Published online Nov 25, 2015. doi: 10.4239/wjd.v6.i16.1312
Peer-review started: June 6, 2015
First decision: June 18, 2015
Revised: August 27, 2015
Accepted: September 29, 2015
Article in press: September 30, 2015
Published online: November 25, 2015
AIM: To design a medical cost calculator and show that diabetes care is beyond reach of the majority particularly patients with complications.
METHODS: Out-of-pocket expenditures of patients for medical treatment of type-2 diabetes were estimated based on price data collected in Benin, Burkina Faso, Guinea and Mali. A detailed protocol for realistic medical care of diabetes and its complications in the African context was defined. Care components were based on existing guidelines, published data and clinical experience. Prices were obtained in public and private health facilities. The cost calculator used Excel. The cost for basic management of uncomplicated diabetes was calculated per person and per year. Incremental costs were also computed per annum for chronic complications and per episode for acute complications.
RESULTS: Wide variations of estimated care costs were observed among countries and between the public and private healthcare system. The minimum estimated cost for the treatment of uncomplicated diabetes (in the public sector) would amount to 21%-34% of the country’s gross national income per capita, 26%-47% in the presence of retinopathy, and above 70% for nephropathy, the most expensive complication.
CONCLUSION: The study provided objective evidence for the exorbitant medical cost of diabetes considering that no medical insurance is available in the study countries. Although the calculator only estimates the cost of inaction, it is innovative and of interest for several stakeholders.
Core tip: The costs of medical treatment of diabetes are poorly documented in sub-Saharan Africa, while such data are of interest for several stakeholders and useful for advocacy. There is a lack of tools to make these estimations. We describe a standardized, innovative and user-friendly medical cost calculator and provide the results of its use in four countries. It was developed in West-Africa but it is also relevant for other African countries and perhaps even in Asia provided the standard treatment protocol is deemed appropriate.
- Citation: Alouki K, Delisle H, Besançon S, Baldé N, Sidibé-Traoré A, Drabo J, Djrolo F, Mbanya JC, Halimi S. Simple calculator to estimate the medical cost of diabetes in sub-Saharan Africa. World J Diabetes 2015; 6(16): 1312-1322
- URL: https://www.wjgnet.com/1948-9358/full/v6/i16/1312.htm
- DOI: https://dx.doi.org/10.4239/wjd.v6.i16.1312
Non-communicable diseases (NCDs) including diabetes pose a serious challenge to health systems already overstretched with acute and infectious diseases in Africa[1]. Following the High Level Meeting of the United Nations on NCDs in New-York in 2011[2], heads of governments made commitments towards prevention and control. However, the misconception that NCDs are diseases of the affluent is still widespread in low-income countries in spite of accumulating evidence against this myth. Strong advocacy is therefore required and the International Diabetes Federation (IDF), for instance, has developed a series of tools and guidelines to influence decision makers[3]. The following definition of advocacy is relevant for all health professionals[4]: “Blending science, ethics and politics, advocacy is self-initiated, evidence-based, strategic action that health professionals can take to help transform systems and improve the environments and policies which shape their patients’ behaviours and choices, and ultimately their health”. Simple and culture-sensitive advocacy tools are direly needed to foster the prevention and control of chronic diseases such as diabetes.
Several methods for identifying the economic consequences of diseases have been defined. Standard costs of diabetes in Africa, including the direct and indirect costs of the illness, have been estimated based on secondary data[5]. Such cost-of-illness (COI) studies, in addition to direct and indirect costs, may also include the intangible costs although these are seldom measured owing to the complexity of such measurements[6]. COI methods are simpler than, and very different from, the macro- and micro-economic models that have been developed to estimate the economic burden of the disease (cost of inaction) and the cost-effectiveness of action, such as CORE[7] and other Markov-based models, and WHO CHOICE[8]. Markov models are computer simulations of probabilistic progression of a disease in a hypothetical cohort which have been adapted to forecast mortality and complications of diabetes, as well as medical costs[9]. WHO CHOICE has been used to estimate the cost-effectiveness of interventions to combat chronic diseases, including diabetes, at the regional level, thereby assisting decision makers[10]. Comprehensive computer models of diabetes economic burden are many and they are in constant evolution[11,12]. However, such models are highly complex and ill-suited to the field.
As part of a university partnership project on the double burden of malnutrition in French-speaking West-Africa[1], diabetes advocacy instruments that are more specific to sub-Saharan African countries were developed. The principal tool was a simple medical cost calculator which is described and the results discussed in the present paper.
A Diabetes Advocacy Working Group was set up among the partnership project institutions, with members from Benin, Burkina Faso, Mali, Guinea and Canada (University of Montreal). The focus on diabetes, rather than obesity, was a strategic choice because obesity is not as yet commonly perceived as a health problem while diabetes certainly is.
The working group held regular sessions between 2009 and 2014. A medical cost calculator for diabetes treatment, in the absence or presence of complications, was designed. The team was inspired by the positive experience with PROFILES in the area of nutrition for advocating investments to eradicate malnutrition and micronutrient deficiencies[13]. The costing tool was applied after pretesting in the four West-African countries represented on the working group. A training workshop on diabetes advocacy with the introduction of this tool was held in Benin for members of the project’s institutional partners and for graduate students in health and nutrition.
The approach was based on COI, which is quite different from a cost-effectiveness approach[6,14]. In our study, the COI included only medical care from the patient perspective, that is, estimated individual, out-of-pocket expenditures. Medical cost estimates would also be relevant for third-party payers if and when health insurance becomes available. Other direct costs, for instance for transportation, are highly variable across individual patients and cannot be estimated in a standardized fashion. Although the instrument was based on the PROFILES conceptual model[13], only the first component was considered at the present stage, that is, the cost of the disease (cost of inaction), as there are as yet insufficient relevant data for Africa on the cost-effectiveness of primary prevention, screening and secondary prevention to also include the cost of action.
Prior to data collection on medical costs, a detailed protocol for the basic treatment of type-2 diabetes and for the treatment of main complications was developed by the working group. Components of care were listed under physicians and allied health professionals’ services, hospital care, lab tests and controls, and drugs and medical supplies, first for uncomplicated diabetes and then for each of the main acute and chronic complications. Acute complications included ketoacidosis, acute diabetic foot, kidney failure and stroke. Chronic complications were proliferative retinopathy, hypertension, nephropathy, cardiac ischemia, foot ulcer and the chronic phase of stroke. These complications were considered as the most common according to published data[15-19]. The treatment protocol was based on realistic medical care for uncomplicated and complicated diabetes in the African context, rather than on optimal care as may be available in high-income countries. The working group selected the components of care based on the latest IDF clinical guidelines[20], on IDF guidelines for Africa in 2006[21] taking account of needed update, as well as on a thorough literature review and on the clinical experience of endocrinologists of the group. Standards of care of the American Diabetes Association[22] were also examined for their relevance. The level of medical care was usually between “standard” and “minimal” as defined by IDF[20]. The care components as detailed for the basic treatment of uncomplicated type-2 diabetes and its complications are shown in Table 1. The frequency of medical check-ups, controls and tests is indicated, as well as drug posology. It will be noted that there are some alternatives, for instance, for hypoglycemic agents, as well as for drugs for complications. This is so because a cheaper alternative and a more expensive one are provided in order to estimate a range of medical costs instead of a single value such as the mean. Regarding tests, medical supplies, specialized treatments and drugs, two alternatives are also sometimes listed, a cheaper and a more expensive one.
| Medical conditions | Care component | Guidelines |
| Uncomplicated diabetes | ||
| Consultation of diabetes specialist or a general practitioner | 4/yr | |
| Fasting glucose test | 4/yr | |
| Urine glucose test | 6/yr | |
| Glycated hemoglobin | 2/yr | |
| Proteinuria test | 1/yr | |
| Blood lipid test TG, HDL-cholesterol, LDL-cholesterol | 1/yr | |
| Electrocardiogram | 1/yr | |
| Chest X-ray | 1/yr | |
| Ophthalmology consult | 1/yr | |
| Oral hypoglycemic agents | ||
| Glibenclamide 5 mg OR in combination with metformin | 3 tablets/d | |
| Metformin® 500 mg | 3 tablets/d | |
| Glucophage® 850 mg OR in combination with Amarel® | 3 tablets/d | |
| Amarel® 4 mg | 1 tablet/d | |
| For insulin users | ||
| Syringes | 1/wk (min)-1/d (max) | |
| Insulin | 30 UI (min) et 60 UI (max)/d | |
| Strips for blood glucose control | 1 strip/d (min) | |
| 3 strips/d (max) | ||
| Glucometer | 1 (Duration: 2 yr) | |
| Chronic complications | ||
| Proliferative retinopathy | ||
| Consultation in ophthalmology | 3/yr | |
| Retinography | 1/yr | |
| Laser photocoagulation | 1/yr | |
| Overt nephropathy | ||
| Consultation in nephrology | 2/yr | |
| Blood creatinine test | 2/yr | |
| Serum protein test | 2/yr | |
| Serum electrolytes test (sodium, potassium) | 2/yr | |
| Urinary electrolytes test (sodium, potassium) | 2/yr | |
| Urine creatinine test | 2/yr | |
| Proteinuria | 2/yr | |
| Hemogram | 2/yr | |
| Urine bacteriology | 4/yr | |
| Urine culture (ECBU) | 1/yr | |
| Antiplatelet drugs | ||
| Aspirin® 100 mg OR | 1 tablet/d | |
| Plavix® 75 mg | 1 tablet/d | |
| Antihypertensive (ARA2) | ||
| Valsartan® 80 mg | 1 tablet/d | |
| Diuretics: | ||
| Laxilix® 40 mg OR | 3 tablets/d | |
| Laxilix® special 500 mg | Half tablet/d | |
| Calcium carbonate (added to antiplatelet therapy, maximum cost) | 2 tablets/d | |
| Statin (added to antiplatelet therapy, maximum cost) | 1 tablet/d | |
| Renal failure | ||
| Dialysis | 2 session/wk | |
| Potex® 4000 UI (EPO) | 50 UI/kg weight (max) | |
| 2 sessions/wk | ||
| Calcium carbonate 500 mg | 1.5 g or 3 tablets/d (max) | |
| Ischemic heart disease | ||
| Consultation in cardiology | 2/an | |
| Antiplatelet drugs | See under nephropathy | |
| Statins | ||
| Simvastatin (Zocor®) OR | 1 tablet/d | |
| Atorvastatin (Tahor®) | 1 tablet/d | |
| Exercise electrocardiogram testing | 1/yr | |
| Echo doppler | 1/yr | |
| Cardiac ultrasound | 1/yr | |
| Coronarography | 1/yr | |
| Hypertension | ||
| Consultation in cardiology | 1/yr | |
| Antihypertensive drugs (ACEI) | ||
| Captopril® 25 mg OU | 3 tablets/d | |
| Ramipril® 5 mg | 1 tablet/d | |
| Diuretics | See under nephropathy | |
| Aggregation inhibitors | See under nephropathy | |
| Semi quantitative urine protein test | 2/yr | |
| Blood creatinine test | 2/yr | |
| Proteinemia | 2/yr | |
| Blood electrolytes test (Na, K, Ca) | 2/an | |
| Stroke (chronic phase) | ||
| Consultation in cardiology | 2/yr | |
| Antiplatelet drugs | See under nephropathy | |
| Diabetic foot | ||
| Consultation in podiatry | 1/yr | |
| Arteriography of the lower limbs | 1/yr | |
| Physiotherapy sessions | 10-20 sessions/yr | |
| Echo doppler | 1/yr | |
| Statins | See under ischemic heart disease | |
| Antiplatelet drugs | 1 tablet/d | |
| Orthopedic shoes | 2 pairs/yr | |
| Acute complications | ||
| Ketoacidosis | ||
| Hospitalization | 7 d | |
| Blood glucose test | Done once during hospitalization | |
| Glycated hemoglobin | Done once during hospitalization | |
| Hemogram | Done once during hospitalization | |
| Blood lipids test | Done once during hospitalization | |
| Blood electrolytes test (Na, K) | Done once during hospitalization | |
| Blood creatinine test | Done once during hospitalization | |
| Blood urea test | Done once during hospitalization | |
| Electrocardiogram | Done once during hospitalization | |
| Chest X- ray | Done once during hospitalization | |
| Echo doppler | Done once during hospitalization | |
| Keto-Diastix® box of 50 strips (blood biology) | 3 times/d for 3 d | |
| Perfusion | 3 d | |
| Diabetic foot (acute) | ||
| Hospitalization | 90 d | |
| Antibiotics | ||
| Oxaciline® 500 mg | 4 tablets/d | |
| 3 wk of treatment without bone involvement (min); 10 wk when bone involved (max) | ||
| Vasodilator: Vastarel® 35 mg | 2 tablets/d, 22 wk | |
| Biopsy | Done once during hospitalization | |
| Antibiogram | Done once during hospitalization | |
| Bone radiography | Done once during hospitalization | |
| Vascular ultrasound | Done once during hospitalization | |
| Dressings | 1/wk, 22 wk | |
| Foot surgery | ||
| Minor surgery (56%) | ||
| Major surgery, amputation (44%) | ||
| Prosthesis | ||
| End stage renal disease | ||
| Hospitalization | 30 d | |
| Ultrasound | Done once during hospitalization | |
| Electrolytes blood test (Na, K) | Done once during hospitalization | |
| Creatinine blood test | Done once during hospitalization | |
| Proteinemia | Done once during hospitalization | |
| Stroke | ||
| Hospitalization | 18 d | |
| Vasodilatator: Vastarel® 35 mg | 2 tablets/d, 18 d | |
| Anticoagulants | 1 tablet/d, 18 d | |
| Rehabilitation/physical therapy | 18 d | |
Diabetes care costs were computed from price data (in local currency) collected in hospitals, clinics and pharmacies of the targeted countries, and not on the basis of actual patients’ expenditures. Unit prices or rates for services and supplies were collected and entered in the tally forms designed for the purpose and including each care component previously identified. Prices were retrieved in public hospitals, private clinics, hospital pharmacies and private pharmacies of the capital city. The two hospitals included a university hospital (there is usually only one, serving as reference hospital) and a secondary hospital. Price data were also collected in two private clinics, including one offering specialized diabetes care if available. Prices for drugs and medical supplies were obtained in the pharmacies of the selected public hospitals and in two private pharmacies. Prices or rates were as charged to patients, irrespective of government subsidies that may exist in a given country. Forms for entering price data were designed (available from the corresponding author upon request). Unit costs were entered in the unshaded parts of the forms. If an element of care was only offered in one public hospital or only in one private clinic, the same price was entered for the other public or private structure. In public pharmacies, prices of available generic drugs were collected. If a given drug was only available in private pharmacies, the same price would be entered for the public pharmacies as well. The cost of drugs was to be entered for the number of units as generally packaged, but if the number was different, it had to be specified on the form. General and specific guidelines were developed to assist the users of the cost calculator in filling the forms.
A user-friendly software was designed on Excel 2010 for Windows with the assistance of a computer specialist in order to compute the medical costs of diabetes, in the absence or presence of complications. The estimated costs per individual are given as a range in the public and private health sector of a given country. It was hypothesized that incurred costs would be higher in the private healthcare sector and this was the rationale for collecting data in the public and private sectors. The cost data could be entered directly in the Excel software, but the algorithms could not be changed. They are quite complex as several assumptions and empirical solutions had to be made. For instance, in computing the annual cost of basic care in the absence of complications, an assumption had to be made regarding the proportion of subjects taking insulin since glucose monitoring regimen is different from those on oral hypoglycemic agents. It was estimated that roughly 20% of all patients were on insulin, based on clinical practice and published data[15]. Another example refers to dialysis. Some hospitals have a package rate, whereas others have a rate per session, with a separate charge for the catheter. For any care component, four prices were obtained; the software computed the range of cost per care item and for the total in the private and public sectors.
Based on the recommended frequency of “treatment” units, the total cost was computed per year and per individual for the medical cost of uncomplicated diabetes. Similarly, the additional annual cost for the treatment of chronic complications (one by one to prevent dual counting) was computed. For acute complications, the additional cost was calculated per episode. Costs were computed in local currency and they can then be converted automatically into Euros or United States dollars. The software provides the results in table and figure format. It is also possible to estimate with the software the total theoretical medical costs at country level, based on prevalence of diabetes and its main complications, but this is beyond the scope of the present paper (The software, which includes the spreadsheet for price data entry, is available from the corresponding author).
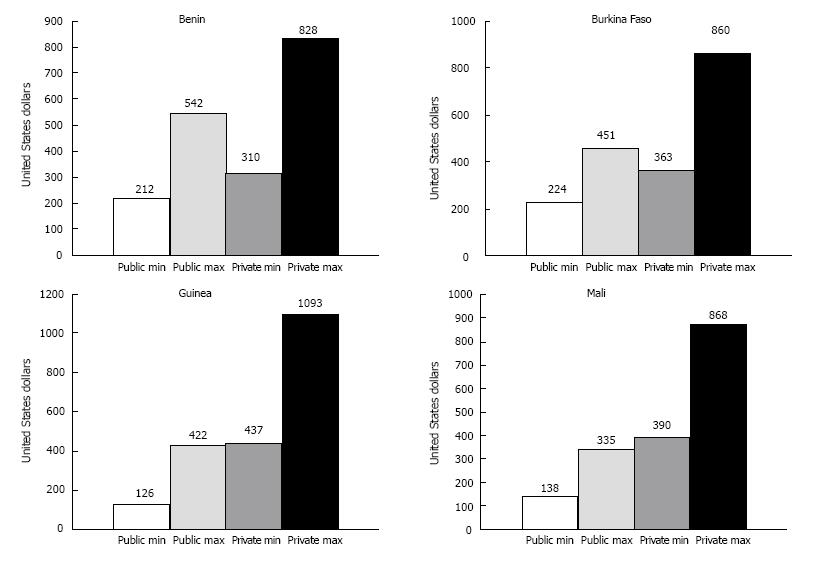
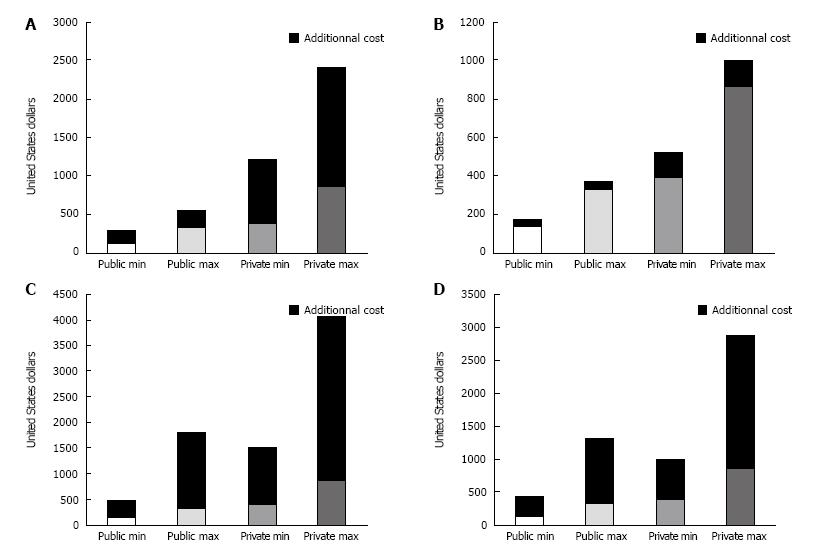
Individual medical costs for uncomplicated diabetes and additional costs associated with complications are shown in Table 2 for each study country (in United States dollars). Uncomplicated diabetes costs and chronic complication costs are given on an annual basis. Costs for acute complications include uncomplicated diabetes annual costs plus additional costs per episode of a given complication. Medical costs of uncomplicated diabetes ranged from 126 United States dollars to 1093 United States dollars in Guinea, 137 United States dollars to 869 United States dollars in Mali, 212 United States dollars to 828 United States dollars in Benin, and 224 United States dollars to 859 United States dollars in Burkina-Faso. Wide ranges were also observed within countries, with at least a twofold increase from the minimum to the maximum cost in the public healthcare system as well as in the private sector. The minimum cost in the public sector was lower by a factor of 4 to 8 than the maximum cost in the private sector in all countries. In the treatment of uncomplicated diabetes, drugs and medical supplies represented the highest cost share, ranging from 52% to 75%. Figure 1 illustrates the range of medical costs per person per year for uncomplicated diabetes, in the public and private healthcare systems and for each study country. The medical costs increased steadily from the public to the private sector, except in Benin and Burkina-Faso where the maximum medical cost in the public sector was higher than the minimum cost in the private sector. Figure 2 provides illustrated examples of the software outputs for incremental medical costs per person per year in the presence of one chronic complication, in this instance for Mali. It shows that except for retinopathy, the additional cost for treating complications represents at least twice the medical cost of basic diabetes care. Of all chronic complications considered, the most costly was nephropathy in all countries.
| Medical condition | Bénin | Burkina Faso | Guinea | Mali | ||||||||||||
| Public sector | Private sector | Public sector | Private sector | Public sector | Private sector | Public sector | Private sector | |||||||||
| Min | Max | Min | Max | Min | Max | Min | Max | Min | Max | Min | Max | Min | Max | Min | Max | |
| Uncomplicated diabetes | 212 | 542 | 310 | 828 | 224 | 451 | 363 | 859 | 126 | 422 | 437 | 1093 | 137 | 335 | 390 | 869 |
| Chronic complications - Basic medical cost for uncomplicated diabetes plus additional annual cost for single complication | ||||||||||||||||
| Retinopathy | 320 | 686 | 421 | 987 | 306 | 532 | 465 | 984 | 187 | 488 | 511 | 1243 | 177 | 374 | 524 | 1002 |
| Stroke | 233 | 576 | 672 | 1360 | 241 | 469 | 1644 | 2155 | 135 | 432 | 1267 | 1937 | 147 | 345 | 687 | 1850 |
| Nephropathy | 850 | 1920 | 1614 | 3198 | 783 | 1299 | 2578 | 3412 | 808 | 1578 | 2366 | 4256 | 491 | 1808 | 1516 | 4069 |
| Hypertension | 345 | 751 | 1256 | 2065 | 377 | 605 | 2074 | 2590 | 367 | 667 | 1784 | 2655 | 293 | 556 | 1212 | 2408 |
| Ischemic heart disease | 535 | 1297 | 1050 | 2188 | 496 | 785 | 1943 | 2577 | 313 | 612 | 1484 | 2553 | 441 | 1324 | 1002 | 2881 |
| Diabetic foot | 694 | 1533 | 1103 | 2386 | 923 | 1337 | 2447 | 4294 | 527 | 877 | 1717 | 3393 | 484 | 1424 | 1043 | 3172 |
| Acute complications - Basic annual medical cost for uncomplicated diabetes plus additional cost per episode of acute complication | ||||||||||||||||
| Keto acidosis | 406 | 802 | 576 | 1297 | 387 | 665 | 1036 | 1936 | 222 | 531 | 726 | 1758 | 243 | 463 | 606 | 1391 |
| Infected diabetic foot requiring hospitalization | 728 | 1539 | 1020 | 3860 | 729 | 1702 | 6886 | 12043 | 667 | 1129 | 2897 | 6679 | 698 | 1340 | 1709 | 5802 |
| Stroke (acute phase) | 637 | 1117 | 834 | 1935 | 576 | 1064 | 2316 | 4147 | 510 | 933 | 1427 | 3315 | 455 | 705 | 1003 | 2266 |
Table 3 shows for each study country the estimated cost range in current United States dollars and in percentage of gross national income (GNI) per capita (http://wdi.worldbank.org/table/1.1) and of an economic poverty threshold (2$ per day or 730$ a year according to the World Bank[23]) for uncomplicated diabetes, for diabetes with retinopathy, the complication with the lowest incremental cost, and for diabetes with nephropathy which entails the highest additional cost. GNI per capita in current United States dollars 2013 ranged from 460$ in Guinea to 790$ in Benin. Uncomplicated diabetes cost amounted to a minimum of 21%-34% of the GNI, with a maximum reaching 238% in Guinea. With chronic complications, the share of the GNI soared. The minimum cost of diabetes with nephropathy represented 73%-176% of the GNI. The medical costs of diabetes without complications ranged from 17.2% to 150% of the annual income corresponding to the poverty line. With retinopathy, the least costly complication, medical costs varied from 24.2% in Mali to 170% in Guinea. For nephropathy, the most costly complication, medical costs amounted to at least 67% of the annual poverty line.
| Countries | Mali | Benin | Burkina Faso | Guinea | |
| GNI per capita (2013) | 670 | 790 | 670 | 460 | |
| % of population with < $2/d (= $730/yr) | 78.7 | 74.3 | 72.6 | 72.7 | |
| Uncomplicated diabetes | |||||
| Minimum cost | 137.21 | 211.63 | 224.42 | 125.58 | |
| Maximum cost | 868.60 | 827.91 | 859.30 | 1093.02 | |
| % of GNI (% of poverty threshold1) | |||||
| Minimum | 20.5 (18.7) | 26.8 (28.9) | 33.5 (30.7) | 27.3 (17.2) | |
| Maximum | 129.6 (118.9) | 104.8 (113.4) | 128.3 (117.6) | 237.6 (149.7) | |
| Diabetes + retinopathy | |||||
| Minimum cost | 176.74 | 320.93 | 305.81 | 187.21 | |
| Maximum cost | 1002.33 | 987.21 | 983.84 | 1243.02 | |
| % of GNI (% of poverty threshold) | |||||
| Minimum | 26.4 (24.2) | 40.6 (43.9) | 45.6 (41.9) | 46.8 (25.6) | |
| Maximum | 149.6 (137.3) | 125.0 (135.2) | 141.6 (134.7) | 270.2 (170.3) | |
| Diabetes + nephropathy | |||||
| Minimum cost | 490.70 | 850.00 | 782.56 | 808.14 | |
| Maximum cost | 4068.60 | 3197.67 | 3411.63 | 4256.98 | |
| % of GNI (% of poverty threshold) | |||||
| Minimum | 73.2 (67.2) | 107.6 (116.4) | 116.8 (107.2) | 175.7 (110.7) | |
| Maximum | 607.3 (557.3) | 404.8 (438.0) | 509.2 (467.3) | 925.4 (583.1) | |
The aim of this study was to develop and test a simple medical cost calculator for diabetes to be used primarily for advocacy purposes. Research evidence is not consistently used for policy formulation[24], even by international organizations[25]. Demonstration of unbearable economic and human costs of a chronic disease such as diabetes may be regarded as concrete and therefore more promising as a means to influencing decision makers. While considerations other than financial, whether political or other, are at play, economic arguments are important even if not sufficient by themselves to induce changes in public policy and programmes[26]. Furthermore, figures are compelling for decision-makers who have to address competing priorities. Cost indeed plays a critical role in decision making regarding health, in any country.
What the study showed is that the medical cost calculator was quite user-friendly and that collecting country-specific price data was highly relevant, considering the wide differences observed across countries in estimated medical costs of uncomplicated and complicated diabetes. The country-specific cost data collected using this instrument could actually be used to update regional estimates that are needed for macroeconomic models. The diabetes cost calculator is certainly not intended as a substitute for highly technical and validated models such as CORE[7] and WHO-CHOICE[8]. However, their use is constrained by their complexity, the global scale of the figures, and the numerous assumptions underlying the calculations. Expertise is required to manipulate and adjust the models. Furthermore, since data on local effectiveness of interventions are scanty, particularly in Africa, assumptions have to be made. The costing tool was designed so as to remain simple in order to encourage its use at country level. The participants of the advocacy training workshop during which the calculator was presented indeed felt that the instrument was transparent and easy to use, but at the present time, we have no feedback on the effective use of the calculator for advocacy purposes.
The results confirmed that medical costs vary considerably between the private and public healthcare systems and even within each sector. Similarly, in India, direct costs were nearly four times higher in Chennai than in Delhi, illustrating wide variations within a country[6]. Providing ranges of medical costs was considered more representative than means. Medical costs in other hospitals, clinics and pharmacies of the country would most likely fall within the computed range. Additionally, in order to compute means that would be representative of a whole country’s medical costs, the process would be much heavier and expensive, with the need for a large number of randomly selected health facilities to include in the study. The cost calculator also allows to better size up the medical cost discrepancies between the private and public sector. Public subsidies on drugs, hospitalization and other treatment components were not taken into account and likely contribute to these discrepancies among countries and between the private and public sector, for example in Benin, where the government gives subsidies for dialysis and for hospitalization. Additionally, costs for drugs will depend on the type of molecules and on whether or not generic formulations are available. The specific guidelines provided with the cost calculator regarding the type of drugs to consider (available on demand) contribute to standardize as much as possible cost data compilation.
The costing tool that we developed is the first of its kind and there is no equivalent in the published literature, where only out-of-pocket expenditures based on patients’ surveys are to be found. The cost calculator refers to a standardized medical care protocol so that costs can be compared across countries. The tool is flexible in that prices can be updated as required in the Excel file, with automatic adjustment of the outputs (tables and graphs). This allows for the tool to be updated whenever new data become available. However the treatment components cannot be modified in the software in order to allow comparisons.
The estimated total medical cost for the basic treatment of diabetes at the individual level in a given country using this standard procedure may be of value to health professionals, governments and other potential payers such as insurance companies in many ways. Firstly and of foremost importance, the burden of the expenses that households or individuals would have to incur for basic care of uncomplicated diabetes can be appraised based on income levels and income distribution in the country, where such data are available. In the absence of recent household budget surveys, a basis for comparison could be the country’s minimum wage, the GNI per capita, or else an economic poverty threshold, as was done in the present study. This may allow to clearly show that several patients are not minimally treated because they simply cannot afford the medical follow-ups and even the drugs, in the absence of government subsidies or insurance (or even when these are available). These cost data may therefore represent in themselves powerful advocacy arguments. In Cameroon, a study on out-of-pocket expenditures of more than 350 diabetes patients revealed that monthly medical costs reached 148$ United States in 2009-2011 (89.40$ for medicines, 10.40$ for consults, 35.0$ for tests, and 13.20$ for glycemia monitoring), which amounted to more than twice the minimum wage[27]. According to the present study, basic treatment cost range of uncomplicated diabetes would represent 27%-105% of GNI per capita in Benin, 21%-130% of GNI in Mali, 27%-238% in Guinea, and in Burkina, where the minimum estimated cost was the highest of the four countries, from 34% to 138%. Actual expenditures of patients probably lie somewhere in-between the minimum and the maximum. Analysis of data from a survey of several hundred individuals living with diabetes in Mali showed that annual medical expenditures of subjects free from complications were within the range of estimated costs using the calculator, at least in the public sector (unpublished data). A study on the economic burden of diabetes in Africa[5] showed that average medical costs (including the same components as the present study) represented 36% of GNI for countries with a GNI lower than 2000$ United States, which includes all four countries of the present study. Furthermore, this is the basic cost only. Treatment costs soared when diabetes complications are present, which is the case for a majority of persons living with diabetes -70% according to the survey in Mali[28]. In India, the cost-ratio for those having complications vs those without was around 2.0[6]. In our study, for instance, the treatment of nephropathy, considering only the minimum cost in the public sector, would more than treble the yearly basic cost, ranging from a factor of 3.5 in Burkina Faso to 6 in Guinea. A few studies have shown that the cost of diabetes is indeed beyond reach of a sizeable proportion of the population. In Côte d’Ivoire, for instance, 35% to 55% of the household income would have to be spent for diabetes care[29]. In Mali, it was estimated that for insulin only, households with a diabetic member spent 38% of their total income[30]. This confirms that acceptable diabetes care is likely unaffordable to most. In our study, we used the GNI per capita as a proxy of income, as well as the World Bank poverty threshold of 2$/d (or 730$/year). It is noteworthy that the GNI per capita itself is below this poverty threshold in three of the four study countries. Roughly 75% of the population of these countries lives with less than 2$/d, which betrays rampant poverty. It is therefore likely that a good majority of the people would not afford even the most basic medical treatment of type-2 diabetes. The diabetes cost calculator provides for an estimation of minimum incurred medical expenses as a percentage of income proxy without having to conduct lengthy and expensive surveys for that purpose. Furthermore, demonstrating the cost increment associated with complications related to a late diagnosis may help convince decision-makers to make the screening more efficient at primary health care level. Comparing the medical costs of diabetes in neighbouring countries may also be of interest for policy purposes, even if only the cost of the disease is computed at this stage.
There are obviously several limitations to this costing tool. Only direct medical costs are estimated, on the basis of diabetes treatment component price data collected locally in public and private care institutions. Other direct costs incurred by families, such as transportation, traditional medicine, time of the care-provider and extra-expenditures for the diet are not taken into account and besides, these can hardly be standardized. However, according to other studies on actual expenditures, direct costs tend to be higher than indirect costs[6].
Although the treatment protocol was considered realistic for Africa, all included elements of care may not be absolutely necessarily in spite of their relevance. For instance, some could argue that care may be acceptable even if some costly tests are not performed. Moreover, although consensus was required in the working group to define the treatment components, some arbitrariness was unavoidable, whether in the frequency of medical visits or in medicine posology.
The cost calculator does not include either the indirect costs to the health system (salaries and training of health personnel; health facilities; subsidies, etc.), the families and the society as a whole (loss of productivity, of income, of healthy life years...). The medical costs estimated with the calculator represent only a fraction of the total economic burden of the disease.
A useful addition to the costing tool would be to estimate cost-effectiveness of interventions for primary prevention among high-risk individuals, combined with secondary prevention among diagnosed individuals, in order to demonstrate the savings that may accrue from earlier detection and treatment of diabetes, using the costing tool. However, there are no cost-effectiveness data that are relevant for Africa and the only controlled interventions in low- and middle-income countries were conducted in India[31] and China[32]. Additionally, cost-effectiveness analyses do not take into account non-health benefits, such as income gains, which may be important[33].
In conclusion, the study confirms in an objective and standardized fashion that the basic medical cost of diabetes is likely beyond reach of a majority of people in West-African countries considering that no medical insurance is available in most of them. In spite of its limitations, the medical cost calculator, which can be used in different countries, is deemed important in Africa, considering the paucity of data on diabetes cost in the whole region. It is also flexible enough since cost data can easily be changed. No study had so far designed a simple costing tool which would take into account the various components of medical care of diabetes and its complications in sub-Saharan Africa.
The authors thank Mr Stéphane Proulx for software development, Drs. Adébayo Alassani (Benin), Joseph Samah (Guinea) and Alexandre Zoungrana (Burkina-Faso) for their support in price data collection, and Pr Amédégnato Degno and Dr. Denis Agbétiafa for pretesting the calculator in Togo.
Non-communicable chronic diseases such as diabetes are taking a heavy social and economic toll in low income countries already overburdened by acute diseases. However, diabetes remains far from the top of health priorities in most of sub-Saharan Africa. In addition to global calls for action, specific advocacy strategies and instruments are therefore timely. The study describes a standardized calculator that was developed to estimate the medical costs of diabetes in sub-Saharan Africa. Showing the exorbitant cost of inaction is regarded as potentially convincing for decision makers.
Economic models of diabetes and other chronic diseases exist but their complexity is a serious barrier to their wider use notably for advocacy purposes. The development and testing of simple yet standardized estimators of medical costs of diabetes (and other chronic diseases) is a relevant research area for low- and middle-income countries who now face a staggering escalation of chronic diseases.
Previous studies on this topic in Africa focused on medical costs of acute complications in the hospital or of specific care components such as insulin treatment, whereas this study included all direct medical costs for basic treatment and for the treatment of chronic and acute complications. To develop the medical cost calculator, a detailed protocol for the basic treatment of type-2 diabetes and for the treatment of main complications was first developed by a working group consisting of medical and public health specialists from the four West African study countries. Care components for minimally adequate treatment included physicians and allied health professionals’ services, hospital care, lab tests and controls, and drugs and medical supplies. Price data for the care components were then collected in the public and private health sectors of the study countries. The user-friendly software designed on Excel 2010 for Windows allows to compute ranges of total medical costs for patients. Total yearly medical costs for a person with diabetes convincingly show that the treatment is unaffordable for many, particularly when taking into account local incomes and if complications are present, which is the case for a majority of patients.
The medical costs calculator developed in the study can be used in other African countries since the treatment protocol is standardized; only local prices vary. This tool can be used by health professionals or other stakeholders for advocacy so that action is taken for type 2 diabetes prevention and control. The calculator allows to show the prohibitive cost of inaction vis-à-vis type 2 diabetes, whether at the individual or country level. The tool would have to be complemented with data on alternative interventions in order to show the cost of action.
Direct medical costs of diabetes: The calculator provides an estimate of out-of-pocket expenditures of patients with diabetes for their treatment in the study countries of West Africa. Other direct costs (transportation, diet...) are not included. Gross national income (GNI) per capita: This figure is often used as a proxy for income, as done in the study countries. The GNI is converted to international dollars using purchasing power parity rates. An international dollar has the same purchasing power as a United States dollar in the United States.
The authors describe a tool that is a simple medical cost calculator; they report and discuss the results of this tool. The manuscript is well written and well organized.
P- Reviewer: Beltowski J, Masaki T, Traub M, Verrotti A S- Editor: Gong XM L- Editor: A E- Editor: Lu YJ
| 1. | Lefebvre P. La pandémie de diabète: un fléau cardiovasculaire et une menace pour les systèmes de santé et l’économie mondiale. Médecine des Maladies Métaboliques. 2008;2:169-179. [Cited in This Article: ] |
| 2. | United Nations . Political declaration of the High-level Meeting of the General Assembly on the prevention and control of non-communicable diseases. 2011;. [Cited in This Article: ] |
| 3. | International Diabetes Federation. Adovacy and policy. Resources and tools. Available from: http: //www.idf.org/resources-and-tools. [Cited in This Article: ] |
| 4. | International Council of Nurses. Promoting health. Advocacy guide for health professionals. Geneva: ICN 2008; . [Cited in This Article: ] |
| 5. | Kirigia JM, Sambo HB, Sambo LG, Barry SP. Economic burden of diabetes mellitus in the WHO African region. BMC Int Health Hum Rights. 2009;9:6. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 72] [Cited by in F6Publishing: 89] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 6. | Ng CS, Lee JY, Toh MP, Ko Y. Cost-of-illness studies of diabetes mellitus: a systematic review. Diabetes Res Clin Pract. 2014;105:151-163. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 75] [Cited by in F6Publishing: 78] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 7. | Palmer AJ, Roze S, Valentine WJ, Minshall ME, Foos V, Lurati FM, Lammert M, Spinas GA. The CORE Diabetes Model: Projecting long-term clinical outcomes, costs and cost-effectiveness of interventions in diabetes mellitus (types 1 and 2) to support clinical and reimbursement decision-making. Curr Med Res Opin. 2004;20 Suppl 1:S5-26. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 360] [Cited by in F6Publishing: 372] [Article Influence: 18.6] [Reference Citation Analysis (0)] |
| 8. | World Health Organization. Cost effectiveness and strategic planning (WHO-CHOICE). Available from: http://www.who.int/choice. [Cited in This Article: ] |
| 9. | González JC, Walker JH, Einarson TR. Cost-of-illness study of type 2 diabetes mellitus in Colombia. Rev Panam Salud Publica. 2009;26:55-63. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 29] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 10. | Ortegón M, Lim S, Chisholm D, Mendis S. Cost effectiveness of strategies to combat cardiovascular disease, diabetes, and tobacco use in sub-Saharan Africa and South East Asia: mathematical modelling study. BMJ. 2012;344:e607. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 59] [Cited by in F6Publishing: 68] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 11. | Zhou H, Isaman DJ, Messinger S, Brown MB, Klein R, Brandle M, Herman WH. A computer simulation model of diabetes progression, quality of life, and cost. Diabetes Care. 2005;28:2856-2863. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 81] [Cited by in F6Publishing: 83] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 12. | Mount Hood 4 Modeling Group. Computer modeling of diabetes and its complications: a report on the Fourth Mount Hood Challenge Meeting. Diabetes Care. 2007;30:1638-1646. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 165] [Cited by in F6Publishing: 174] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 13. | Burkhalter BR, Abel E, Aguayo V, Diene SM, Parlato MB, Ross JS. Nutrition advocacy and national development: the PROFILES programme and its application. Bull World Health Organ. 1999;77:407-415. [PubMed] [Cited in This Article: ] |
| 14. | Bloom DE, Cafiero ET, Jané-Llopis E, Abrahams-Gessel S, Bloom LR, Fatima S. The global economic burden of non-communicable diseases. Switzerland: Geneva World Economic Forum 2011; . [Cited in This Article: ] |
| 15. | Sobngwi E, Ndour-Mbaye M, Boateng KA, Ramaiya KL, Njenga EW, Diop SN, Mbanya JC, Ohwovoriole AE. Type 2 diabetes control and complications in specialised diabetes care centres of six sub-Saharan African countries: the Diabcare Africa study. Diabetes Res Clin Pract. 2012;95:30-36. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 76] [Cited by in F6Publishing: 57] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 16. | Mbanya JC, Sobngwi E. Diabetes in Africa. Diabetes microvascular and macrovascular disease in Africa. J Cardiovasc Risk. 2003;10:97-102. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 35] [Reference Citation Analysis (0)] |
| 17. | Mbanya JC, Motala AA, Sobngwi E, Assah FK, Enoru ST. Diabetes in sub-Saharan Africa. Lancet. 2010;375:2254-2266. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 415] [Cited by in F6Publishing: 417] [Article Influence: 29.8] [Reference Citation Analysis (0)] |
| 18. | Hall V, Thomsen RW, Henriksen O, Lohse N. Diabetes in Sub Saharan Africa 1999-2011: epidemiology and public health implications. A systematic review. BMC Public Health. 2011;11:564. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 301] [Cited by in F6Publishing: 353] [Article Influence: 27.2] [Reference Citation Analysis (0)] |
| 19. | Kengne AP, Amoah AG, Mbanya JC. Cardiovascular complications of diabetes mellitus in sub-Saharan Africa. Circulation. 2005;112:3592-3601. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 98] [Cited by in F6Publishing: 123] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 20. | International Diabetes Federation. Clinical Guidelines Task Force. Global guidance for type 2 diabetes. : International Diabetes Federation 2012; . [Cited in This Article: ] |
| 21. | International Diabetes Federation. Guide de prise en charge du diabète de type 2 pour l’Afrique sub-saharienne. : International Diabetes Federation 2006; . [Cited in This Article: ] |
| 22. | American Diabetes Association. Executive summary: standards of medical care in diabetes--2011. Diabetes Care. 2011;34 Suppl 1:S4-10. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 64] [Cited by in F6Publishing: 118] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 23. | World Bank. Ratio de la population pauvre disposant de moins de $ 2 par jour (% de la population) (Internet). Available from: http: //data.worldbank.org/indicator/SI.POV.2DAY. [Cited in This Article: ] |
| 24. | Prewitt K, Schwandt TA, Straf ML. Using science as evidence in public policy. Washington, DC: The National Academies Press 2012; . [Cited in This Article: ] |
| 25. | Hoffman SJ, Lavis JN, Bennett S. The Use of Research Evidence in Two International Organizations‘ Recommendations about Health Systems. Healthc Policy. 2009;5:66-86. [PubMed] [Cited in This Article: ] |
| 26. | Bowman S, Unwin N, Critchley J, Capewell S, Husseini A, Maziak W, Zaman S, Ben Romdhane H, Fouad F, Phillimore P. Use of evidence to support healthy public policy: a policy effectiveness-feasibility loop. Bull World Health Organ. 2012;90:847-853. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 24] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 27. | Ngassam E, Nguewa JL, Ongnessek S, Foulko A, Mendane F. Coût de la prise en charge du diabète de type 2 à l’Hôpital Central de Yaoundé. Diabetes Metab. 2012;38:n° S2. [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 28. | Brown JB, Ramaiya K, Besançon S, Rheeder P, Tassou CM, Mbanya JC, Kissimova-Skarbek K, Njenga EW, Muchemi EW, Wanjiru HK, Schneider E. Use of medical services and medicines attributable to diabetes in Sub-Saharan Africa. PLoS One. 2014;9:e106716. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 29. | Ankotche A, Binan Y, Leye A. Graves conséquences du coût financier du diabète sur sa prise en charge, en dehors des complications, en Afrique sub-saharienne: l’exemple de la Côte-d’Ivoire. Médecine des Maladies Métaboliques. 2009;3:100-105. [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 30. | Labie D. [Diabetes care in sub-Saharan Africa]. Med Sci (Paris). 2007;23:320-322. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 31. | Ramachandran A, Snehalatha C, Mary S, Mukesh B, Bhaskar AD, Vijay V. The Indian Diabetes Prevention Programme shows that lifestyle modification and metformin prevent type 2 diabetes in Asian Indian subjects with impaired glucose tolerance (IDPP-1). Diabetologia. 2006;49:289-297. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1219] [Cited by in F6Publishing: 1141] [Article Influence: 63.4] [Reference Citation Analysis (0)] |
| 32. | Li G, Zhang P, Wang J, Gregg EW, Yang W, Gong Q, Li H, Li H, Jiang Y, An Y. The long-term effect of lifestyle interventions to prevent diabetes in the China Da Qing Diabetes Prevention Study: a 20-year follow-up study. Lancet. 2008;371:1783-1789. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1074] [Cited by in F6Publishing: 1004] [Article Influence: 62.8] [Reference Citation Analysis (0)] |
| 33. | Weatherly H, Drummond M, Claxton K, Cookson R, Ferguson B, Godfrey C, Rice N, Sculpher M, Sowden A. Methods for assessing the cost-effectiveness of public health interventions: key challenges and recommendations. Health Policy. 2009;93:85-92. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 181] [Cited by in F6Publishing: 195] [Article Influence: 13.0] [Reference Citation Analysis (0)] |