In this issue of EuroIntervention, results from the long-awaited three-vessel-disease (3VD) subset of the CREDO-Kyoto PCI/CABG registry cohort-2 (CREDO-Kyoto registry) are published1. These findings were first presented at the European Society of Cardiology Congress in Paris, France, in August 2011, and were controversial. Although the registry was retrospective in nature, given its size, the results are difficult to ignore, particularly the apparent finding of CABG being “best” for 3VD in lower SYNTAX-score patients2.
Over a three-year period (2005-2007), 15,939 consecutive patients were enrolled in 26 centres in Japan, of whom 2,981 patients were identified with 3VD (PCI: n=1,825; CABG: n=1,156), and an impressive 2,812 patients (PCI: n=1,792; CABG: n=1,020) underwent retrospective SYNTAX score calculations. As expected, the adjusted primary endpoint of all-cause death, MI, or stroke was significantly lower in CABG-treated patients compared to PCI-treated patients, reflecting recent findings from the ASCERT registry3, and the randomised, all-comers SYNTAX trial4.
Interestingly, in the CREDO-Kyoto registry, unadjusted all-cause death was significantly greater for PCI compared to CABG (PCI: 11.7% vs. CABG: 9.3%, p=0.046), whereas unadjusted cardiac death was similar (PCI: 5.6% vs. CABG: 5.4%, p=0.41). Adjusted all-cause death (p=0.005) remained significantly in favour of CABG, whereas adjusted cardiac death remained neutral between CABG and PCI (p=0.28).
The results stratified by the presence of tertiles of the SYNTAX score in the CREDO-Kyoto registry are of additional interest, since the European revascularisation guidelines5 advocate that, for 3VD disease with a low SYNTAX score (0-22), PCI is given a class IIA recommendation (weight of evidence/opinion in favour of usefulness/efficacy). This recommendation is based primarily on the results of the SYNTAX trial4. Conversely, for 3VD associated with higher SYNTAX scores (>22), PCI is given a class III recommendation (not useful/effective and possibly harmful). Yet in the low SYNTAX score subset (0-22) of the CREDO-Kyoto study, the adjusted risk of the primary endpoint was higher for PCI compared to CABG (HR 1.66 [1.04-2.65], p=0.03), whereas the unadjusted risk of the primary endpoint was similar between CABG and PCI (HR 1.26 [0.86-1.925], p=0.24). Findings in the higher SYNTAX score tertiles were mixed, with only a high SYNTAX score (≥33) showing a trend towards treatment benefit for CABG compared to PCI on adjusted analyses (p=0.051). Given these contradictory findings, how is one to interpret them, particularly in the context of the current published evidence?
Interpreting the CREDO-Kyoto study
The main observation of the CREDO-KYOTO study is that the authors attempt to equalise the two treatment groups (CABG and PCI), through adjustment of data with simple clinical variables, and then undertake sensitivity analyses using propensity score matching to confirm the findings. What should be highlighted is that the authors endeavour to adjust an unadjustable characteristic, namely the clinical judgement and decision-making process of the Heart Team in selecting the most appropriate revascularisation modality6. As the authors appropriately highlight in the limitations section, selection bias due to unmeasured confounders, such as patient frailty, cognitive dysfunction, active malignancy, and systemic infection, could not be controlled for, and may offer an explanation why all-cause death was higher for PCI, whereas cardiac death was similar between CABG and PCI, even after adjustment for baseline factors.
Evidence to support these statements comes from the New York State registry6,7, in which survival after CABG or PCI was similar in unadjusted curves, but showed a mortality benefit favouring CABG after adjustment for risk factors (Figure 1). Excessive comorbidities make CABG less attractive due to the operative risk, which can be prohibitive. In such scenarios, PCI becomes the default approach. In the SYNTAX trial, these types of patients were not randomised, since CABG and PCI could not be offered equally, and they were therefore nested in a PCI registry (n=198). Strikingly, at five years, the nested PCI registry of the SYNTAX trial reported a mortality rate of 30%4. By comparison, in the randomised SYNTAX trial, five-year all-cause mortality was 11.4% in the CABG arm and 13.9% in the PCI arm (p=0.10). The reasons to explain the more than doubling of mortality in the PCI registry of the SYNTAX trial may be related to a greater occurrence of incomplete revascularisation due to severe anatomical complexity, and the associated negative impact on long-term survival8,9, high EuroSCORE subjects being shown to have an excess of mortality after PCI10,11, and the hypothesis12 that bypass grafts “protect” coronary vessels from future cardiac events for the lifespan of the graft, whereas PCI treats individual lesions –particularly in very high-risk subjects where the chances of a future clinical event are likely to be substantial.
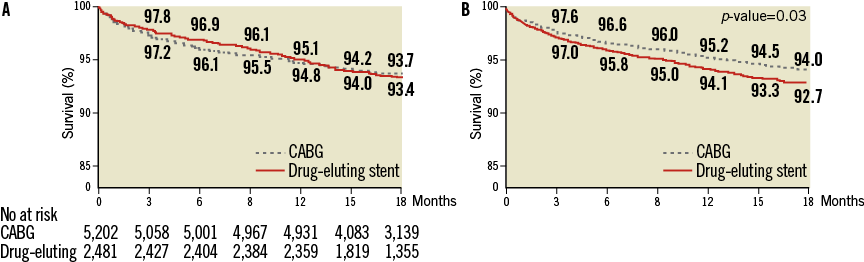
Figure 1. Unadjusted (A) and adjusted (B) Kaplan-Meier curves for survival from the New York State registry7. Adjusted survival curves (B) are for age, sex, ejection fraction, haemodynamic state, history or no history of myocardial infarction before the procedure, the presence or absence of cerebrovascular disease, peripheral arterial disease, congestive heart failure, chronic obstructive pulmonary disease, diabetes, renal failure, and involvement of the proximal left anterior descending artery. Reprinted with permission from Massachusetts Medical Society, Hannan et al7.
In the higher SYNTAX scores in the CREDO-Kyoto study, at least a trend for a treatment benefit of CABG was seen in the high SYNTAX score tertile (>32). This is likely to be related to the data being underpowered, confounded by selection bias as discussed.
SYNTAX score II
Recently, the SYNTAX score II was proposed and validated13, whereby the anatomical SYNTAX score was combined with clinical variables shown directly to affect decision making between CABG and PCI based on interactions (Figure 2). For example, the anatomical SYNTAX score aids decision making between CABG and PCI because it is more predictive of clinical outcomes in patients undergoing PCI, compared to patients undergoing CABG (where it is not predictive). Based on this principle, other factors were included in the SYNTAX score II, that were shown to alter the threshold value of the anatomical SYNTAX score that would lead to similar long-term mortality between CABG and PCI.
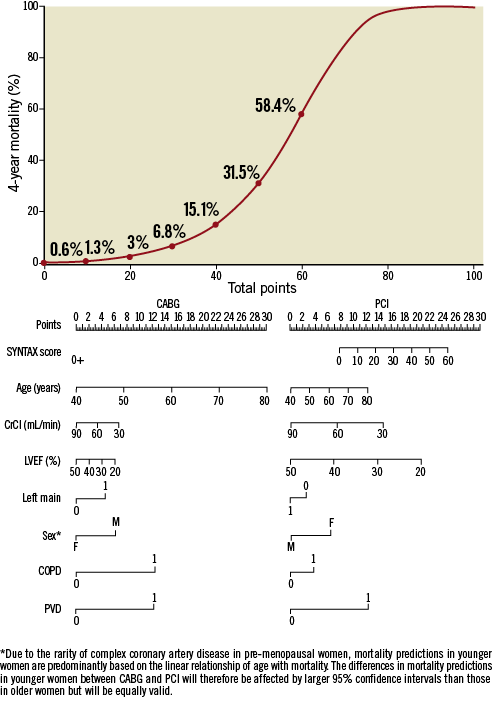
Figure 2. The SYNTAX score II nomogram for bedside application. Total number of points for 8 factors can be used for accurate prediction of 4-year mortality for the individual patient proposing to undergo CABG or PCI. Younger age, female gender and reduced LVEF favoured CABG compared to PCI on long-term prognostic grounds. Thus, in such patients a lower anatomical SYNTAX score would be required in order for the long-term mortality risk to be similar between CABG and PCI. By contrast, older age, chronic obstructive pulmonary disease or ULMCA disease favoured PCI compared to CABG. Thus, in this type of patient, a higher anatomical SYNTAX score would be needed for the long-term mortality risks to be similar. For example, a 60-year-old male with an anatomical SYNTAX score of 30, ULMCA disease, CrCl 60 ml/min, a LVEF of 50%, and COPD would have 41 points (predicted 4-year mortality: 16.3%) and 33 points (predicted 4-year mortality: 8.7%) to undergo CABG and PCI, respectively. The same example, without COPD included, would lead to identical points (29 points) and 4-year mortality predictions (6.3%) for CABG and PCI. Legend and image modified and reproduced with permission from Farooq et al11. CABG: coronary artery bypass graft surgery; PCI: percutaneous coronary intervention; CrCl: creatinine clearance (Cockcroft and Gault formula); LVEF: left ventricular ejection fraction; Left main: unprotected left main coronary artery disease; COPD: chronic obstructive pulmonary disease (long-term use of bronchodilators or steroids for lung disease [EuroSCORE definition]); PVD: peripheral vascular disease (aorta and arteries other than coronaries, with exercise-related claudication, and/or revascularisation surgery and/or reduced or absent pulsation and/or angiographic stenosis of more than 50%).
In essence, the SYNTAX score II adjusts the individual patient anatomical and clinical characteristics to aid objective decision making between CABG and PCI for the Heart Team. In addition, by individualising risk, the SYNTAX score II was shown to be able to identify higher and lower-risk subjects in all tertiles of the anatomical SYNTAX score who had a long-term mortality that favoured either CABG or PCI, or both revascularisation modalities. As compared to existing revascularisation guidelines using the conventional SYNTAX score, the selection of subjects based on a higher or lower expected survival using the SYNTAX score II was recently reported to be necessary only in approximately 110 patients in order to have one more patient alive at four years14.
Conclusion
What is required for validation of the effectiveness of the SYNTAX score and SYNTAX score II in decision making are prospectively run studies, or randomised validation studies, free from selection bias. Registry data, no matter how large, are confounded by (often appropriate) decision-making processes, and should therefore be interpreted with caution, as exemplified in the CREDO-Kyoto registry. The take-home message from the CREDO-Kyoto study is that the results actually appear to support current revascularisation guidelines, particularly with respect to the low SYNTAX score group, provided both anatomical and clinical factors are accounted for, as demonstrated in the SYNTAX score II.
Conflict of interest statement
The authors have no conflicts of interest to declare.