | √ | √ | 4 |
| 8 | Soltani et al. (33) | √ | √ | √ | √ | √ | √ | √ | 7 |
| 9 | Hatamabadi et al. (34) | √ | √ | - | - | -- | √ | √ | |
| 10 | Bolandparvaz et al. (24) | √ | √ | √ | √ | √ | √ | √ | 7 |
| 11 | Ghaffari-Fam et al. (35) | √ | √ | - | - | - | √ | √ | 4 |
| 12 | Yousefzadeh et al. (26) | √ | √ | √ | - | - | √ | √ | 5 |
| 13 | Yadollahi and Sahmeddini (23) | √ | √ | - | - | - | √ | √ | 4 |
| 14 | Montazer et al. (36) | √ | √ | - | - | - | √ | √ | |
| 15 | Zandi and Seyed Hoseini (37) | √ | √ | √ | √ | √ | √ | √ | 7 |
| 16 | Zandi et al. (38) | √ | √ | - | - | - | √ | √ | 4 |
| 17 | Jalalvandi et al. (39) | √ | √ | - | √ | √ | √ | √ | 6 |
| 18 | Hatamabadi et al. (40) | √ | √ | - | - | - | √ | √ | 4 |
| 19 | Ghaem et al. (41) | √ | √ | - | - | - | √ | √ | 4 |
| 20 | Abbasi et al. (42) | √ | √ | - | - | - | √ | √ | 4 |
| 21 | Sehat et al. (43) | √ | √ | - | - | - | √ | √ | 4 |
| 22 | Karbakhsh et al. (44) | √ | √ | - | - | - | √ | √ | 4 |
| - | Authors | Years | Gender | Age, y | City | Type of Study | Sample Size | Prevalence (N) | |
|---|---|---|---|---|---|---|---|---|---|
| Male | Female | ||||||||
| 1 | Aghakhani et al. (27) | 2013 | - | - | 31.9 | Urmia | Retrospective | 1,796 | 721 |
| 2 | Rahimi-Movaghar et al. (25) | 2011 | 17 (81) | 4 (19) | 28.7 ± 14.8 | Tehran | Retrospective | 7,110 | 21 |
| 3 | Fakharian et al. (28) | 2016 | 38 (97.2) | 3 (7.3) | 36.6 ± 20.6 | Kashan | Cross-sectional | 1,629 | 41 |
| 4 | Reihanian et al. (29) | 2022 | 116 (69.8) | 50 (30.2) | 0 - 15 | Northern Iran | Cross-sectional | 543 | 166 |
| 5 | Alavi et al. (30) | 2013 | 44 (81.48) | 10 (19.52) | Male: 24.8, Femail: 27.4 | Bandar-Abbas | Cross-sectional | 1,971 | 54 |
| 6 | Yousef Zade Chabok et al. (31) | 2008 | 2,582 (76.7) | 781 (23.3) | 31.35 ± 18.16 | Rasht | Cross-sectional | 3,368 | 2,156 |
| 7 | Saeednejad et al. (32) | 2021 | - | - | - | Tehran | Cross-sectional | 1,817 | 62 |
| 8 | Soltani et al. (33) | 2016 | 58 (75) | 19 (25) | 32 | Tehran | Routine-data-based study | 307 | 77 |
| 9 | Hatamabadi et al. (34) | 2017 | - | -- | - | Tehran | Cross-sectional | 460 | 198 |
| 10 | Bolandparvaz et al. (24) | 2017 | 5,933 (34.7) | 1,493 (30.9) | 30 (23 - 44) | Shiraz | Cross-sectional | 47,295 | 7,426 |
| 11 | Ghaffari-Fam et al. (35) | 2015 | - | - | - | Azerbaijan | Cross-sectional | 3,397 | 2,268 |
| 12 | Yousefzadeh et al. (26) | 2008 | - | - | 0 - 14 | Guilan | Cross-sectional | 347 | 272 |
| 13 | Yadollahi and Sahmeddini (23) | 2021 | - | - | - | Shiraz | Cross-sectional | 246 | 215 |
| 14 | Montazer et al. (36) | 2019 | - | - | - | Mazandaran | Cross-sectional | 13,965 | 5,216 |
| 15 | Zandi and Seyed Hoseini (37) | 2013 | 268 (88.7) | 34 (11.3) | 41.8 ± 21.4 | Hamedan | Case-control | 2,692 | 302 |
| 16 | Zandi et al. (38) | 2011 | - | - | - | Hamedan | Prospective study | 2,450 | 65 |
| 17 | Jalalvandi et al. (39) | 2016 | 52 (29.1) | 43 (34.4) | - | Kermanshah | Cross-sectional | 304 | 95 |
| 18 | Hatamabadi et al. (40) | 2012 | - | - | - | Tehran | Cohort | 394 | 84 |
| 19 | Ghaem et al. (41) | 2017 | - | - | - | Shiraz | Cross-sectional | 5,840 | 842 |
| 20 | Abbasi et al. (42) | 2013 | - | - | - | Shiraz | Cross-sectional | 2,322 | 1,057 |
| 21 | Sehat et al. (43) | 2021 | - | - | - | Kashan | Cross-sectional | 274 | 29 |
| 22 | Karbakhsh et al. (44) | 2009 | - | - | - | Kermanshah | Cross-sectional | 779 | 215 |
Flowcharts for systematic review
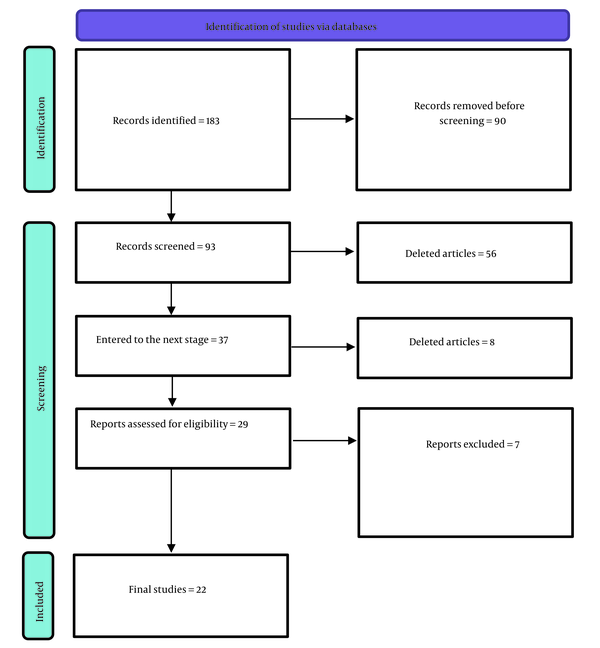
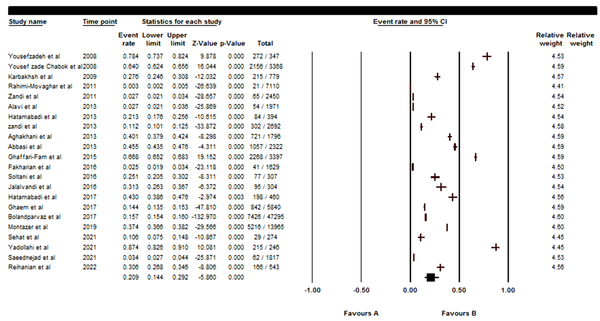
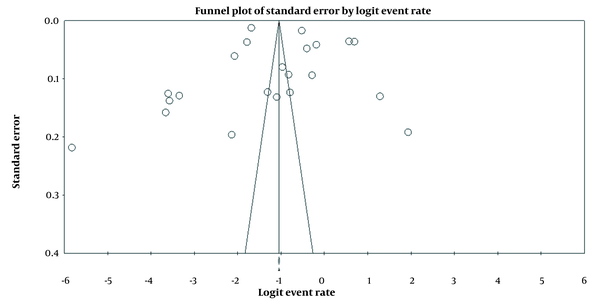
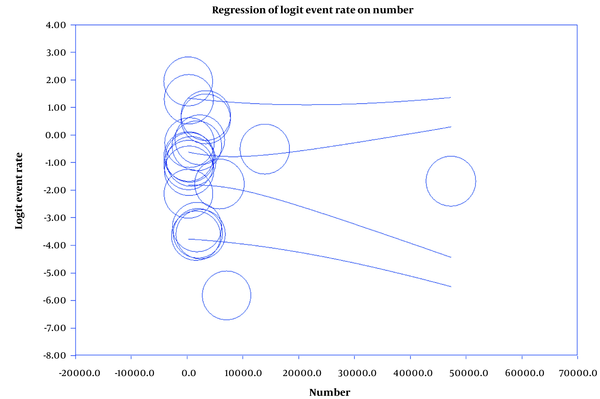
Figure 2 shows that the overall HT prevalence was 20.9 (95% CI, 14.4 - 29.2) in Iran. Also, Figure 3 shows the funnel plot diagram, and Figures 4 and 5 show the meta-regression of the prevalence of HT based on the year and number of patients of publication of the articles. Also, there was no relationship between the year of publication of articles (P = 0.96, Z-value = 0.05) and sample size (P = 0.41, Z-value = -0.82) with the prevalence of HT.
The prevalence of head trauma in Iran
Funnel plot for studies included in the meta-analysis
Meta-regression, according to the time of article publication
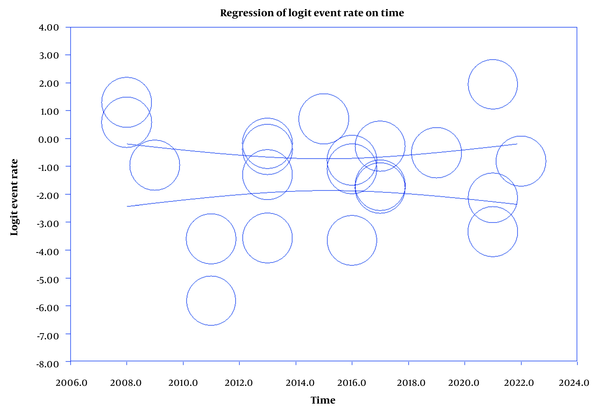
Meta-regression, according to the years of article publication
Diseases related to the head and nervous system can seriously threaten the patient’s life (45-47). Trauma has many types, and its prevalence is high (48, 49). According to the results, the overall prevalence of HT in Iran is 20.9 (95% CI, 14.4 - 29.2). Various studies have been conducted on traumatic brain injury (TBI) prevalence in different age groups. For example, in a study on 42,412 children and adolescents, Nigrovic et al. reported that the TBI prevalence was 42,099 (99%) (16). Aoki et al. also stated that out of 15,441 trauma children in Japan, 6,386 (41.35%) patients had HT (50). Langlois et al. also reported that the TBI prevalence in children aged 0 - 14 years was reported to be about 475,000 (51), which is much more than the results of the present study.
This discrepancy seems to be due to the study population. Further, the TBI prevalence in Thurman's study was 74 per 100,000 people in the emergency department (52). Haarbauer-Krupa et al. also reported that the TBI prevalence was 2.5% (95% CI, 2.3% - 2.7%) during the years 2011 - 2012 (53), which was lower than the results of the present study. This discrepancy may be due to differences in age groups and also the type of study. The current study is a meta-analysis study that was carried out on all age groups, while the aforementioned studies were original and were performed on children.
The TBI prevalence has also been investigated among the adult population in other countries. For example, Gerritsen et al. found that the HT prevalence was equal to 22.1 per 1,000 patients (54), Baiden et al. also concluded that out of 6,314 patients, the TBI prevalence was equal to 208 cases (3.3%) (55), which is much lower than the present study. This discrepancy may be due to the fact that the current study was a meta-analysis, while the above-mentioned studies were original.
5. Conclusions
Considering the high prevalence of HT in Iran, it is necessary to carry out necessary preventive interventions in this field.
References
-
1.
Retel Helmrich IRA, van Klaveren D, Andelic N, Lingsma H, Maas A, Menon D, et al. Discrepancy between disability and reported well-being after traumatic brain injury. J Neurol Neurosurg Psychiatry. 2022;93(7):785-96. [PubMed ID: 35537823]. [PubMed Central ID: PMC9279746]. https://doi.org/10.1136/jnnp-2021-326615.
-
2.
Yadollahi M, Jamali K, Pazhuheian F, Nezam Eftekhari MA. Survival Following Road Traffic Accidents in a Level-I Trauma Center, Parametric versus Semi-Parametric Survival Models. Iran Red Crescent Med J. 2021;23(5):e297. https://doi.org/10.32592/ircmj.2021.23.5.297.
-
3.
Yang R, Lan S, Wu Q, Ye F, Ye J, Huang S, et al. Intrathoracic fracture-dislocation of the humeral head: A case report and review of the literature. Iran Red Crescent Med J. 2021;23(8):e1248. https://doi.org/10.32592/ircmj.2021.23.8.1248.
-
4.
Godoy DA, Seifi A, Chi G, Paredes Saravia L, Rabinstein AA. Intracranial Pressure Monitoring in Moderate Traumatic Brain Injury: A Systematic Review and Meta-Analysis. Neurocrit Care. 2022;37(2):514-22. [PubMed ID: 35610529]. https://doi.org/10.1007/s12028-022-01533-z.
-
5.
Felder JM, Ducic I. Cross-Sectional Evaluation of the Economic Burden on Patients Seeking Surgical Treatment for Chronic Nerve Injuries. Ann Plast Surg. 2022;88(2):200-7. [PubMed ID: 34176908]. https://doi.org/10.1097/SAP.0000000000002924.
-
6.
Sahu ES, Sachdeva M, Sen A, Karkhur S. Multimodal Imaging in Retinal Vascular Occlusions following Trauma - A Case of Sickle Cell Disease with Negative Sickling Test. J Ophthalmic Vis Res. 2021;16(3):502-6. [PubMed ID: 34394877]. [PubMed Central ID: PMC8358746]. https://doi.org/10.18502/jovr.v16i3.9444.
-
7.
Dar AA, Deb S. Prevalence of trauma among young adults exposed to stressful events of armed conflicts in South Asia: Experiences from Kashmir. Psychol Trauma. 2022;14(4):633-41. [PubMed ID: 34323569]. https://doi.org/10.1037/tra0001045.
-
8.
Narayanan SP, Rath H, Panda A, Mahapatra S, Kader RH. Prevalence, Trends, and Associated Risk Factors of Traumatic Dental Injury among Children and Adolescents in India: A Systematic Review and Meta-analysis. J Contemp Dent Pract. 2021;22(10):1206-24. [PubMed ID: 35197391].
-
9.
Dahal S, Karmacharya RM, Singh AK, Vaidya S, Dhakal P, Thapa P, et al. Peripheral Vascular Trauma among Vascular Surgery Cases Operated in a Tertiary Care Hospital: A Descriptive Cross-sectional Study. JNMA J Nepal Med Assoc. 2022;60(245):12-6. [PubMed ID: 35199678]. [PubMed Central ID: PMC9157658]. https://doi.org/10.31729/jnma.6764.
-
10.
Kanala S, Gudipalli S, Perumalla P, Jagalanki K, Polamarasetty PV, Guntaka S, et al. Aetiology, prevalence, fracture site and management of maxillofacial trauma. Ann R Coll Surg Engl. 2021;103(1):18-22. [PubMed ID: 32808805]. [PubMed Central ID: PMC7705151]. https://doi.org/10.1308/rcsann.2020.0171.
-
11.
Pillay L, Mabongo M, Buch B. Prevalence and aetiological factors of maxillofacial trauma in a rural district hospital in the Eastern Cape. S Afr Dent J. 2018;73(5):348-53. https://doi.org/10.17159/2519-0105/2018/v73no5a4.
-
12.
Olczak-Kowalczyk D, Turska-Szybka A, Studnicki M, Tomczyk J. Prevalence, Etiology, and Types of Dental Trauma in Self-Assessment of 18-Year-Olds in Poland. Int J Environ Res Public Health. 2022;19(19):12924. [PubMed ID: 36232226]. [PubMed Central ID: PMC9566764]. https://doi.org/10.3390/ijerph191912924.
-
13.
Shokri M, Nayyeri S, Salimi N, Nourmohammadi A, Tarjoman A, Borji M, et al. Prevalence of Neonatal Birth Trauma in Iran: a Systematic Review and Meta-analysis. Int J Pediatr. 2021;9(10):14520-31. https://doi.org/10.22038/ijp.2020.50652.4032.
-
14.
Shokri M, Afsharloo S, Tarjoman A, Borji M, Mahdikhani S, Maleki M, et al. Dental Trauma among Iranian Children and Adolescents: A Comprehensive Study. Int J Pediatr. 2021;9(1):12901-8. https://doi.org/10.22038/ijp.2020.49893.3980.
-
15.
Maleki MM, Afsharloo S, Tarjoman A, Borji M, Mahdikhani S, Shokri M. Prevalence of Trauma and Related Factors in Iranian Children and Adolescents: Systematic Review. Int J Pediatr. 2021;9(9):14293-306. https://doi.org/10.22038/ijp.2020.49720.3975.
-
16.
Nigrovic LE, Lee LK, Hoyle J, Stanley RM, Gorelick MH, Miskin M, et al. Prevalence of clinically important traumatic brain injuries in children with minor blunt head trauma and isolated severe injury mechanisms. Arch Pediatr Adolesc Med. 2012;166(4):356-61. [PubMed ID: 22147762]. https://doi.org/10.1001/archpediatrics.2011.1156.
-
17.
Maas AIR, Menon DK, Adelson PD, Andelic N, Bell MJ, Belli A, et al. Traumatic brain injury: integrated approaches to improve prevention, clinical care, and research. Lancet Neurol. 2017;16(12):987-1048. [PubMed ID: 29122524]. https://doi.org/10.1016/S1474-4422(17)30371-X.
-
18.
Karacabey S, Sanrı E. Optic Nerve Sheath Diameter Affected by Cervical Collar Placement in Minor Head Trauma Patients. Iran Red Crescent Med J. 2022;24(10). e1530. https://doi.org/10.32592/ircmj.2022.24.10.1530.
-
19.
Bresnahan BW. Economic evaluation in radiology: reviewing the literature and examples in oncology. Acad Radiol. 2010;17(9):1090-5. [PubMed ID: 20634104]. https://doi.org/10.1016/j.acra.2010.05.020.
-
20.
Shahhosseini R, Ebrahimi Nejad A, Shahba M, Tajoddini S, Ghaedamini H, Farahbakhsh S, et al. [Investigation of the changes in CT scan findings in patients with head trauma referred to the emergency department of Shahid Bahonar Hospital in Kerman in 2020]. Qom Univ Med Sci J. 2021;15(2):130-9. Persian. https://doi.org/10.52547/qums.15.2.130.
-
21.
Behnke JA, Ye C, Setty A, Moberg KH, Zheng JQ. Repetitive mild head trauma induces activity mediated lifelong brain deficits in a novel Drosophila model. Sci Rep. 2021;11(1):9738. [PubMed ID: 33958652]. [PubMed Central ID: PMC8102574]. https://doi.org/10.1038/s41598-021-89121-7.
-
22.
Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169(7):467-73. [PubMed ID: 30178033]. https://doi.org/10.7326/M18-0850.
-
23.
Yadollahi M, Sahmeddini S. An overview of the prevalence and pattern of maxillofacial trauma in the south of Iran. J Emerg Pract Trauma. 2021;7(2):118-22. https://doi.org/10.34172/jept.2021.13.
-
24.
Bolandparvaz S, Yadollahi M, Abbasi HR, Anvar M. Injury patterns among various age and gender groups of trauma patients in southern Iran: A cross-sectional study. Medicine (Baltimore). 2017;96(41):e7812. [PubMed ID: 29019874]. [PubMed Central ID: PMC5662297]. https://doi.org/10.1097/MD.0000000000007812.
-
25.
Rahimi-Movaghar V, Saadat S, Rasouli MR, Ghahramani M, Eghbali A. The Incidence of Traumatic Brain Injury in Tehran, Iran: A Population Based Study. The American Surgeon. 2011;77(6):112-4. https://doi.org/10.1177/000313481107700608.
-
26.
Yousefzadeh S, Hemmati H, Alizadeh A, Karimi A, Masoumeh Ahmadi M, Mohammadi H. Pediatric Unintentional Injuries in North of Iran. Iran J Pediatr. 2008;18(3):267-71.
-
27.
Aghakhani N, Azami M, Jasemi M, Khoshsima M, Eghtedar S, Rahbar N. Epidemiology of traumatic brain injury in urmia, iran. Iran Red Crescent Med J. 2013;15(2):173-4. [PubMed ID: 23682332]. [PubMed Central ID: PMC3652507]. https://doi.org/10.5812/ircmj.2090.
-
28.
Fakharian E, Mohammadzadeh M, Behdadmehr S, Sabri HR, Mirzadeh AS, Mohammadzadeh J. Repetitive Traumatic Brain Injury in Patients From Kashan, Iran. Trauma Mon. 2016;21(4):e23869. [PubMed ID: 28180123]. [PubMed Central ID: PMC5282941]. https://doi.org/10.5812/traumamon.23869.
-
29.
Reihanian Z, Noori Roodsari N, Rimaz S, Asadi P, Khoshsima N, Rafiee Zadeh A, et al. Traumatic brain injuries in children during COVID-19 pandemic: a national report from northern Iran. Int J Burns Trauma. 2022;12(4):175-9. [PubMed ID: 36160672]. [PubMed Central ID: PMC9490154].
-
30.
Alavi SA, Taghaviasl M, Baghr Zadeh Homaii N. Prevalence of head trauma causes in Bandar Abbas-Iran. Life Sci J. 2013;10(12s):284-7.
-
31.
Yousef Zade Chabok S, Safayi M, Hemati H, Mohammadi H, Ahmadi Dafchahi M, Koochaki Nezhad L, et al. [Epidemiology of Head Injury in Patients who were Reffered to Poorsina Hospital]. J Guilan Univ Med Sci. 2008;16(64):112-9. Persian.
-
32.
Saeednejad M, Zafarghandi M, Khalili N, Baigi V, Khormali M, Ghodsi Z, et al. Evaluating mechanism and severity of injuries among trauma patients admitted to Sina Hospital, the National Trauma Registry of Iran. Chin J Traumatol. 2021;24(3):153-8. [PubMed ID: 33640244]. [PubMed Central ID: PMC8173574]. https://doi.org/10.1016/j.cjtee.2021.01.009.
-
33.
Soltani S, Aghakhani K, Rismantab Sani S, Asgari M, Fallah F. Review of Fall Injuries and Related Factors in Patients Admitted to a Trauma Referral Hospital in Tehran, Iran. Int J Med Toxicol Forensic Med. 2016;6(4):200-8.
-
34.
Hatamabadi H, Arhami Dolatabadi A, Atighinasab B, Safari S. Baseline Characteristics of fall from Height Victims Presenting to Emergency Department; a Brief Report. Emerg (Tehran). 2017;5(1):e55. [PubMed ID: 28894771]. [PubMed Central ID: PMC5585825].
-
35.
Ghaffari-Fam S, Sarbazi E, Daemi A, Sarbazi M, Riyazi L, Sadeghi-Bazargani H, et al. Epidemiological and Clinical Characteristics of Fall Injuries in East Azerbaijan, Iran; A Cross-Sectional Study. Bull Emerg Trauma. 2015;3(3):104-10. [PubMed ID: 27162912]. [PubMed Central ID: PMC4771250].
-
36.
Montazer SH, Hosseininejad SM, Bozorgi F, Assadi T, Hashemi SN, Lotfipour M, et al. Epidemiology of Injuries Caused By Motor Accidents in Patients Referred To Emergency Department of A Trauma Center Hospital in North of Iran. Int J Med Invest. 2019;8(1):10-8.
-
37.
Zandi M, Seyed Hoseini SR. The relationship between head injury and facial trauma: a case-control study. Oral Maxillofac Surg. 2013;17(3):201-7. [PubMed ID: 23100036]. https://doi.org/10.1007/s10006-012-0368-z.
-
38.
Zandi M, Khayati A, Lamei A, Zarei H. Maxillofacial injuries in western Iran: a prospective study. Oral Maxillofac Surg. 2011;15(4):201-9. [PubMed ID: 21660436]. https://doi.org/10.1007/s10006-011-0277-6.
-
39.
Jalalvandi F, Arasteh P, Safari Faramani R, Esmaeilivand M. Epidemiology of Pediatric Trauma and Its Patterns in Western Iran: A Hospital Based Experience. Glob J Health Sci. 2016;8(6):139-46. [PubMed ID: 26755468]. [PubMed Central ID: PMC4954915]. https://doi.org/10.5539/gjhs.v8n6p139.
-
40.
Hatamabadi H, Vafaee R, Hadadi M, Abdalvand A, Esnaashari H, Soori H. Epidemiologic study of road traffic injuries by road user type characteristics and road environment in Iran: a community-based approach. Traffic Inj Prev. 2012;13(1):61-4. [PubMed ID: 22239145]. https://doi.org/10.1080/15389588.2011.623201.
-
41.
Ghaem H, Soltani M, Yadollahi M, ValadBeigi T, Fakherpour A. Epidemiology and Outcome Determinants of Pedestrian Injuries in a Level I Trauma Center in Southern Iran; A Cross-Sectional Study. Bull Emerg Trauma. 2017;5(4):273-9. [PubMed ID: 29177174]. [PubMed Central ID: PMC5694600]. https://doi.org/10.18869/acadpub.beat.5.4.508.
-
42.
Abbasi HR, Mousavi SM, Taheri Akerdi A, Niakan MH, Bolandparvaz S, Paydar S. Pattern of Traumatic Injuries and Injury Severity Score in a Major Trauma Center in Shiraz, Southern Iran. Bull Emerg Trauma. 2013;1(2):81-5. [PubMed ID: 27162829]. [PubMed Central ID: PMC4771228].
-
43.
Sehat Z, Fakharian E, Sehat M, Omidi A. Epidemiology pattern of traumatic injuries of adults older than 15 years in Kashan, Iran: A population-based study in 2018-2019. Med J Islam Repub Iran. 2021;35:62. [PubMed ID: 34277499]. [PubMed Central ID: PMC8278027]. https://doi.org/10.47176/mjiri.35.62.
-
44.
Karbakhsh M, Zandi NS, Rouzrokh M, Zarei MR. Injury epidemiology in Kermanshah: the National Trauma Project in Islamic Republic of Iran. East Mediterr Health J. 2009;15(1):57-64. [PubMed ID: 19469427].
-
45.
Bunyatisai W, Chakrabandhu S, Sripan P, Rankantha A, Prasitwattanaseree S, Chitapanarux I. Spatial Distribution of Head and Neck Cancer in Chiang Mai, Thailand. Asian Pac J Cancer Prev. 2022;23(8):2583-90. [PubMed ID: 36037110]. [PubMed Central ID: PMC9741908]. https://doi.org/10.31557/APJCP.2022.23.8.2583.
-
46.
Nayak SG, Sharan K, Chakrabarty J, Devi ES, Ravishankar N, George A. Psychosocial Distress of Head Neck Cancer (HNC) Patients Receiving Radiotherapy: A Systematic Review. Asian Pac J Cancer Prev. 2022;23(6):1827-35. [PubMed ID: 35763621]. [PubMed Central ID: PMC9587841]. https://doi.org/10.31557/APJCP.2022.23.6.1827.
-
47.
Suzuki H, Kawasaki Y, Miura M, Hatakeyama H, Shina K, Suzuki S, et al. Tumor Infiltrating Lymphocytes are Prognostic Factors and Can Be Markers of Sensitivity to Chemoradiotherapy in Head and Neck Squamous Cell Carcinoma. Asian Pac J Cancer Prev. 2022;23(4):1271-8. [PubMed ID: 35485685]. [PubMed Central ID: PMC9375628]. https://doi.org/10.31557/APJCP.2022.23.4.1271.
-
48.
Alsabieh M. Traumatic Spinal Injuries in Saudi Arabia: A Retrospective Single-center Medical Record Review. Journal of Spine Practice. 2021;1(1):43. https://doi.org/10.18502/jsp.v1i1.9801.
-
49.
Alhabeeb A. Consequences of Delayed Surgical Treatment of Traumatic Spinal Cord Injuries: Tertiary Centre Experience. Journal of Spine Practice. 2021;1(1):5. https://doi.org/10.18502/jsp.v1i1.9765.
-
50.
Aoki M, Abe T, Saitoh D, Oshima K. Epidemiology, Patterns of treatment, and Mortality of Pediatric Trauma Patients in Japan. Sci Rep. 2019;9(1):917. [PubMed ID: 30696939]. [PubMed Central ID: PMC6351578]. https://doi.org/10.1038/s41598-018-37579-3.
-
51.
Langlois JA, Rutland-Brown W, Thomas KE. The incidence of traumatic brain injury among children in the United States: differences by race. J Head Trauma Rehabil. 2005;20(3):229-38. [PubMed ID: 15908823]. https://doi.org/10.1097/00001199-200505000-00006.
-
52.
Thurman DJ. The Epidemiology of Traumatic Brain Injury in Children and Youths: A Review of Research Since 1990. J Child Neurol. 2016;31(1):20-7. [PubMed ID: 25123531]. https://doi.org/10.1177/0883073814544363.
-
53.
Haarbauer-Krupa J, Lee AH, Bitsko RH, Zhang X, Kresnow-Sedacca MJ. Prevalence of Parent-Reported Traumatic Brain Injury in Children and Associated Health Conditions. JAMA Pediatr. 2018;172(11):1078-86. [PubMed ID: 30264150]. [PubMed Central ID: PMC6248161]. https://doi.org/10.1001/jamapediatrics.2018.2740.
-
54.
Gerritsen H, Samim M, Peters H, Schers H, van de Laar FA. Incidence, course and risk factors of head injury: a retrospective cohort study. BMJ Open. 2018;8(5):e020364. [PubMed ID: 29858414]. [PubMed Central ID: PMC5988084]. https://doi.org/10.1136/bmjopen-2017-020364.
-
55.
Baiden F, Anto-Ocrah M, Adjei G, Gyaase S, Abebrese J, Punguyire D, et al. Head Injury Prevalence in a Population of Injured Patients Seeking Care in Ghana, West Africa. Front Neurol. 2022;13:917294. [PubMed ID: 35812104]. [PubMed Central ID: PMC9266767]. https://doi.org/10.3389/fneur.2022.917294.