Orbital Exenterations in the Treatment of Extended Palpebral Basocellular Carcinoma: About 8 Cases
Opango Alban Déo Christian*, Bosco Nshimirimana, Boutayna Bendali, Maryame Elboukhani, Zakaria Aziz and Nadia Mansouri Hattab
1Department of Stomatology and maxillofacial surgery department, Mohammed VI University Hospital, Morocco
Received Date: 06/05/2024; Published Date: 19/09/2024
*Corresponding author: Alban Déo Christian Opango, Doctor, Department of Stomatology and maxillofacial surgery department, Mohammed VI University Hospital, Marrakech 40000, Morocco
Abstract
Orbital exenteration is a disfiguring surgical procedure consisting of resecting the entire orbital contents. We report a series of 8 cases of eyelid BCC with orbital extension having benefited from orbital exenteration.
Exenteration was total in 75% of cases, enlarged in 25% of cases. The main methods of reconstruction were the temporalis muscle flap with skin graft (62.5%) and directed healing (37.5%). The development was generally favorable. The patients were referred for aesthetic rehabilitation with an orbital prosthesis.
Orbital exenteration is a deteriorating technique indicated in cancers such as extensive eyelid BCC. Although new conservative approaches such as surgery with preservation of the eyeball with radiotherapy or targeted therapies offer an interesting alternative in the management of eyelid BCCs, orbital exenteration still retains its indications. It poses the real challenge of aesthetic rehabilitation, for which osteointegrated prostheses constitute the gold standard.
Keywords: Orbital exenteration; Cancer; Basal cell carcinoma; Reconstruction; Aesthetic rehabilitation
Introduction
Orbital exenteration is a deteriorating surgical procedure consisting of resecting the entire orbital contents and its annexes by subperiosteal dissection, leaving the bony walls of the orbit exposed. It is generally indicated in the management of orbital malignancies, particularly Basal Cell Carcinomas (BCC). It poses the essential problem of post-surgical rehabilitation. The aim of this work is to show the approach of the Stomatology and maxillofacial surgery department of the Mohammed VI University Hospital in Marrakech in the PEC of eyelid BCCs with orbital extension.
We report a series of 8 patients treated in the stomatology and maxillofacial surgery department of the Mohammed VI University Hospital in Marrakech (Morocco) for eyelid BCCs extended by orbital exenteration.
Case Series
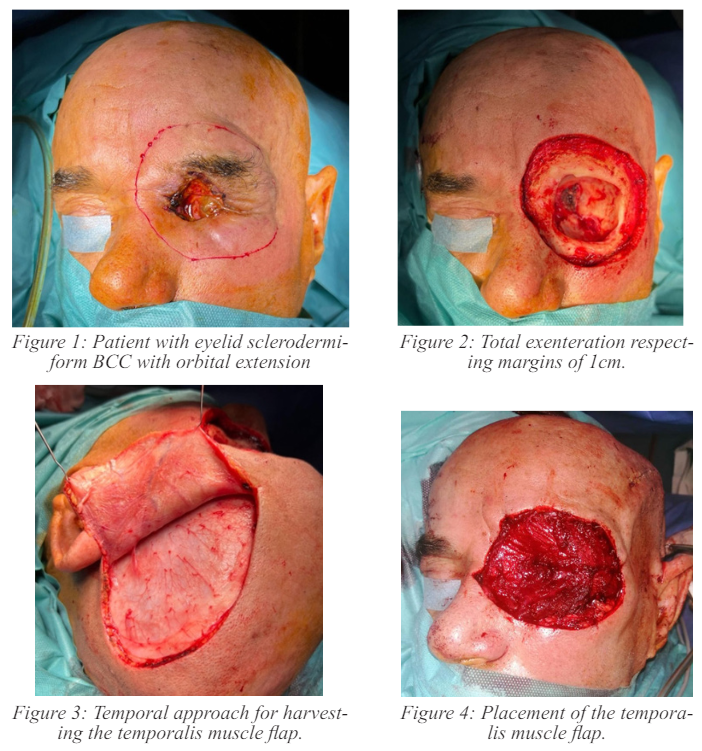
The average age was 63.5 years with extremes of 39 and 76 years. Fifty percent of patients were between 60 and 76 years old. There was a clear male predominance with a sex ratio of 3. The notion of sun exposure was found in all patients, one patient was albino. They all consulted for an ulcerative budding lesion of the eyelid. It was a sclerodermiform Basal Cell Carcinoma (BCC) in 50% of cases, a nodular BCC in 37.5% of cases and a follicular BCC in 12.5% of cases. Imaging, notably oculo-orbital MRI, showed extension of the eyelid tumor into the orbit with infiltration of intraorbital fat and the eyeball (Case 1).
After obtaining informed consent, all patients underwent excision of the eyelid tumor with orbital exenteration under general anesthesia. It was a total exenteration in 75% of cases, and enlarged in 25% of cases (2 cases). It was enlarged to the medial wall of the orbit in one case, and to the medial and inferior walls of the orbit in the other case. The safety margins varied between 5 and 10mm depending on the histological subtype of BCC (10mm for sclerodermiform BCCs and 5mm for nodular and follicular BCCs) (Figure 1, 2). The pathological examination of the surgical specimen showed healthy and sufficient margins in all cases.
As a means of reconstruction, we used directed healing in 37.5% of cases. The temporalis muscle flap with skin graft was used in 62.5% of cases (Figure 3, 4). The reconstruction was either carried out at the same operating time or delayed.
The evolution was good in 75% of cases. We noted a case of post-operative superinfection managed by antibiotic therapy and local care, a case of partial necrosis of the temporalis muscle flap with failure to take up the skin graft, subsequently left in directed healing. No cases of tumor recurrence were noted during the follow-up period.
All patients were referred for rehabilitation by orbital prosthesis to specialized anaplastologists.
Discussion
First described in 1583 by Bartische, exenteration is a complex and disfiguring procedure [1]. It involves the removal of the globe and all orbital contents, including muscles, fat, optic nerve, lacrimal gland, nerves, periorbita [2]. Rare, we report 8 cases over 3 years, i.e., an annual average of 2.6 cases in our series. Zhang Z and colleagues report a frequency of 2.5 cases per year in their series [3]. The average age in our series is 63.5 years, which corresponds to many authors [4-6]. Male predominance is accepted by all [7].
Orbital exenteration is indicated in the treatment of malignant tumors invading the orbit. It was only CBC in our series. BCC is the most common indication for orbital exenteration worldwide, followed by squamous cell carcinoma, melanoma, sebaceous carcinoma, lacrimal gland carcinoma [8-10]. Recently, more and more authors [11-12] adopt globe-sparing surgery combined with radiotherapy in extensive BCCs with orbital extension. This protocol seems to give encouraging results at the cost of serious complications (disabling diplopia, keratitis, radiological retinopathy, optic neuropathy, neovascular glaucoma) sometimes justifying secondary enucleation. Targeted therapies also, notably Vismodegib, alone or as neoadjuvant treatment in extensive BCC, also seem to give interesting results with significant side effects [13-15]. The protocols are not yet properly defined.
Regarding orbital exenterations, although many classifications exist, there are 3 essential types. Total orbital exenteration which concerns the entire orbital contents and the eyelids, sub-total exenteration which preserves the eyelids and enlarged exenteration which extends to neighboring structures (bony walls of the orbit, sinus cavities, cranial cavity) [2].
The aim of the reconstruction is to obtain a bowl-shaped appearance of the orbital socket, ideal for the subsequent placement of the prosthesis. The means of reconstruction are numerous. Directed healing requires several months of follow-up before obtaining the expected result [16]. There are also skin grafts, dermal fat graft, artificial dermis graft, loco-regional flaps (superficial temporal flap, temporalis muscle flap, galeal or pericranial flap), free flaps (radial forearm flap, anterolateral thigh flap, latissimus dorsi flap and microvascular scapula flap) [17].
Once the expected result has been achieved, aesthetic rehabilitation is necessary. It is mainly based on orbital prostheses, although some patients prefer to wear an eye patch. Osseointegrated prostheses constitute the gold standard today, a principle described for the first time by Branemark in 1969 [18]. Their installation takes place in 2 stages: the installation of the orbital implants in the socket then that of the pillars 3-4 months later [19]. Patients are generally satisfied with their prostheses when they are made by specialized anaplastologists. Peri-implant hygiene must be rigorous.
References
- Bartische G, Oftalmodouleiam, das ist augendienst. Dresden: Mathes Stockel, 1583: 217-219.
- Gregory M Notz, Nicholas Purdy. Indication and technique of orbital exenteration, Operating techniques in otolaryngology - Head and neck surgery, 2018; 29: 218-221.
- Zhang Z, Ho S, Yin V, et al. International multicenter review of orbital exenteration and reconstruction in oculoplastic and orbital practice. Br J Ophthalmol, 2018; 102(5): 654-658.
- Tassone P, Gill KS, Hsu D, et al. Naso- or orbito-cutaneous fistulas after free flap reconstruction of orbital exenteration defects: retrospective study, systematic review and meta-analysis. J Neurol Surg Part B Skull Base, 2017; 78(4): 337-345.
- Gill KS, Hsu D, Tassone P, et al. Postoperative cerebrospinal fluid leak after microvascular reconstruction of craniofacial defects with orbital exenteration. The laryngoscope, 2017; 127(4): 835-841.
- Aryasit O, Preechawai P, Hirunpat C, Horatanaruang O, Singha P. Factors related to survival outcomes after orbital exenteration: a retrospective and comparative case series. BMC Ophthalmol, 2018; 18(1): 186.
- Arnaud Martel, Stéphanie Baillif, Sacha Nahon-Estève, et al. Orbital exenteration: an updated review with perspectives. Ophthalmology Survey, 2021; 66: 856–876.
- Casale R, Symeonidou Z, Bartolo M. Topical treatments for localized neuropathic pain. Curr Pain Headache Rep, 2017; 21(3): 15.
- Gerring RC, Ott CT, Curry JM, Sargi ZB, Wester ST. Orbital Exenteration for Advanced Non-Melanoma Periorbital Skin Cancer: Prognostic Factors and Survival. Eye Lond Engl, 2017; 31(3): 379-388.
- Langlois B, Jacomet PV, Putterman M, Morax S, Galatoire O. Evaluation of reconstructive techniques after orbital exenteration in 56 cases. J Fr Ophthalmol, 2012; 35(9): 667-677.
- Leibovitch I, McNab A, Sullivan T, Davis G, Selva D. Orbital invasion by periocular basal cell carcinoma. Ophthalmology, 2005; 112(4): 717-723.
- Madge SN, Khine AA, Thaller VT, et al. Globe-sparing surgery for medial canthal basal cell carcinoma with anterior orbital invasion. Ophthalmology. 2010;117(11):2222-8.
- Wong KY, Fife K, Lear JT, Price RD, Durrani AJ. Vismodegib for locally advanced periocular and orbital basal cell carcinoma: A review of 15 consecutive cases. Plast Reconstr Surg Glob Open, 2017; 5(7): e1424.
- Yin VT, Merritt H, Esmaeli B. Targeting EGFR and Sonic Hedgehog pathways for locally advanced eyelid and periocular carcinomas. Global cases J Clin, 2014; 2(9): 432-438.
- Yin VT, Pfeiffer ML, Esmaeli B. Targeted therapy for orbital and periocular basal cell carcinoma and squamous cell carcinoma. Ophthal Plast Reconstruction Surg, 2013; 29(2): 87-92.
- Cooper J. Wound management after orbital exenteration surgery S4, S6, S8, passim. Br J Nursing Mark Allen Publ, 2009; 18(6).
- Langlois B, Jacomet PV, Putterman M, Morax S, Galatoire O. Evaluation of reconstructive techniques after orbital exenteration in 56 cases.
- Brånemark PI, Adell R, Breine U, Hansson BO, Lindström J, Ohlsson A. Intraosseous anchoring of dental prostheses. I. Experimental studies. Scand J Plast Reconstruction Surg, 1969; 3(2): 81-100.
- Melicher Larson JS, Nerad JA. The use of osseointegration and rare earth magnetic coupling for the retention of oculofacial prostheses in the exenterated orbit. Curr Opin Ophthalmol, 2009; 20(5): 412-416.

