Published online Jun 26, 2021. doi: 10.4330/wjc.v13.i6.155
Peer-review started: January 20, 2021
First decision: February 28, 2021
Revised: March 18, 2021
Accepted: May 17, 2021
Article in press: May 17, 2021
Published online: June 26, 2021
A challenging technical scenario frequently encountered in a percutaneous coronary intervention of a coronary bifurcation lesion (CBL) is stent implantation of only the stenosed segment without compromising the other two normal segments in non-true bifurcation lesions. Another is precise stent implantation covering the side branch ostium without leaving excessive stent metal at the other two segments of a bifurcation lesion in complex true bifurcation lesions. The aim of this study was to describe a novel stenting technique for both non-true and true CBLs by using a guide extension catheter (GuideLiner). With the assistance of a guide extension catheter mounted on both the main and the side-branch guidewires and with its intubation down to the bifurcation carina, a stent can be implanted in the side branch segment or distal main segment of the bifurcation lesion appropriately without compromising the other two segments of the coronary bifurcation. Stent implantation is described in three bifurcation lesions in three cases and shown in detail with illustrative figures. The technique facilitates side-branch only stenting in side-branch mono-ostial (medina 0, 0, 1) CBL or only the distal main segment in distal mono-ostial (medina 0, 1, 0) CBL without compromising the other two remaining segments when using the one-stent technique in non-true CBLs without leaving unnecessary excessive stent metal at the bifurcation site and when using a two-stent technique in complex true bifurcation lesions (tri-ostial or medina 1, 1, 1). Consequently, through optimizing stent deployment, the technique may have the potential to reduce the risk of subacute stent thrombosis and future in-stent restenosis. The most appropriate lesions suitable for the technique, and some other practical tips are also described.
Core Tip: A novel stenting technique for coronary bifurcation lesions (CBLs) is presented. With the help of a guide extension-assisted technique using a GuideLiner mounted on both guidewires in the branches of the bifurcation lesion and advanced to the carina of the bifurcation, a stent can be implanted at the most possible appropriate site of the side branch in side-branch mono-ostial (medina 0, 0, 1) or in the distal mono-ostial (medina 0, 1, 0) in non-true CBLs. The technique can also be used to stent the side branch in two-stent techniques for complex true CBLs (tri-ostial or medina 1, 1, 1).
- Citation: Y-Hassan S, de Palma R. A Novel guide extension assisted stenting technique for coronary bifurcation lesions. World J Cardiol 2021; 13(6): 155-162
- URL: https://www.wjgnet.com/1949-8462/full/v13/i6/155.htm
- DOI: https://dx.doi.org/10.4330/wjc.v13.i6.155
Percutaneous coronary intervention (PCI) of a coronary bifurcation lesion (CBL) is a challenging procedure for interventionists[1]. The short- and long-term outcomes are closely related to the procedural success and optimization of the bifurcation stenting technique[2,3]. Several one- or two-stent techniques for PCI of CBLs have been described, depending on the type and location of the bifurcation lesions[1,4]. Stenting of the side branch in side-branch mono-ostial[5] (medina 0, 0, 1)[6] bifurcation stenoses is associated with difficulties in stent placement at the proper site with the risk of missing the side branch ostium or of excessive stent protrusion in the main branch. The same applies to stenting only the distal main segment in distal mono-ostial (medina 0, 1, 0) bifurcation stenoses. Consequently, the provisional stenting technique is typically employed in treating a distal mono-ostial stenosis (medina 0, 1, 0) but this requires “unnecessary” stenting of the normal proximal main segment of the bifur
The provisional stenting technique is also recommended as the default strategy by most interventionists in tri-ostial (medina 1, 1, 1) or true bifurcation lesions[1]. However, this technique may lead to side-branch occlusion during stenting of the main branch and acute peri-procedural myocardial infarction. Improvements in the protection of the side branch have been reported with the jailed balloon protection of the side branch[7] or modified jailed balloon techniques[8]. The risk of side-branch occlusion is increased in complex tri-ostial (medina 1, 1, 1) bifurcation lesions where a two-stent technique should always be considered. However, the current two-stent techniques for the CBLs, such as crush[9] and culotte[10] stenting, leave multiple layers of stent struts at the bifurcation site causing difficulties in rewiring, balloon re-crossing, and the performance of sequential post-dilatation and final kissing balloon inflation. This may result in stent under expansion, and/or malapposition at the bifurcation site predisposing to acute and sub-acute stent thrombosis. Suboptimal stent implantation is also associated with an increased risk of future in-stent restenosis[1]. To overcome these challenges, the crush technique has evolved to mini-crush and double kissing (DK)-crush techniques[1]. The DK-crush stenting technique facilitates final kissing balloon inflation, but the technique has complex procedural steps and is time consuming. Other two-stent techniques include simultaneous kissing stenting, T-stenting and V-stenting techniques. The T-stenting technique does not leave multiple layers of stent struts, which facilitates final kissing balloon inflation, but has the potential of geographical miss at the side branch. These technical shortcomings highlight the need for a stent implantation technique that avoids unnecessary stenting of the normal segments and not leaving multiple layers of stent struts at the bifur
The GuideLiner is a guide extension catheter that is mounted coaxially on a monorail system extending through the guide catheter. It consists of a coaxial exchange system with a flexible extension of 20 cm and a radio-opaque marker 2 mm proximal to the tip of the catheter. The extension catheter has been used for deep vessel intubation to allow the smooth device delivery of balloons and stent platforms in calcified or tortuous vessel anatomy. Guide extension catheters have also been used to facilitate obtaining good angiographic and optical coherence tomographic (OCT) images by subselective injection of reduced contrast medium, and particularly useful in tortuous vessel or angulated bifurcation anatomy[11]. Further uses include stenting the main branch of a complex bifurcation lesion while retaining guide wires in both side branches of the bifurcation[12] and to facilitate side strut stenting technique for the treatment of right coronary artery ostial in-stent restenosis where there is ostial right coronary artery stent overhang into the aortic root[13].
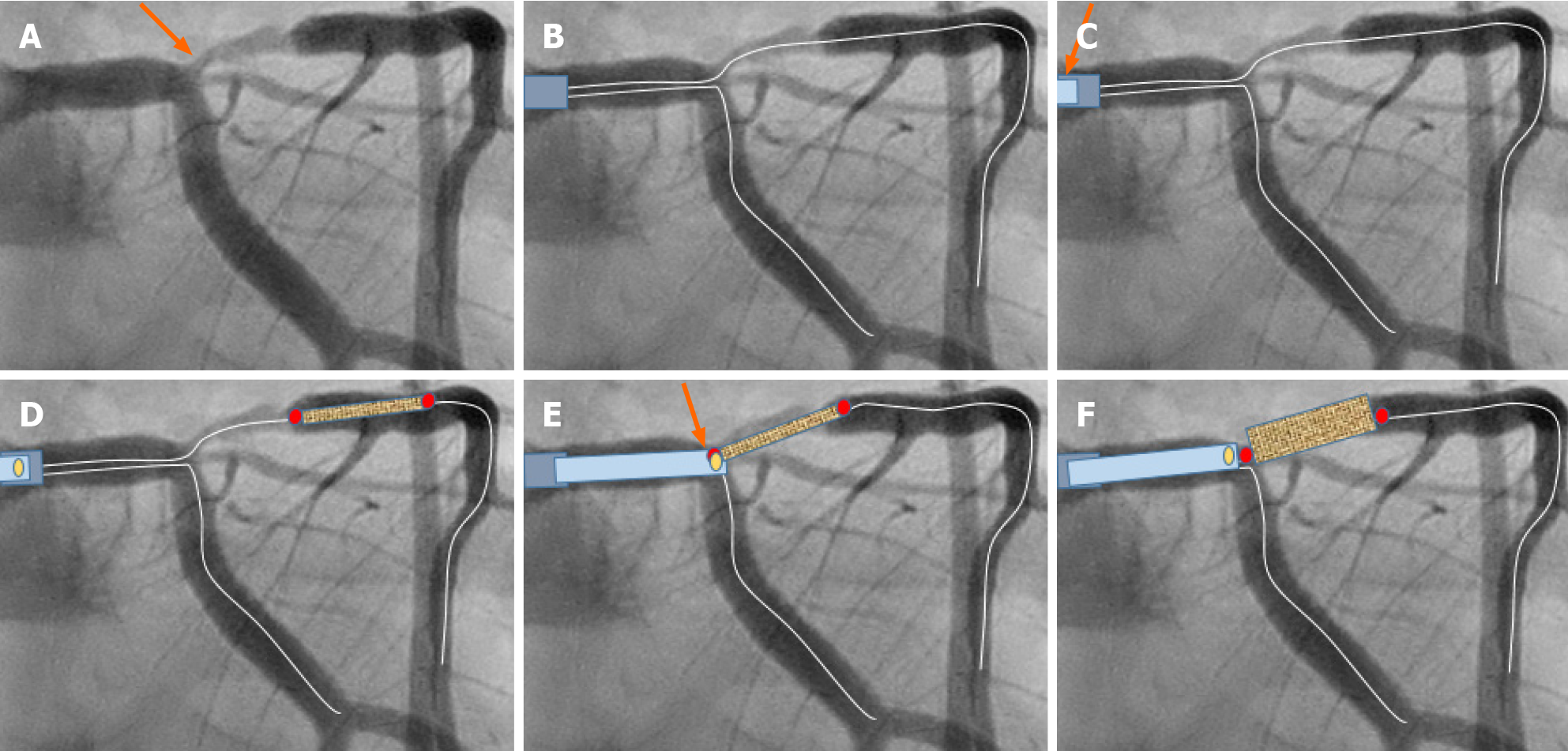
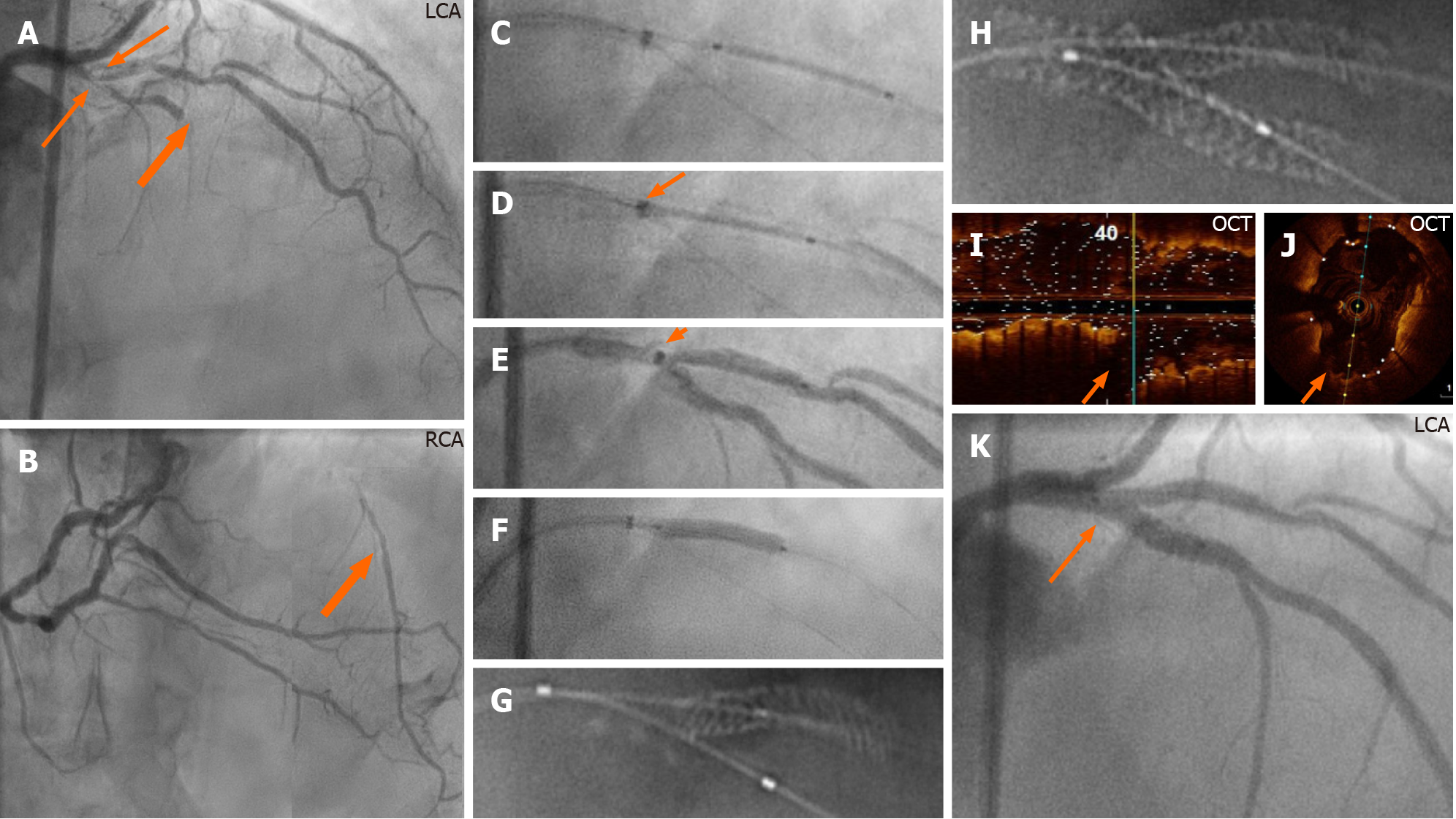
In this novel technique, the coronary artery is engaged by conventional 6, 7, or 8F guide catheters, through radial (6 and 7F), or femoral (6, 7, and 8F) artery approaches. Two guidewires are placed in the branches of the bifurcation lesion, one in the main branch and one in the side branch (Figure 1A and B). The bifurcation lesion is pre-dilated, preferably with undersized 1.5 or 2 mm balloon, and the ostium of the side branch should be dilated with a cutting or scoring balloon, especially the left anterior descending artery (LAD) ostium or the left circumflex artery (LCx) ostium. The dilated but still stenosed bifurcation lesion helps to prevent to-and-fro movement of the stent during stent implantation especially in LAD. Dilatation of the ostium by a cutting or scoring balloon helps to avoid stent sliding distally during stent implantation. Thereafter, the appropriate (6, 7, or 8F) GuideLiner mounted on both guidewires is introduced and placed near the tip of the guide catheter (Figure 1C). The stent is introduced somewhat distal to the lesion (Figure 1D) and then the GuideLiner introduced to the carina of the bifurcation, and the stent is retracted while the GuideLiner is advanced carefully against the carina until the proximal radio-opaque marker of the stent balloon is overlapping the distal radio-opaque marker of the GuideLiner (Figure 1E). Being mounted on both main and side-branch guidewires, the guide extension catheter will stop at the carina of the bifurcation just adjacent to the ostium of the side branch or ostium of the distal main segment of the main branch. The stent is then implanted slowly to avoid stent displacement (Figure 1F). During stent implantation, the proximal part of the stent balloon pushes the GuideLiner catheter backward. In this way the stent is implanted at the ostial region and distally without compromising the other two segments of the bifurcation (Figures 1-4). The stent balloon catheter is pulled out first followed by the GuideLiner. The stent is then post-dilated, and the stent apposition is checked in the conventional way. In tri-ostial bifurcation lesions (medina 1, 1, 1), and after stenting the side branch by GuideLiner technique described above (Figure 4), the procedure is completed conventionally with stenting of the main branch, proximal optimization technique (POT), rewiring of the side branch, balloon re-crossing of the main branch stent struts, sequential balloon dilatation, and final kissing balloon inflation. The technique is further illustrated and described in three bifurcation cases treated with this guide extension technique in Figures 1-4.
This novel guide extension assisted stenting technique is characterized by keeping the guidewire access to both branches of the bifurcation during the whole procedure in side-branch mono-ostial (medina 0, 0, 1), distal mono-ostial (medina 0, 1, 0) CBL, and stenting only the lesion site without compromising the other two segments of the bifurcation. The most appropriate bifurcation sites suitable are the bifurcation lesions situated proximally in the coronary artery trees as left main stem/LAD/LCx, proximal LAD/diagonal, and proximal LCx/marginal bifurcation lesions. The most suitable types of CBLs for this technique are the side-branch mono-ostial (medina 0, 0, 1), the distal mono-ostial (medina 0, 1, 0) and potentially distal bi-ostial (medina 0, 1, 1) bifurcation lesions when the proximal segment of the main branch is normal. The technique can also be utilized in tri-ostial bifurcation stenosis (medina 1, 1, 1) through stenting the side branch using the guide extension technique (Figure 4) and then conventional stent implantation in the main branch with the advantage of not leaving excessive stent metal at the carina and facilitation of the procedure by proximal optimization, rewiring, sequential balloon dilatation, and final kissing balloon inflation.
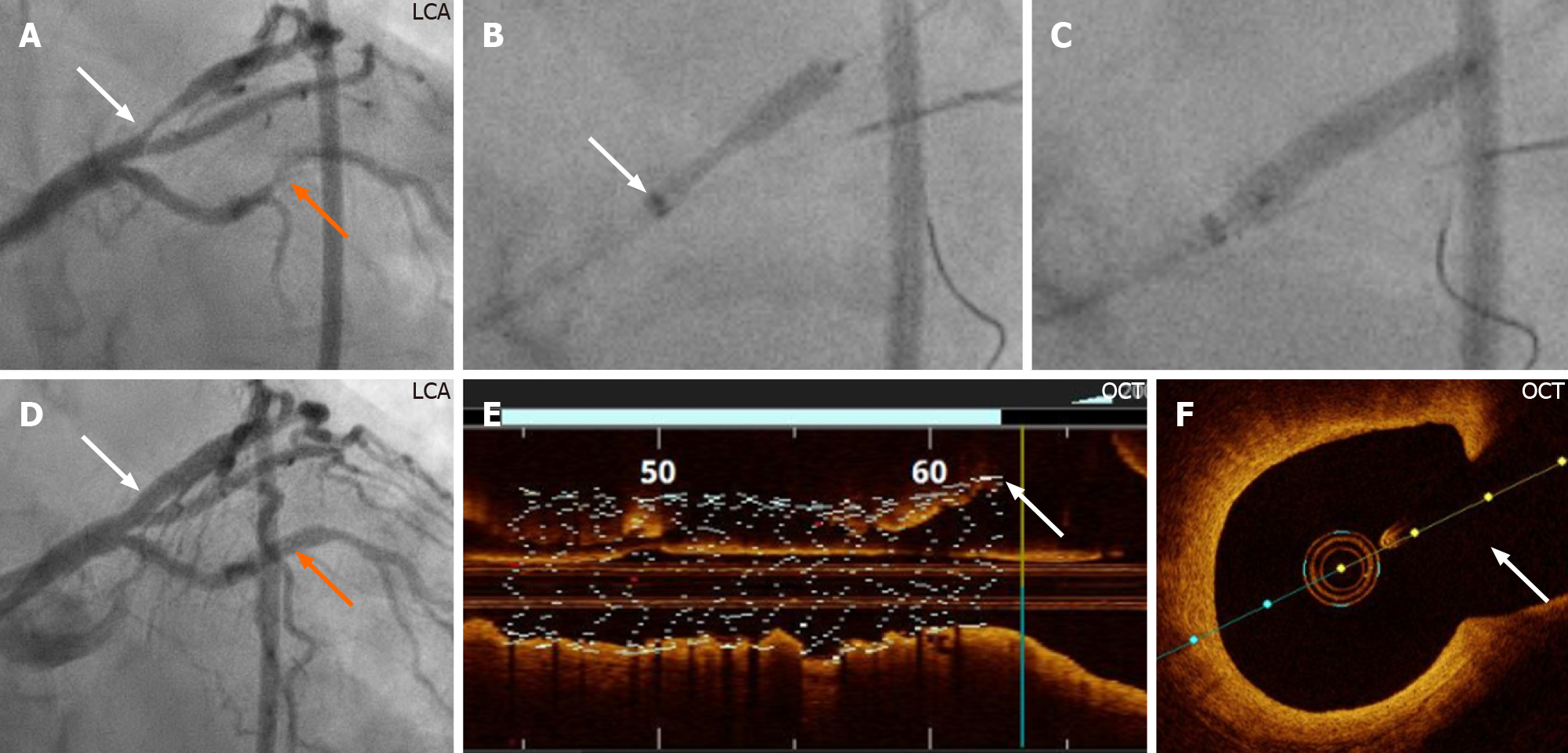
Side branch stenting is challenging for all interventionists. The crucial step is positioning the stent so that it covers the ostium of the side branch without protruding too much into the main branch. Achievement of geographical precision is more difficult when the bifurcation angle is of the “Y-type” and almost impossible when the ostium of the side branch cannot be visualized, which is the case in some bifurcation lesions as shown in Figure 3. One of the disadvantages of the T-stenting technique is that it may miss covering the ostium of the side branch. In contrast, the crush, mini-crush, and culotte stenting techniques[1] leave multiple strut layers in the main branch that may result major difficulty in rewiring the side branch and subsequent sequential and final kissing balloon inflations. The novel guide extension-assisted stenting technique of the side branch reduces the risk of missing the ostium substantially and avoids unnecessary stent protrusion into the main branch.
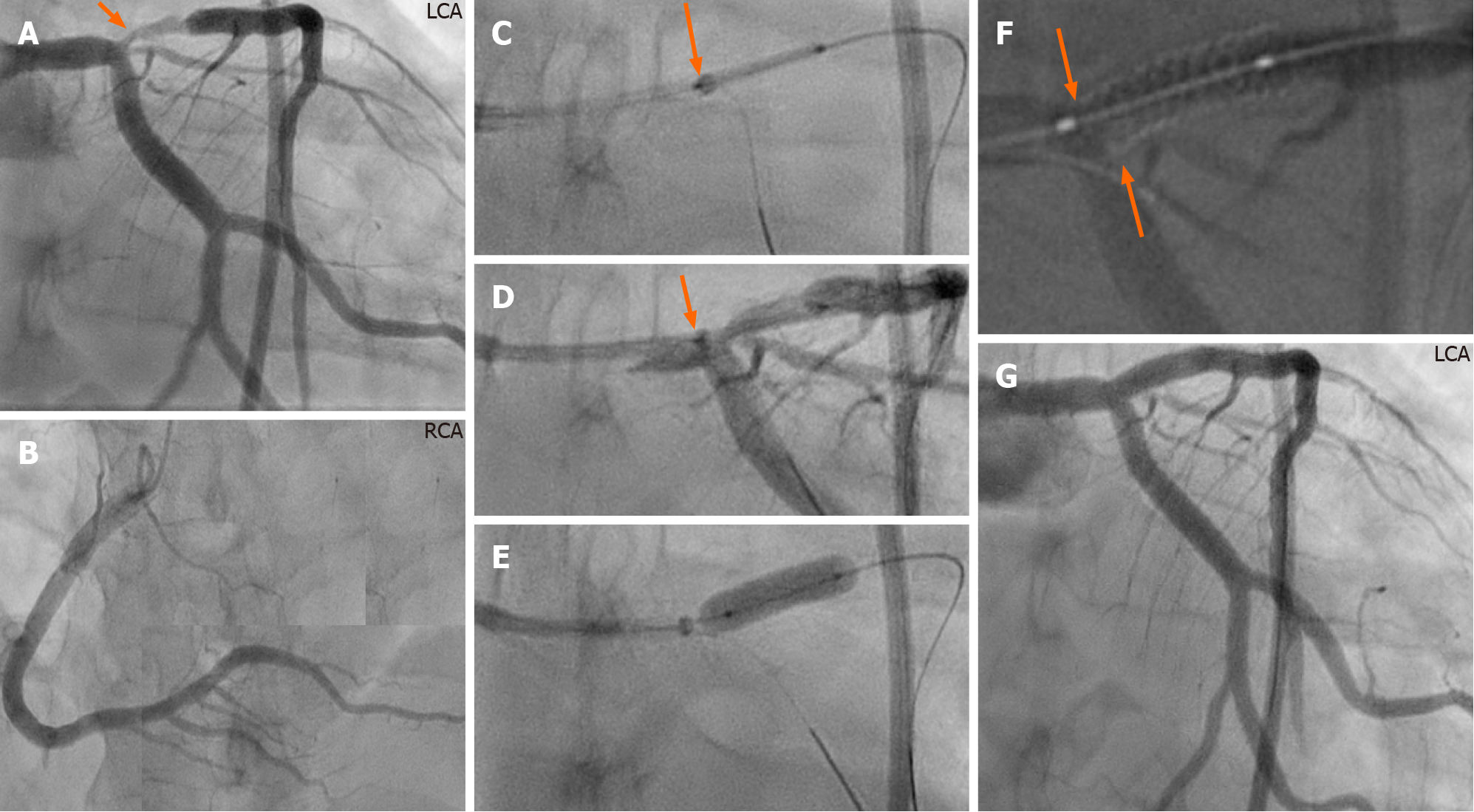
Three different types of CBLs in three cases that were successfully treated with PCI using a GuideLiner-assisted stenting technique. Two cases had non-true CBLs and one had a true CBL. The first case had left main stem/LCx/LAD bifurcation stenosis of a side-branch type mono-ostial (medina 0, 0, 1) bifurcation lesion. With a GuideLiner advanced to the carina of the bifurcation, the side branch (LAD) was stented successfully (Figure 2). The stent covered the ostium of the LAD without leaving stent struts in the left main stem or LCx, confirmed by StentBoost imaging (Figure 2F). The bifurcation lesion in the second case treated with this novel technique was a LAD/ diagonal bifurcation stenosis type distal mono-ostial (medina 0, 1, 0) where the stenosis was restricted to the distal main segment of the bifurcation. It is worth mentioning that visualization of the angle between the diagonal branch and the distal segment of the main branch (LAD) was ambiguous, making it especially suitable for this novel technique. With a GuideLiner intubated down to the carina of the bifur
The main advantage of the guide extension-assisted stenting technique is precise positioning of the stent at the side branch of a CBL especially in lesions where the side-branch ostium is challenging to visualize or ambiguous. The most appropriate CBLs suitable for this technique are the side-branch mono-ostial (medina 0, 0, 1), distal mono-ostial (medina 0, 1, 0), and potentially distal bi-ostial (medina 0, 1, 1) CBLs. In such lesions, the guide extension-assisted technique avoids stenting of the normal proximal segment of the bifurcation with its subsequent risk of compromising the other branch of the bifurcation, and the subsequent need for re-crossing the stent struts for final kissing balloon inflation. The guide extension assisted technique can also be utilized for stenting the side-branch lesion in complex tri-ostial (medina 1, 1, 1) bifurcation lesions as demonstrated Figure 4.
The bifurcation PCI principle of “keep it open” for the side branch and the provisional side-branch stenting, is currently regarded as the default procedure in the majority of bifurcation lesions, in part attributable to the fact that the two-stent techniques (crush and culotte) are more complex and may leave stent struts under expanded or malapposed, with increased risk of acute or subacute stent thrombosis and future in-stent-restenosis. However, in complex bifurcation lesions, the risk of compromising the side branch is substantial with a provisional approach. The incidence of side-branch occlusion was 13.4% for true bifurcation and 4.0% for non-true bifurcation lesions in a bifurcation stenting registry enrolling 2227 cases of bifurcation PCIs treated by the one-stent approach[14]. For this reason, a two-stent technique is frequently necessary for complex true bifurcation lesions. The DK-crush technique has been shown to be superior to the provisional side-branch stenting as well as to culotte techniques in terms of efficacy and safety[1,3]. Nonetheless, it must be recognized that the DK-crush technique is technically demanding and time consuming.
A simplified two-stent technique, which does not leave excess layers of stent struts at the bifurcation site, is thus highly desirable. The guide extension-assisted stenting technique for the side branch does not leave unnecessary stent metal in the main branch as may occur with crush and culotte techniques and consequently avoids the subsequent risks of subacute stent thrombosis and difficulties in performing rewiring, balloon re-crossing the stent strut toward the side branch, sequential balloon dila
The main limitation of the technique is that in Y-shaped side branch angulation, it is impossible to implant a stent covering the whole side-branch ostium circumferentially; in such cases the stent either protrudes somewhat into the main branch at the lower edge of the side-branch ostium or misses somewhat the upper edge of the side-branch ostium. Care must also be taken to ensure that the proximal stent balloon marker is not proximal to the guide extension radio-opaque marker during stent implantation to avoid inadvertent “trapping” of the guide extension.
In addition, the use of guide extensions is associated with complications such as proximal dissection due to deep intubation, air embolism due to insufficient de-airing, and ischemia, which may limit the length of time that the equipment can be kept in place.
Finally, other guide extension catheters are currently available, including Guidezilla (Boston Scientific), Telescope (Medtronic), and Gudion (IMDS). The technique should be applicable to these platforms even though they were not tested in this reported experience.
A novel guide extension-assisted stenting technique for selected CBLs is described. This technique facilitates stenting only the diseased side branch or distal main segment in non-true bifurcation lesions without compromising the other branches. It may also facilitate precise stenting implantation in the side branch when using two-stent techniques in complex true bifurcation stenoses without leaving excess stent struts at the bifurcation site, which facilitates easier rewiring, balloon re-crossing, and performing final kissing balloon inflation. The technique may potentially reduce the risks of acute and subacute stent thrombosis as well as future in-stent restenosis and is worthy of further investigation.
Manuscript source: Invited manuscript
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: Sweden
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Lim PO, Sato A S-Editor: Fan JR L-Editor: Filipodia P-Editor: Yuan YY
| 1. | Collet C, Mizukami T, Grundeken MJ. Contemporary techniques in percutaneous coronary intervention for bifurcation lesions. Expert Rev Cardiovasc Ther. 2018;16:725-734. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 2. | Huang F, Luo ZC. Cardiovascular outcomes associated with crush vs provisional stenting techniques for bifurcation lesions: a systematic review and meta-analysis. BMC Cardiovasc Disord. 2019;19:93. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | Chen E, Cai W, Chen LL. Crush vs Culotte stenting techniques for coronary bifurcation lesions: A systematic review and meta-analysis of clinical trials with long-term follow-up. Medicine (Baltimore). 2019;98:e14865. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 4. | Y-Hassan S, Lindroos MC, Sylvén C. A novel stenting technique for coronary artery bifurcation stenosis. Catheter Cardiovasc Interv. 2009;73:903-909. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Y-Hassan S, Lindroos MC, Sylvén C. A Novel Descriptive, Intelligible and Ordered (DINO) classification of coronary bifurcation lesions. Review of current classifications. Circ J. 2011;75:299-305. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | Medina A, Suárez de Lezo J, Pan M. [A new classification of coronary bifurcation lesions]. Rev Esp Cardiol. 2006;59:183. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 500] [Cited by in F6Publishing: 470] [Article Influence: 26.1] [Reference Citation Analysis (0)] |
| 7. | Burzotta F, Trani C, Sianos G. Jailed balloon protection: a new technique to avoid acute side-branch occlusion during provisional stenting of bifurcated lesions. Bench test report and first clinical experience. EuroIntervention. 2010;5:809-813. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 49] [Cited by in F6Publishing: 51] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 8. | Shishido K, Moriyama N, Hayashi T, Yokota S, Miyashita H, Mashimo Y, Yokoyama H, Nishimoto T, Ochiai T, Tobita K, Yamanaka F, Mizuno S, Tanaka Y, Murakami M, Takahashi S, Saito S. The efficacy of modified jailed balloon technique for true bifurcation lesions. Catheter Cardiovasc Interv. 2020;96:20-28. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 9. | Colombo A, Stankovic G, Orlic D, Corvaja N, Liistro F, Airoldi F, Chieffo A, Spanos V, Montorfano M, Di Mario C. Modified T-stenting technique with crushing for bifurcation lesions: immediate results and 30-day outcome. Catheter Cardiovasc Interv. 2003;60:145-151. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 211] [Cited by in F6Publishing: 216] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 10. | Chevalier B, Glatt B, Royer T, Guyon P. Placement of coronary stents in bifurcation lesions by the "culotte" technique. Am J Cardiol. 1998;82:943-949. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 181] [Cited by in F6Publishing: 183] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 11. | Mitomo S, Naganuma T, Nakamura S, Tahara S, Ishiguro H. Potential advantages of the GuideLiner® catheter: insights from optical coherence tomography. Cardiovasc Interv Ther. 2017;32:56-61. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 12. | Warisawa T, Naganuma T, Nakamura S. Off-label use of 7Fr GuideLiner in the bifurcation coronary intervention protecting 2 side branches. Cardiovasc Interv Ther. 2017;32:392-395. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Kassimis G, Raina T. GuideLiner extension catheter-facilitated side strut stenting technique for the treatment of right coronary artery ostial in-stent restenosis. Cardiovasc Revasc Med. 2018;19:133-136. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Hahn JY, Chun WJ, Kim JH, Song YB, Oh JH, Koo BK, Rha SW, Yu CW, Park JS, Jeong JO, Choi SH, Choi JH, Jeong MH, Yoon JH, Jang Y, Tahk SJ, Kim HS, Gwon HC. Predictors and outcomes of side branch occlusion after main vessel stenting in coronary bifurcation lesions: results from the COBIS II Registry (COronary BIfurcation Stenting). J Am Coll Cardiol. 2013;62:1654-1659. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 164] [Cited by in F6Publishing: 126] [Article Influence: 11.5] [Reference Citation Analysis (0)] |