Article / Case Report
1Private Practice in Oral, Maxillofacial and Reconstructive Surgery. Aiea, Hawaii 96701. USA
2The Queen’s Medical Center. Honolulu, Hawaii 96813. Associate Clinical Professor of Pathology. John A Burns School of Medicine. University of Hawaii. Honolulu, Hawaii 96813, USA
Cameron Y. S. Lee, DMD, MD, PHD, MPH, MSEd
Private Practice in Oral Maxillofacial and Reconstructive Surgery. Aiea, Hawaii 96701. USA
Professor of Surgery. Department of Periodontology and Oral Implantology. Kornberg School of Dentistry, Temple University, Philadelphia, PA 19140. USA
18 January 2021 ; 5 February 2021
Condyloma acuminatum (CA) is a sexually transmitted infection (STI) that results in psychosocial distress. The etiologic agent is the human papillomavirus (HPV), genotypes 6 and 11. Sexually transmitted infections from the HPV are the world’s most common infection. Infections occur on the skin, and mucous membranes of the genital and perianal region, and less frequently in the oral cavity. But, with an increase in oral sexual practices with infected partners of all ages, CA should be considered in the differential diagnosis of oral lesions. The mode of transmission is through oral sex. Dental clinicians will often be the first healthcare provider to detect lesions in the oral cavity, especially HPV origin. In addition to obtaining a complete medical and dental history, histopathologic diagnosis will enable the healthcare team in arriving at an accurate diagnosis of CA. In this case report, we diagnose condyloma acuminatum in a geriatric female who was unaware of the STI on the left buccal mucosa of the cheek that was treated by complete surgical excision.
Keywords: Geriatric patient, Sexually transmitted infection, Human papillomavirus, Condyloma acuminatum, Oral Cavity, Histopathology
Globally, human papillomavirus (HPV) infection is the most common etiologic agent for sexually transmitted infections [1]. In the United States, it is estimated that there are greater than 6.2 million cases diagnosed per year [2]. However, infections can progress and usually result in condyloma on the genital and perianal regions [3]. Condyloma acuminatum is infectious, as 65% of men or women will become infected from their sexual partner [4]. The virus can infect epithelia and mucosa resulting in slow, benign proliferations of stratified squamous epithelium frequently observed on the skin, anogenital area and oral cavity [5-7]. HPV-induced oral infections are associated with the risk of developing cancer of the oral cavity [8,9].
HPV is the viral etiologic agent for condyloma acuminatum (CA) commonly observed on the skin and anogenital region [10,11]. Condyloma acuminatum (also known as venereal wart) beyond the anogenital region is less frequently observed [12-14].The common mode of transmission is through oral sex between sexual partners. As unwanted pregnancy is no longer a concern in the geriatric female patient, sexually active senior citizens are still vulnerable to sexually transmitted infections (STIs).
Mucosal lesions of the oral cavity are often asymptomatic and can affect the lips, tongue, floor of mouth, buccal mucosa of the cheeks, soft palate, and the gingiva [6,12,14,15,16]. The papillomatous growths can be composed of small solitary papules or grouped together with a sessile or pedunculated base to large pedunculated growths [6,12,15]. Upon clinical presentation, condyloma may appear similar to squamous papilloma, verruca vulgaris, verruciform xanthoma, focal epithelial hyperplasia, verrucous hyperplasia, and verrucous carcinoma.
We report a case of condyloma acuminatum in the oral cavity in a female geriatric patient.
The human papillomavirus is a 55nm non-enveloped icosahedral double-stranded deoxyribonucleic acid (DNA) virus [17, 18]. There are over 150 genotypically different types and classified as either mucosal or cutaneous [19-21]. Oral condyloma infection is associated with HPV subtypes 6 and 11 [7, 22]. Papillomas induced by HPV types 6 and 11 are considered to have low oncogenic potential. However, approximately 85% of dysplastic lesions, carcinoma in situ and squamous cell carcinoma involve the DNA sequence of HPV 16 and 18. DNA replication of HPV occurs in the nuclei of the basal epithelial cells. The HPV capsid proteins enter the host cell delivering the viral DNA to the nucleus which allows proliferation of the viral lesion [17, 19, 20, 21].

Figure 1: Intraoral photograph of condyloma on left buccal mucosa of cheek
A 66-year old female was referred to the office by her family dentist for evaluation of multiple raised papules on the left buccal mucosa of the cheek near the commissure (Figure 1). The patient stated that she did not know how long the lesion was present. Her past medical history was unremarkable. She was not taking any medications and denied any allergy to medications. The patient admits to being sexually active with multiple partners.
Head and neck examination were negative for palpable neck masses and lymphadenopathy. Oral examination revealed multiple pink colored pedunculated papules on the buccal mucosa of the cheek near the commissure. The surface texture had a pebbly appearance that resembled, “cauliflower”. The remaining oral examination was unremarkable. Based on the clinical appearance of the lesion, the differential diagnosis included squamous papilloma, verruca vulgaris, verruciform xanthoma, focal epithelial hyperplasia, papillary hyperplasia and condyloma acuminatum. The patient was informed of the clinical findings and recommendation of excisional biopsy to obtain a definitive microscopic diagnosis under local anesthesia.
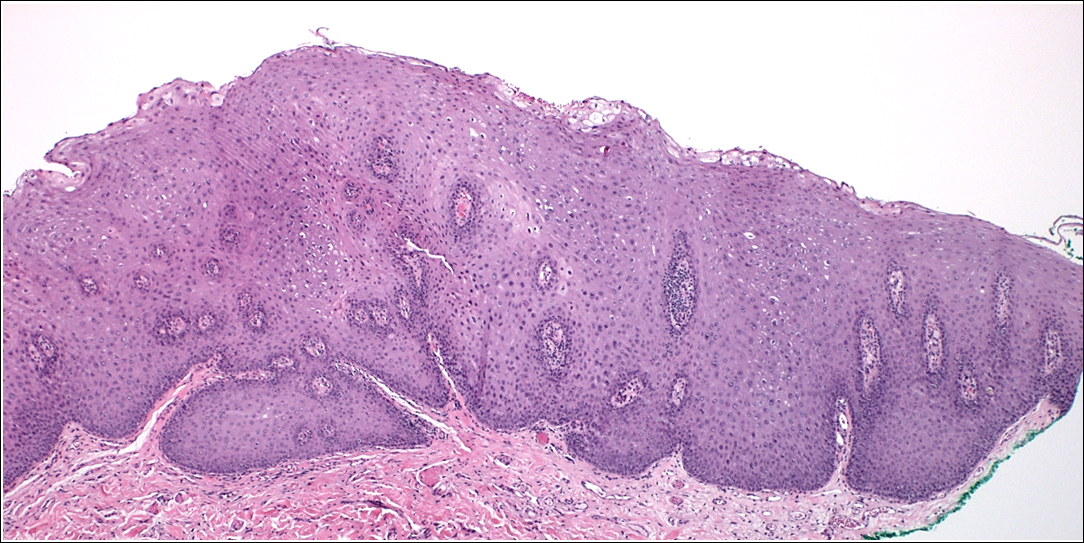
Figure 2A: Biopsy of condyloma from left cheek. Irregular epithelial thickening with acanthosis and marked papillomatosis with nonuniform perinuclear halos. Hematoxylin and eosin, 400x.
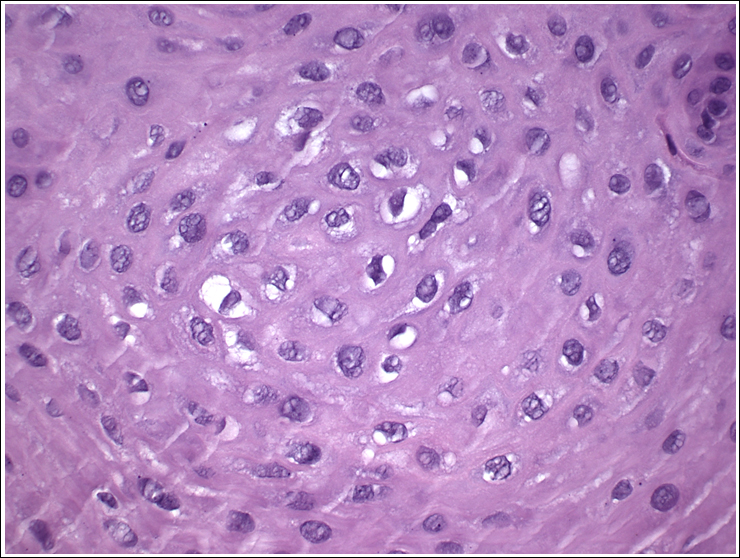
Figure 2B: High power view demonstrating viral infected cells (koilocytes). Note nonuniform perinuclear cytoplasmic halos and hyperchromatic nuclei. Hematoxylin and eosin, 1000x.
Excisional biopsy was completed under local anesthesia with 1.0 mm margins of normal tissue and to the depth of the orbicularis oris muscle. The lesion was stained with hematoxylin and eosin for histopathologic diagnosis. Histological examination demonstrated papillary projections of parakeratinized stratified squamous epithelium with acanthosis (Figure 2A). Cells variable in size with nonuniform perinuclear halos and hyperchromatic nuclei were observed (koilocytes) (Figure 2B). The histological findings were consistent with condyloma acuminatum. The patient was referred to an infectious disease specialist for further evaluation of sexually transmitted infections of the female reproductive tract.
Human papilloma virus affects all age groups and condyloma acuminatum is a sexually transmitted infection caused by HPV 6 and 11 in patients who engage in oral sex [6, 23, 24]. Transmission of the HPV to the oral cavity can occur through oral sex, autoinoculation, and rarely, perinatal transmission through the birth canal [6, 13, 14]. Non-sexual transmission of HPV oral lesions can also occur by autoinoculation from lesions on the genitals via hand to mouth, and perinatal transmission [25].
Histopathologic features of oral condyloma acuminatum demonstrate papillomatosis, and the primary diagnostic feature, koilocytosis, which are cells with nonuniform perinuclear halos of variable size and hyperchromicity [24, 26, 27]. The characteristic feature of CA infection is the presence of koilocytes (Figure 2B) which are virus-infected epithelial cells with perinuclear cytoplasmic vacuolization of cells of the spinous layer of the epithelium. This results in the nuclei becoming pyknotic and cremated surrounded by an optically clear zone [7,23,28] .The histopathologic findings in our patient are characteristic of HPV-induced condyloma acuminatum.
A case of oral condyloma acuminatum of a 66-year old female is presented to create awareness of this sexually transmitted infection in the oral cavity of a geriatric patient due to the human papillomavirus. Educating clinicians and senior citizens about the HPV and condyloma acuminatum will create greater awareness that despite their advanced age group, they are not immune to sexually transmitted infections.
- World Health Organization (2007). International Agency for Research on Cancer (IARC). Human Papillomaviruses. IARC. Monogr Eval Carcinog Risk Hum, 90:47-79.
- Cates W Jr (1999). Estimates of the incidence and prevalence of sexually transmitted diseases in the United States. American Social Health Association Panel. Sex Transm Dis, 26:S2-7.
- Dunne EF, Nielson CM, Stone KM, et. al (2006). Prevalence of HPV infection among men: A systematic review of the literature. J Infect Dis, 194:1044-57.
- Scheurer ME, Tortolero-Luna G, Adler-Storthz K (2005). Human papillomavirus infection: biology, epidemiology, and prevention. Int J Gynecol Cancer, 15:727-46.
- Oriel JD (1971). Natural history of genital warts. Br J Vener Dis, 47:1-13.
- Abbey LM, Page DG, Sawyer DR (1980). The clinical and histopathologic features of a series of 464 oral squamous cell papillomas. Oral Surg Oral Med Oral Pathol 49(5):419-428.
- Zunt SL, Tomich CE (1989). Oral condyloma acuminatum. J Dermatol Surg Oncol, 15:591-594.
- Neville BW, Damm DD, Allen CM (2009). Epithelial pathology. In: Textbook of oral and maxillofacial pathology. Ed 3rd. Elsevier, pp. 362- 364.
- de Villiers EM, Faquet C, Broker TR, et. al (2004). Classification of papillomaviruses. Virology, 324:17–27.
- Della Torre G, Pilotti S, De Palo G (1978). Viral particle in condylomatous lesions. Tumori, 64:549-555.
- Sehgal VN, Koranne RV, Srivastava SB. Genital warts (1989). Current status. Int J Dermatol, 28:75-78.
- Knapp MJ, Uohara GI (1967). Oral condyloma acuminatum. Oral Surg Oral Med Oral Pathol, 232(4):538-545.
- Choukas NC, Toto PD (1982). Condylomata acuminatum of the oral cavity. Oral Surg Oral Med Oral Pathol, 54(4):480-485.
- Butler S, Molinari JA, Plezia RA, et. al (1988). Condyloma acuminatum in the oral cavity: Four cases and a review. Rev Infect Dis, 10(3):544-550.
- Manganaro AM (2000). Oral condyloma acuminatum. Gen Dent, 48:62-64.
- Flaitz CM (2001). Condyloma acuminatum of the floor of the mouth. Am J Dent, 14:115-116.
- Sanclemente G, Gill DK (2002). Human papillomavirus molecular biology and pathogenesis. J Eur Acad Dermatol Venereol, 16(3):231-240.
- Carneiro TE, Marinho SA, Verli FD, Mesquita AT, Lima NL, et. al (2009). Oral squamous papilloma: Clinical, histologic, and immunohistochemical analyses. J Oral Sci 51(3):367-372.
- Swygart C (1997). Human papillomavirus: disease and laboratory diagnosis. Br J Biomed Sci 54(4):299-303.
- Mammas IN, Sourvinos G, Spandidos D (2014). The paediatric story of human papilloma virus (HPV). Oncol Lett 8(2):502-506.
- Feller L, Hammissa RA, Wood NH, Lemmer J (2009). Epithelial maturation and molecular biology of oral HPV. Infect Agent Cancer 4:16-23.
- Major T, Szarka K, Sziklai I, Gergely L, Czegledy J (2005). The characteristics of human papillomavirus DNA in head and neck cancers and papillomas. J Clin Pathol 58(1):51-55.
- Abbey LM, Page DG, Sawyer DR (1980). The clinical and histopathologic features of a series of 464 oral squamous cell papillomas. Oral Surg Oral Med Oral Pathol, 49(5):419-428.
- Anderson KM, Perez-Montiel D, Miles L, et. al (2003). The histologic differentiation of oral condyloma acuminatum from its mimics. Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 96:420-428.
- Panici PB, Scambia G, Perrone L, et. al (1992). Oral condyloma lesions in patients with extensive genital human papillomavirus infection. Am J Obstet Gynecol, 167(2):451-458.
- Nuovo GJ (1990). Human papillomavirus DNA in genital tract lesions histologically negative for condylomata: analysis by in situ, Southern blot hybridization and the polymerase chain reaction. Am J Surg Pathol, 14:643-651.
- Nuovo GJ, Gallery F, MacConnell P (1992). Detection of amplified HPV 6 and 11 DNA in vulvar lesions by hot start PCR in situ hybridization. Mod Pathol, 5:444-448.
- Park JS, Hur S (2013). Up to date: Comprehensive knowledge of human papillomavirus. Expert Rev Vaccines, 12(4):353-355.