CASE SUMMARY
BACKGROUND: A 63-year-old man was referred for cardiac catheterisation for typical angina. At angiography, high-grade stenosis of the first diagonal branch, of the proximal circumflex and of an intermediate branch was found. After treatment of the diagonal branch, fractional flow reserve of the circumflex and intermediate branch was negative, but symptoms persisted.
INVESTIGATION: Physical examination, laboratory test, stress echocardiography, fractional flow reserve, coronary flow reserve.
DIAGNOSIS: Complex interaction between epicardial stenosis and microvascular hyporeactivity.
MANAGEMENT: Stenting.
KEYWORDS: coronary angiogram, fractional flow reserve, refractory angina pectoris
PRESENTATION OF THE CASE
A 63-year-old man underwent elective coronary angiography for dyspnoea (NYHA Class III) and typical angina (CCS Class III). His medical history included embolic central retinal occlusion 10 years before and thromboendarterectomy of the right internal carotid artery in 2008. He had arterial hypertension and received therapy with metoprolol, aspirin and candesartan.
Coronary angiography (Figure 1, Moving image 1) revealed a subocclusive stenosis of a diagonal branch, non-relevant atherosclerosis (<20% at angiography) of the left anterior descending coronary and the right coronary artery, and 75% stenosis involving a marginal branch as well as the ostium of the circumflex (as assessed by quantitative coronary angiography). After administration of 5000 IU heparin, an XB 3.5 guiding catheter was placed at the ostium of the left coronary. The patient reported angina after a BMW intracoronary wire was placed in the periphery of the diagonal branch. A XIENCE PRIME™ drug-eluting stent (2.5×23 mm; Abbott Laboratories, Abbott Park, IL, USA) was successfully implanted with resolution of the symptoms.

Figure 1. The first angiography showed a 90% stenosis of a diagonal branch and a 75% stenosis of the proximal circumflex and first marginal branch.
In order to assess the haemodynamic relevance of the stenosis of the circumflex, fractional flow reserve (FFR) measurements of both the circumflex and the marginal branch were performed. A PressureWire™ Certus (St. Jude Medical, St. Paul, MN, USA) was advanced 6-7 cm to the periphery of the circumflex coronary followed by an intracoronary nitroglycerine (200 µg) injection. The mean transit time (Tmn, an expression of coronary resistances1) was measured as the average of three separate rapid injections of 3 ml saline through the coronary catheter (Figure 2). At rest, Pd (mean blood pressure distal to the stenosis) was 87 mmHg, Pa (mean aortic pressure) was 90 mmHg, and the Tmn was 1.07. After that, hyperaemia was induced by intravenous administration of adenosine through a repeatedly flushed 4 Fr sheath placed in the vena femoralis. The infusion was kept at 140 µg/kg/min. Sixty seconds into the adenosine infusion the patient complained of “typical” adenosine-induced symptoms. While the systolic blood pressure decreased to 78 mmHg, hyperaemic Tmn and the ratio of distal to proximal blood pressure (fractional flow reserve, FFR) were assessed: FFR was 0.98, Tmn during hyperaemia 1.48, and the coronary flow reserve (CFR, calculated by dividing the resting Tmn by the Tmn measured during adenosine infusion) was 0.7 (=0.8 after exclusion of one outlier). The index of microvascular resistances (IMR, the product of intracoronary pressure and Tmn during adenosine infusion) was 139, suggesting impaired microvascular reactivity.
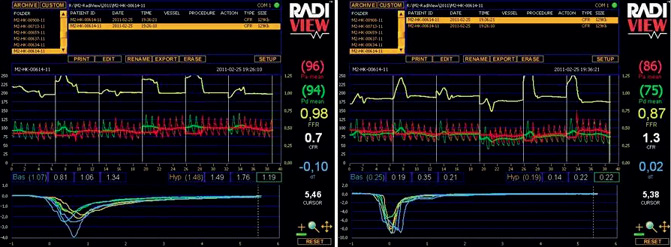
Figure 2. The results of FFR and CFR measurements in the circumflex (A) and marginal branch (B). The low Tmn in the second assessment (marginal branch) could be explained by the fact that, due to the small vessel size, the wire was not advanced deep into the vessel.
The same measurements were performed after placing the wire proximal in the marginal branch and during infusion of adenosine at a rate of 170 µg/kg/min. In this case, FFR was 0.92 and CFR was 1.3.
In conclusion, FFR suggested that the stenosis in the marginal branch and the circumflex coronary was haemodynamically non-significant. The patient was discharged.
One month later, the patient underwent a control visit, where he reported the persistence of the symptoms (dyspnoea NYHA Class II, angina CCS Class III). Due to chronic knee pain, the patient could not undergo an exercise stress test and it was decided to repeat coronary angiography. At angiography, the stent in the diagonal branch was patent. There was no change in the angiographic appearance of the (angiographically relevant) stenosis at the ostium of the circumflex and marginal branch, and no new stenosis was found. The patient was prescribed organic nitrates (80 mg pentaerythrityltetranitrate t.i.d.) and discharged, but typical symptoms persisted despite therapy for the following four months.
FFR has become the gold standard for the assessment of coronary artery disease. CFR has several limitations, including a dependence on baseline blood flow, relatively lower repeatability, and technical limitations (in this patient the first CFR was <1, probably due to two outlier values, and the Tmn in the second assessment was low at baseline, probably due to the fact that the wire could not be safely pushed far enough in the relatively small periphery of the marginal branch). In this case, however, a blunted CFR fitted well with the angiographic appearance of the stenosis and with the symptoms of the patient. What is the diagnosis, and how should the patient be treated?
How would I treat?
THE INVITED EXPERT’S OPINION
Dr Jabs and colleagues provide a very interesting case highlighting the discrepancy between clinical features and physiologic indices. As physiologic assessment has become more popular in real-world practice, many physicians face similar dilemmas.
The patient seems to have diffuse intermediate stenosis at the proximal left anterior descending coronary artery (LAD), critical stenosis at a relatively small diagonal branch, intermediate stenosis at the left circumflex artery (LCX) and diffuse stenosis at the obtuse marginal branch (OM). It is well known that the mismatch and reverse mismatch between coronary anatomy and functional significance frequently occur in intermediate stenoses, especially in ostial lesions2,3. Since the patient complained of severe symptoms at the time of the index procedure, it would be imperative to identify the culprit lesion causing the symptoms. Thus, I would have measured fractional flow reserve (FFR) in LAD, LCX and OM before stenting the diagonal branch. It is not common that such a diagonal branch causes severe symptoms, especially when OM supplies most of the lateral wall4.
As for the physiologic assessment, high FFR, low coronary flow reserve (CFR) and high index of microcirculatory resistance (IMR) imply the presence of microvascular dysfunction and the possibility of underestimation of epicardial stenosis severity by FFR. However, some caution may be needed in interpreting the results in this patient. In the left panel of Figure 2, systemic blood pressure during hyperaemia is higher than resting blood pressure, and in the right panel the fluctuation of a distal coronary pressure and FFR is observed during three injections of saline. These findings suggest the possibility of submaximal hyperaemia. It is also unusual that hyperaemic mean transit time (Tmn) is longer than baseline Tmn and CFR is lower than 1.0. Furthermore, although the regional difference in microvascular function can exist, it is difficult to understand the huge difference of IMR between LCX and OM (139 vs. 14). Low CFR of OM seems to be mainly due to low baseline Tmn rather than high hyperaemic Tmn. Therefore, with the results provided, it would be difficult to determine whether or not the patient had microvascular dysfunction. As there was diffuse calcified disease in the proximal LAD and LAD flow was a little slower than the other coronary arteries, FFR and IMR of LAD would have been helpful.
Finally, the patient’s sensitivity to pain may also need to be considered when interpreting this patient’s clinical and physiologic features. The patient complained of chest pain after the placement of an intracoronary guidewire, something which is not that frequent in my experience.
So, how would I assess and treat this patient? I would have measured FFR in LAD, LCX and OM during the index procedure. If all FFRs were high, I would have re-measured FFR with different methods of hyperaemia such as intracoronary bolus administration of adenosine or nicorandil5 followed by IMR measurement when FFR was still high. In case of high IMR, medical treatment for microvascular angina would have been maintained and, if not, the possibility of exercise-induced spasm would have been considered. If the patient’s symptoms do not respond to the medical treatment at all, then I would try to find objective evidence of myocardial ischaemia due to epicardial artery stenosis using other non-invasive tests such as cardiac PET scan6, as the revascularisation of the LCX lesion will require complex intervention.
The use of invasive physiologic indices has been increasing rapidly in recent years as several studies have proved the efficacy and cost benefit of a FFR-guided revascularisation strategy. However, to be adequately guided, physicians need to understand well the coronary physiology and the possible pitfalls of these invasive measurements. The numbers derived from physiologic assessment are not the “miracle cure-all” and should be interpreted as one of the guides which lead us to the adequate evaluation and management of patients with coronary artery disease.
Conflict of interest statement
B. K. Koo receives honoraria for lectures and research grants from St. Jude Medical.
How would I treat?
THE INVITED EXPERTS’ OPINION
Jabs and colleagues present a very interesting case of a patient in whom the optimal coronary revascularisation strategy remains debatable despite invasive physiological assessment of an angiographically intermediate coronary stenosis. The authors are to be congratulated for such comprehensive physiological evaluation, as the limitations of pure anatomical assessment with angiography are well recognised.
The challenging aspect of this case is the conflicting information given by the pressure-only and flow-based indices used to interrogate the lesions. Whilst the results of FFR (0.98 and 0.92) indicate physiologically non-significant stenoses, the low values of CFR (around 1, considering a degree of measurement error) clearly demonstrate the inability of the coronary circulation to augment flow in response to adenosine. From the perspective of lesion classification (significant versus non-significant) this is an example of disconcordance between FFR and CFR, which has been demonstrated to occur in approximately 30% of cases7,8.
However, from the physiological perspective such cases should not be considered a disagreement. The pressure drop across a coronary stenosis is dependent on the trans-stenotic flow rate which, during FFR measurement, is driven by the microcirculatory response to adenosine. Therefore, although high FFR values represent, on average, non-significant lesions, low trans-stenotic flow during hyperaemia caused by diseased microcirculation can lead to misleadingly high FFR results. Conversely, following the same principle, an exaggerated response of the microcirculation to adenosine may occasionally cause non-flow-limiting stenoses to have low FFR values, simply because of unusually high hyperaemic flow rates and not because they are truly obstructive9. Patients in whom invasive physiological assessment is conflicting represent a challenge to the interventionalist, who is usually faced with a dichotomous decision regarding revascularisation of such stenoses. In such cases, additional information can be used to help establish the severity of the interrogated lesion. Firstly, information about the resistance imposed by the epicardial stenosis using the hyperaemic stenosis resistance (HSR) index can be useful to differentiate epicardial from distal disease. As HSR incorporates both pressure and flow in the same index, it has been shown to be superior to FFR and CFR in identifying ischaemia when compared to reference perfusion modalities10. Secondly, the haemodynamics of a reference vessel, without focal epicardial disease, can provide useful information. Although the degree of microvascular disease can vary across coronary territories, low values of CFR in a reference vessel would be highly suggestive of the presence of diffuse microvascular disease. Finally, non-invasive perfusion modalities can contribute in such cases as additional pieces to an unresolved puzzle: it must be remembered that FFR and CFR, like any other diagnostic test in medicine, are not infallible, and the idea of using a strict and purely dichotomous interpretation of their results should be avoided.
Additionally, in this particular case, a simple observation of the baseline and hyperaemic pressure tracings provide useful information. The almost complete absence of a visible gradient in the mid-diastolic window both at baseline and hyperaemia strongly suggests that the stenosis imposes no significant limitation to coronary flow. This period within the cardiac cycle is particularly useful for haemodynamic assessment of a stenosis11 because of its intrinsic high flow rate and low resistance.
Finally, although less likely, other possible explanations for the author’s findings are: 1) the recruitment of collaterals creating a steal phenomenon, or 2) paradoxical vasoconstriction of the microcirculation, caused by an accentuated reduction in coronary perfusion pressure during adenosine administration. This latter phenomenon happens because, when mean coronary perfusion pressure reaches approximately 60 mmHg, coronary flow is significantly reduced, and the distal coronary circulation may vasoconstrict in a last effort to maintain perfusion pressure12. Therefore, in such circumstances, FFR values are considered uninterpretable, and efforts should be made to restore blood pressure before FFR measurement is performed13.
In summary, in this particular case, the very high values of FFR and very abnormal values of CFR and IMR make the diagnosis of distal microvascular disease much more likely, leaving the focal epicardial disease as a less important contributor to the patient’s symptoms. Until clinical trials evaluate the best strategy for these patients in a prospective, randomised manner, it appears reasonable to treat them medically and that is indeed what we would recommend as a first approach14. We believe that placing a stent in such lesions should be a matter of individualised clinical judgement, reserved to situations where maximal anti-angina therapy fails to control symptoms15.
Conflict of interest statement
The authors have no conflicts of interest to declare.
How did I treat?
ACTUAL TREATMENT AND MANAGEMENT OF THE CASE
Given the persistence of symptoms, it was decided to perform a dobutamine stress echocardiography which showed normokinesia at rest and a new hypokinesia of the posterolateral wall at 40 µg/kg/min dobutamine +0.5 mg atropine. Based on this evidence of ischaemia in the territory downstream to the stenosis in a symptomatic patient, percutaneous intervention was scheduled. An XB 3.5 guiding catheter was placed at the ostium of the left main coronary, and two BMW wires were advanced in the periphery of the circumflex and first marginal branch. A 3.0×12 mm XIENCE PRIME™ stent (Abbott) was then implanted in the proximal circumflex overlapping the ostium of the marginal branch; after exchange of the guidewires and predilatation with a 2.0×9 mm Maverick® balloon catheter (Boston Scientific, Natick, MA, USA), a second 2.75×15 mm XIENCE stent was placed in the marginal branch (T stenting). A final kissing PTCA was performed with two (2.5×9 mm and 2.0×9 mm) Maverick® balloons. A good final angiographic result was achieved. Six months after the intervention, the patient described an immediate and sustained improvement of symptoms. His reported exercise tolerance had also increased significantly (CCS angina 0-I, dyspnoea NYHA Class 0-I).
We present the case of a patient with a high-grade stenosis at angiography, typical symptoms, and negative FFR. Based on FFR alone, this patient would normally be classified as having microvascular angina or non-cardiac chest pain. Since CFR and IMR are usually not assessed, the validity of the FFR results would not have been questioned in normal practice. In our case, however, CFR and IMR assessments gave evidence of a reduced hyperaemia during FFR assessment. Stress echocardiography confirmed the presence of an exercise-induced regional contractile dysfunction in the territory downstream of the stenosis.
FFR expresses the ratio of maximum myocardial blood flow in the presence of a stenosis divided by the theoretical maximum flow in the absence of the stenosis, thus providing an index of how much maximal blood flow is limited by the stenosis. While the introduction of FFR in clinical practice led to an invaluable improvement in diagnostic capacities, and the systematic use of this technique is both clinically sound and cost-saving, a number of exceptions need to be acknowledged. For instance, the interpretation of FFR data requires particular care in ostial lesions, myocardial bridges, and in the presence of congestive heart failure. Similarly, since the measurement of FFR requires the induction of maximal hyperaemia, the presence of microvascular dysfunction/hyporeactivity can sometimes complicate the application of this method. In patients with microvascular angina and intermediate stenoses, FFR still expresses the epicardial component of ischaemia, providing information on how much the removal of the epicardial stenosis can contribute to the removal of ischaemia. This concept is, however, based on two assumptions that remain undemonstrated:
1. that microvascular dysfunction is reproducible and constant over time, and
2. that the responses to adenosine entirely and invariably reflect the responses to more complex stimuli (ischaemia and exercise).
Regarding point 1, a number of studies and clinical experience demonstrate that, due to a significant regional variation and time variability, the distribution of both resting and hyperaemic flow, and therefore microvascular dysfunction, is very heterogeneous in the population16 and over time17. It cannot a priori be excluded that a blunted microvascular responsiveness (determining in this case a normal FFR) might be a transient phenomenon, as suggested in this case by the fact that the dobutamine test was positive at a distance of time. Regarding point 2, it is well accepted that exercise-induced hyperaemia results from several distinct pathways, including adenosine, ATP-sensitive K+ channels, and nitric oxide-mediated mechanisms; the blunting in one of these pathways might therefore not necessarily reflect “overall” dysfunction.
Taken alone, CFR does not provide a reliable haemodynamic assessment of epicardial stenoses. However, while not adding procedural complications, CFR/IMR assessment may well integrate FFR data (for instance, by proving that an effective hyperaemia has been reached independently of the dosing, administration path and vasodilator used). The assessment of CFR/IMR demonstrated here the failure to achieve maximal hyperaemia: in such cases, the possibility that the FFR data could be falsely negative should be raised and other tests (e.g., FFR with papaverine or dobutamine infusion or exercise echo-stress test) need to be performed. In the absence of CFR/IMR measurements, it can only be assumed that a sufficient hyperaemia can be obtained with the same drug in all patients and that this hyperaemia is reproducible over time. The present case shows that these assumptions should not be taken for granted.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Online data supplement
Moving image 1. First angiography.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1.




