Effects of biofilm formation and plethora of Candida species causing ailments: a mini review
DOI:
https://doi.org/10.54117/gjpas.v1i2.27Keywords:
Candida species, Biofilm formation, Mortality rate, Candida albicans, EpidemiologyAbstract
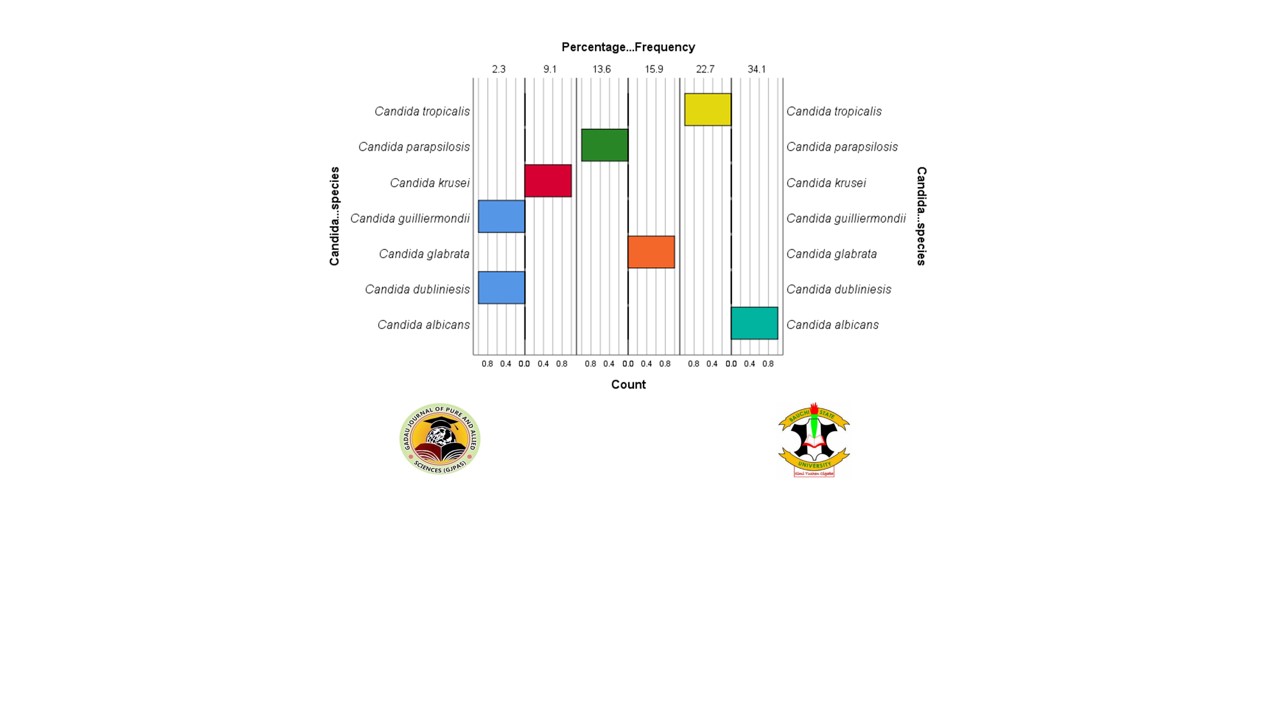
Biofilm formation is an independent predictor of higher mortality rate and significant virulence factor that increase the dissemination ability and persistence of Candida species. However, Candida species distribution differs in population based studies evaluated in different geographical locations. This study aimed to evaluate the biofilm associated mortality rate, spectrum and resistance profile of Candida species. A systemic literature review was carried out to evaluate all current epidemiology that reports the incidence of the biofilm associated mortality rate, spectrum and resistance profile of Candida species. Several studies used optical density of the biomass from culture to measure biofilm formation. Data regarding the prevalence of Candida species, in vitro biofilm assay and rate of biofilm-related Candida species in clinical isolates were also extracted from the case-control, cohort, and retrospective studies. The result of this study shows that the mortality rate due to biofilm associated infections ranged from 6.9% to 70.0% and biofilm formation varied greatly from 27.2% to 100% evaluated from different published studies. Candida albicans was the predominant pathogen and the percentage frequency of the isolates ranged from 36.3% to 78.5%. The distribution of Candida species from 2016 to 2020 revealed that Candida albicans (39.42%) had the highest percentage frequency. High prevalence of Candida species was reported in 2018 (28.2%). The current data revealed that United Kingdom, Spain, Austria and Norway shows resistance profile for Candida tropicalis, Candida albicans, Candida parapsilosis and Candida glabrata. Biofilm formation is considered as potential risk factor of higher mortality rate and effective antifungal agents to eliminate or reduce this menace is urgently needed. The reports of the biofilm-forming potentials and properties among Candida species could provide a remarkable step toward the improvement of Candida infection therapies.
References
Arendrup, M.C. and Patterson, T.F. (2017). Multidrug-Resistant Candida: Epidemiology, Molecular Mechanisms, and Treatment. Journal of Infectious Diseases 216: S445–S451.
Atiencia-Carrera, M.B., Cabezas-Mera, F.S., Tejera, E. and Machado, A. (2022). Prevalence of biofilms in Candida spp. bloodstream infections: A meta-analysis. PLoS ONE 17(2): 1-23.
Badiee, P. and Alborzi, A. (2011). Susceptibility of clinical Candida species isolates to antifungal agents by E-test, Southern Iran: A five year study. Iranian Journal of Microbiology 3: 183–8.
Banerjee, B., Saldanha, Dominic, R.M. and Baliga, S. (2015). Clinico-microbiological study of candidemia in a tertiary care hospital of southern part of India. Iranian Journal of Microbiology 7: 55.
Berenguer, J., Buck, M., Witebsky, F., Stock, F., Pizzo, P.A. and Walsh, T.J. (1993). Lysis-centrifugation blood cultures in the detection of tissue-proven invasive candidiasis. Disseminated versus single-organ infection. Diagnostic Microbiology Infectious Disease 17: 103–109.
Bitew, A. and Abebaw, Y. (2018). Vulvovaginal candidiasis: Species distribution of Candida and their antifungal susceptibility pattern. Women Health 18: 94.
Bongomin, F., Gago, S., Oladele, R.O. and Denning, D.W. (2017). Global and Multi-National Prevalence of Fungal Diseases-Estimate Precision. Journal of Fungi 3(4): 57.
Chandra, J. and Mukherjee, P.K. (2015). Candida Biofilms: Development, Architecture, and Resistance. Microbiology Spectrum 3: 1–14.
Chi, H-W., Yang, Y-S., Shang, S-T., Chen, K-H., Yeh, K-M., Chang, F-Y., et al. (2011). Candida albicans versus non-albicans bloodstream infections: The comparison of risk factors and outcome. Journal of Microbiology Immunology and Infection 44: 369e375.
Das, K.H., Getso, M.I. and Azeez-Akande, O. (2016). Distribution of Candida albicans and non-albicans Candida in clinical samples and their intrinsic biofilm production status. International Journal of Medical Sciences and Public Health 5: 2443–244.
ElFeky, D.S., Gohar, N.M., El-Seidi, E.H., Ezzat, M.M., Hassan, S. and AboElew, S.H. (2016). Species identification and antifungal susceptibility pattern of Candida isolates in cases of vulvovaginal candidiasis. Alexandria Journal of Medicine 52: 269–77.
Galia, L., Pezzani, A.M., Compri, M., Callegari, A., Rajendran, B.N., Carrera, E., Tacconelli, E. and the COMBACTE MAGNET EPI-Net Network. (2022). Surveillance of antifungal resistance in candidemia fails to inform antifungal stewardship in European countries. Journal of Fungi 8(249): 1 – 12.
Ghrenassia, E., Mokart, D., Mayaux, J., Demoule, A., Rezine, I., Kerhuel, L., et al. (2019). Candidemia in critically ill immunocompromised patients: report of a retrospective multicenter cohort study. Ann Intensive Care 9: 62.
Godoy, P., Tiraboschi, I.N., Severo, L.C., Beatriz-Bustamante, B., Calvo, B., de Almeida, L.P., et al. (2003). Species Distribution and Antifungal Susceptibility Profile of Candida spp. Bloodstream Isolates from Latin American Hospitals. Memorias do Instituto Oswaldo Cruz 98: 401 –5.
Guembe, M., Guinea, J., Marcos-Zambrano, L., Fernandez-Cruz, A., Pelaez, T., Munoz, P., et al. (2014). Is Biofilm Production a Predictor of Catheter-Related Candidemia? Medical Mycology 52: 407–410.
Guinea J. (2014). Global trends in the distribution of Candida species causing candidemia. Clinical Microbiology and Infection 20(6): 5 – 10.
Herek, C.T., Managazzo, R.V., Ogaki, B. M., Perini, F.H., Maia, F.L. and Furlaneto C.M. (2019). Biofilms formation by blood isolates of Candida parapsilosis sensu stricto in the presence of a hyperglycidic solution at comparable concentrations of total parenteral nutrition. Journal of the Brazilian Society of Tropical Medicine 52(e-20180182): 1 – 5.
Jensen, R.H., Johansen, H.K., Soes, L.M., Lemming, L.E., Rosenvinge, F.S., Nielsen, L., Olesen, B., Kristensen, L., Dzajic, E., Astvad, K.M., et al. (2015). Post-treatment Antifungal Resistance among Colonizing Candida Isolates in Candidemia Patients: Results from a Systematic Multicenter Study. Antimicrobial Agents and Chemotherapy 60: 1500–1508.
Johnson, C.J., Cabezas-Olcoz, J., Kernien, J.F., Wang, S.X., Beebe, D.J., Huttenlocher, A., et al. (2016). The Extracellular Matrix of Candida albicans Biofilms Impairs Formation of Neutrophil Extracellular Traps. PLoS Pathogens 12: 1–23.
Kaur, R., Dhakad, M.S. and Goyal-Kumar, R.R. (2016). Emergence of non-albicans Candida species and antifungal resistance in intensive care unit patients. Asian Pacific Journal of Tropical Biomedicine 6: 455–60.
Koehler, P., Stecher, M., Cornely, O.A., Koehler, D., Vehreschild, M., Bohlius, J., Wisplinghoff, H. and Vehreschild, J.J. (2019). Morbidity and mortality of candidaemia in Europe: An epidemiologic meta-analysis. Clinical Microbiology and Infection 25: 1200–1212.
Lagunes, L. and Rello, J. (2016). Invasive candidiasis: From mycobiome to infection, therapy, and prevention. European Journal of Clinical Microbiology and Infectious Diseases. Springer Verlag 1221-1226.
Mamali, V., Siopi, M., Charpantidis, S., Samonis, G., Tsakris, A., Vrioni, G. and on behalf of the Candi-Candi Network. (2022). Increasing incidence and shifting epidemiology of candidemia in Greece: Results from the first nationwide 10 years survey. Journal of Fungi 8(116): 1-20.
Marak, M.B. and Dhanashree, B. (2018). Antifungal Susceptibility and Biofilm Production of Candida spp. Isolated from Clinical Samples.
Mohandas, V. and Ballal, M. (2011). Distribution of Candida Species in different clinical samples and their virulence: Biofilm formation, proteinase and phospholipase production: A study on hospitalized patients in Southern India. Journal of Global Infectious Diseases 3: 4–8.
Muadcheingka, T. and Tantivitayakul, P. (2015). Distribution of Candida albicans and non-albicans Candida species in oral candidiasis patients: Correlation between cell surface hydrophobicity and biofilm forming activities. Archives of oral biology 60: 894–901.
Mulu, A., Kassu, A., Anagaw, B., Moges, B., Gelaw, A., Alemayehu, M., et al. (2013). Frequent detection of ‘azole’ resistant Candida species among late presenting AIDS patients in northwest Ethiopia. BMC Infectious Diseases 13: 82.
Nobile, C.J. and Johnson, A.D. (2015). Candida albicans Biofilms and Human Disease. Annual Review of Microbiology 69:71–92.
Pappas, P.G., Kauffman, C.A., Andes, D.R., Clancy, C.J., Marr, K.A., Ostrosky-Zeichner, L., et al. (2015). Clinical Practice Guideline for the Management of Candidiasis: 2016 Update by the Infectious Diseases Society of America. Clinical Infectious Diseases 62: e1–e50.
Pfaller, M.A. and Diekema, D.J. (2007). Epidemiology of invasive candidiasis: a persistent public health problem. Clinical Microbiology Reviews 20: 133–163.
Pham, L.T. T., Pharkjaksu, S., Chongtrakool, P., Suwannakarn, K. and Ngamskulrungroj, P. (2019). A Predominance of Clade 17 Candida albicans Isolated From Hemocultures in a Tertiary Care Hospital in Thailand. Frontiers in Microbiology 10(1194): 1 – 9.
Polke, M., Hube, B. and Jacobsen, I.D. (2015). Candida survival strategies. Advances in Applied Microbiology. Elsevier Ltd.
Prigitano, A., Dho, G., Lazzarini, C., Ossi, C., Cavanna, C. and Tortorano, A.M. (2012). Biofilm production by Candida isolates from a survey of invasive fungal infections in Italian intensive care units. Journal of Chemotherapy 24: 61–63.
Puig-Asensio, M., Padilla, B., Garnacho-Montero, J., et al. (2014). Epidemiology and predictive factors for early and late mortality in Candida bloodstream infections: a population-based surveillance in Spain. Clinical Microbiology and Infection 20(4): 0245 – 54.
Rajendran, R., Sherry, L., Nile, C.J., Sherriff, A., Johnson, E.M., Hanson, M.F., et al. (2016). Biofilm formation is a risk factor for mortality in patients with Candida albicans bloodstream infection-Scotland, 2012–2013. Clinical Microbiology and Infection 22: 87–93.
Rees, J.R., Pinner, R.W., Hajjeh, R.A., Brandt, M.E. and Reingold, A.L. (1998). The epidemiological features of invasive mycotic infections in the San Francisco bay area, 1992-1993: results of population-based laboratory active surveillance. Clinical Infectious Diseases 27: 1138–1147.
Ribeiro, A.L.R., de Alencar-Menezes, T.O., de Melo Alves-Junior, S., de Menezes, S.F., Silvia Helena Marques-da-Silva, S.H. and Rosario Vallinoto, A.C.R. (2015). Oral carriage of Candida species in HIV-infected patients during highly active antiretroviral therapy (HAART) in Belém, Brazil. Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology 120: 29–33.
Richter S.S., Galask, P.R., Messer A.S., Hollis, J.R., Diekema, J.D. and Pfaller A.M. (2005). Antifungal susceptibilities of Candida species causing vulvovaginal and epidemiology of recurrent cases. Journal of Clinical Microbiology 43(5): 2155 – 2162.
Rodrigues, C.F., Silva, S. and Henriques, M. (2014). Candida glabrata: A review of its features and resistance. European Journal of Clinical Microbiology and Infectious Diseases 33: 673–688.
Schmalrec, A.F., Willinger, B., Haase, B.G., Lass-Flo, C., Feeler, K., et al. (2012). Species and susceptibility distribution of 1062 clinical yeast isolates to azoles, echinocandins, flucytosine and amphotericin B from a multi-centre study. Mycoses 55: e124–37.
Seyoum, E., Bitew, A. and Mihret, A. (2020). Distribution of Candida albicans and non-albicans Candida species isolated in different clinical samples and their in vitro antifungal susceptibility profile in Ethiopia. Infectious Diseases 20(231): 1 – 9.
Sida, H., Pethani, J., Dalal, P. and Hiral, S.H. (2017). Study of Changing Trend in the Clinical Distribution of Candida Species in Various Clinical Samples at Tertiary Care Hospital, Ahmedabad, Gujarat. National Journal of Community Medicine 8:109–11.
Silva, S., Negri, M., Henriques, M., Oliveira, R., Williams, D.W. and Azeredo, J. (2012). Candida glabrata, Candida parapsilosis and Candida tropicalis: Biology, epidemiology, pathogenicity and antifungal resistance. FEMS Microbiology Reviews 36: 288–305.
Silva, S., Rodrigues, C.F., Araujo, D., Rodrigues, M.E. and Henriques, M. (2017). Candida species biofilms’ antifungal resistance. Journal of Fungi 3:8.
Soldini, S., Posteraro, B., Vella, A., De Carolis, E., Borghi, E., Falleni, M., et al. (2018). Microbiologic and clinical characteristics of biofilm-forming Candida parapsilosis isolates associated with fungaemia and their impact on mortality. Clinical Microbiology and Infection 24(7): 771 – 777.
Tascini, C., Sozio, E., Corte, L., Sbrana, F., Scarparo, C., Ripoli, A., Bertolino, G., Merelli, M., Tagliaferri, E., Corcione, A., Bassetti, M., Cardinali, G. and Menichetti, F. (2017). The role of biofilm forming on mortality in patients with candidemia: a study derived from real world data. Infectious Diseases 50(3): 1 – 6.
Thompson, A., Davies, L.C., Liao, C-T., da Fonseca, D.M., Griffiths, J.S., Andrews, R., et al. (2019). The protective effect of inflammatory monocytes during systemic C. albicans infection is dependent on collaboration between C-type lectin-like receptors. Hohl TM, editor. PLOS Pathogens 15: e1007850.
Tortorano, A.M., Prigitano, A., Lazzarini, C., Passera, M., Deiana, M.L., Cavinato, S., et al. (2013). A 1-year prospective survey of candidemia in Italy and changing epidemiology over one decade. Infection 41: 655– 662.
Trevino-Rangel, J.R., Espinosa-Perez, F.J., Villanueva-Lozano, H., Montoya, M.A., Andrade, A., Bonifaz A. and Gonzalez M.G. (2018). First report of Candida bracarensis in Mexico: hydrolytic enzymes and antifungal susceptibility pattern. Folia Microbiologica 63(4):1 – 8.
Tsay, S.V., Mu, Y., Williams, S., Epson, E., Nadle, J., Bamberg, W.M., et al. (2020). Burden of Candidemia in the United States, 2017. Clinical Infectious Diseases 71: e449–e453.
Tulasidas, S., Rao, P., Bhat, S. and Manipura, R. (2018). A study on biofilm production and antifungal drug resistance among Candida species from vulvovaginal and bloodstream infections. Infection and Drug Resistance 11: 2443 – 2448.
Tumbarello, M., Fiori, B., Trecarichi, E.M., Posteraro, P., Losito, A. R., de Luca, A., et al. (2012). Risk factors and outcomes of candidemia caused by biofilm-forming isolates in a tertiary care hospital. PLoS One 7: 1–9.
Tumbarello, M., Posteraro, B., Trecarichi, E.M., Fiori, B., Rossi, M., Porta, R., et al. (2007). Biofilm production by Candida species and inadequate antifungal therapy as predictors of mortality for patients with candidemia. Journal of Clinical Microbiology 45: 1843–1850.
Vitalis, E., Nagy, F., Toth, Z., Forgacs, L., Bozo, A., Kardos, G., et al. (2020). Candida biofilm production is associated with higher mortality in patients with candidaemia. Mycoses 63: 352–360.
Yardimci, C.A. and Arman, D. (2021). Changing trends of Candida species and antifungal susceptibility profile of Candida bloodstream isolates: A 5 – year retrospective survey. Jundishapur Journal of Microbiology 14(12): e120801
Zeng, X., Zhang, Y., Kwong, J.S. W., Zhang, C., Li, S., Sun, F., et al. (2015). The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: A systematic review. Blackwell Publishing. Journal of Evidence-Based Medicine 2–10.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Gadau Journal of Pure and Allied Sciences

This work is licensed under a Creative Commons Attribution 4.0 International License.